Abstract
The era of reduced-intensity allogeneic stem cell transplantation, with its emphasis on older patients, has created new challenges in the management of what is now an older related stem cell donor population. These donors are now on average no less than 10 years older than in the mid-1990s. Donors over 70 years of age are no longer isolated or exceptional cases. They may still be considered eligible for donation but many of them, based on the older age and their medical history, may no longer fully qualify as ‘healthy’ or ‘normal’. The older the donor, the more likely that hematologic abnormalities, comorbidities and treated malignancies will complicate the picture. Assessing the risk-benefit ratio for both donor and recipient can now be more challenging than ever.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Pasquini MC, Zhu X Current use and outcome of hematopoietic stem cell transplantation: CIBMTR Summary Slides, 2015. Available at: http://www.cibmtr.org (last accessed 18 March 2016).
Artz AS . Older patients/older donors: choose wisely. Hematology (Am Soc Hematol Educ Program) 2013; 2013: 70–75.
Pulsipher MA, Logan BR, Kiefer DM, Chitphakdithai P, Switzer GE, Riches ML et al. Related PBSC donors experience higher levels of pain and donation-related symptoms and less complete rates of recovery compared to unrelated donors: primary analysis of the Related Donor Safety Study (RDSafe). Biol Blood Marrow Transplant 2015; 21 (Suppl.): S41–S42.
Pulsipher MA, Chitphakdithai P, Logan BL, Switzer GE, Tomblyn MR, Rizzo JD et al. Related PBSC donors age >60 have higher rates of baseline and donation-related pain and slow recovery: first report from the Related Donor Safety Study (RDSafe). Biol Blood Marrow Transplant 2014; 20 (Suppl.):S41–S42.
Pulsipher MA, Switzer GA RDSafe: A multi-institutional study of HSC donor safety and quality of life. Available at: http://grantome.com/grant/NIH/R01-HL085707-04 (last accessed 15 March 2016).
Anderlini P, Rizzo JD, Nugent ML, Schmitz N, Champlin RE, Horowitz MM . Peripheral blood stem cell donation: an analysis from the International Bone Marrow Transplant Registry (IBMTR) and European Group for Blood and Marrow Transplant (EBMT) databases. Bone Marrow Transplant 2001; 27: 689–692.
Why a donor’s age matters. Available at: https://bethematch.org/transplant-basics/matching-patients-with-donors/why-donor-age-matters/ (last accessed 15 March 2016).
Anderlini P, Wu J, Gersten I, Ewell M, Tolar J, Antin JH et al. Cyclophosphamide conditioning in patients with severe aplastic anaemia given unrelated marrow transplantation: a phase 1–2 dose de-escalation study. Lancet Haematol 2015; 2: e367–e375.
Schultz KR . Is any donor too old? Biol Blood Marrow Transplant 2015; 21: 2–3.
de la Rubia J, Arbona C, de Arriba, del Caňizo C, Brunet S, Zamora C et al. Analysis of factors associated with low peripheral blood progenitor cell collection in normal donors. Transfusion 2002; 42: 4–9.
Vasu S, Leitman SF, Tisdale JF, Hsieh MM, Childs RW, Barrett AJ et al. Donor demographics and laboratory predictors of allogeneic peripheral blood stem cell mobilization in an ethnically diverse population. Blood 2008; 112: 2092–2100.
Richa E, Papari M, Allen J, Martinez G, Wickrema A, Anastasi J et al. Older age but not donor health impairs allogeneic granulocyte colony-stimulating factor (G-CSF) peripheral blood stem cell mobilization. Biol Blood Marrow Transplant 2009; 15: 1394–1399.
Anderlini P, Przepiorka D, Seong C, Smith TL, Huh YO, Lauppe J et al. Factors affecting mobilization of CD34+ cells in normal donors treated with filgrastim. Transfusion 1997; 37: 507–512.
Xing Z, Ryan MA, Daria D, Nattamai KJ, Van Zant G, Wang L et al. Increased hematopoietic stem cell mobilization in aged mice. Blood 2006; 108: 2190–2197.
Farrell TL, McGuire TR, Bilek LD, Brusnahan SK, Jackson JD, Lane JT et al. Changes in the frequencies of human hematopoietic stem and progenitor cells with age and site. Exp Hematol 2014; 42: 146–154.
Waterstrat A, Van Zant G . Effects of aging on hematopoietic stem and progenitor cells. Curr Opin Immunol 2009; 21: 408–413.
Chen J . Hematopoietic stem cell development, aging and functional failure. Int J Hematol 2011; 94: 3–10.
Gattillo S, Marktel S, Rizzo L, Malato S, Malabarba L, Coppola M et al. Plerixafor on demand in ten healthy family donors as a rescue strategy to achieve an adequate graft for stem cell transplantation. Transfusion 2015; 55: 1993–2000.
Snoeck HW . Aging of the hematopoietic system. Curr Opin Hematol 2013; 20: 355–361.
Champion KM, Gilbert JG, Asimakopoulos FA, Hinshelwood S, Green AR . Clonal haemopoiesis in normal elderly women: implications for the myeloproliferative disorders and myelodysplastic syndromes. Br J Haematol 1997; 97: 920–926.
Jaiswal S, Fontanillas P, Flannick J, Manning A, Grauman PV, Mar BG et al. Age-related clonal hematopoiesis associated with adverse outcomes. N Engl J Med 2014; 371: 2488–2498.
Busque L, Patel JP, Figueroa ME, Vasanthakumar A, Provost S, Hamilou Z et al. Recurrent somatic TET2 mutations in normal elderly individuals. Nat Genet 2012; 44: 1179–1181.
Xie M, Lu C, Wang J, McLellan MD, Johnson KJ, Wendl MC et al. Age-related mutations associated with clonal hematopoietic expansion and malignancies. Nat Med 2014; 20: 1472–1478.
Malcovati L, Cazzola M . The shadowlands of MDS: idiopathic cytopenias of undetermined significance (ICUS) and clonal hematopoiesis of indeterminate potential (CHIP). Hematology Am Soc Hematol Educ Program 2015; 2015: 299–307.
Townsley DM, Dumitriu B, Young NS . Bone marrow failure and the telomeropathies. Blood 2014; 124: 2775–2783.
Ju Z, Zhang J, Gao Y, Cheng T . Telomere dysfunction and cell cycle checkpoints in hematopoietic stem cells. Int J Hematol 2011; 94: 33–43.
Kyle RA, Therneau TM, Rajkumar SV, Offord JR, Larson DR, Plevak MF et al. A long-term study of prognosis in monoclonal gammopathy of undetermined significance. N Engl J Med 2002; 346: 564–569.
Therneau TM, Kyle RA, Melton LJ 3rd, Larson DR, Benson JT, Colby CL et al. Incidence of monoclonal gammopathy of undetermined significance and estimation of duration before first clinical recognition. Mayo Clin Proc 2012; 87: 1071–1079.
Greipp P . Progression risk for MGUS and SMM. Blood 2007; 100: 2226.
Turesson I, Kovalchik SA, Pfeiffer RM, Kristinsson SY, Goldin LR, Drayson MT et al. Monoclonal gammopathy of undetermined significance and risk of lymphoid and myeloid malignancies: 728 cases followed up to 30 years in Sweden. Blood 2014; 123: 338–345.
Shim YK, Rachel JM, Ghia P, Boren J, Abbasi F, Dagklis A et al. Monoclonal B-cell lymphocytosis in healthy blood donors: an unexpectedly common finding. Blood 2014; 123: 1319–1326.
Stetler-Stevenson M . Monoclonal B-cell lymphocytosis in donors. Blood 2014; 123: 1281–1282.
Hjalgrim H, Rostgaard K, Vasan SK, Ullum H, Erikstrup C, Pedersen OBV et al. No evidence of transmission of chronic lymphocytic leukemia through blood transfusion. Blood 2015; 126: 2059–2061.
Limpens J, Stad R, Vos C, de Vlaam C, de Jong D, van Ommen GJ et al. Lymphoma-associated translocation t(14;18) in blood B cells of normal individuals. Blood 1995; 85: 2528–2536.
Roulland S, Kelly RS, Morgado E, Sungalee S, Solal-Celigny P, Colombat P et al. t(14;18) translocation: a predictive blood biomarker for follicular lymphoma. J Clin Oncol 2014; 32: 1347–1345.
Janikova A, Mareckova A, Baumeisterova A, Krejci M, Supikova J, Salek D et al. Transmission of t(11;14)-positive cells by allogeneic stem cell transplant: 10-year journey to mantle cell lymphoma. Leuk Lymphoma 2014; 55: 1935–1938.
Niederwieser D, Gentilini C, Hegenbart U, Lange T, Moosmann P, Pönisch W et al. Transmission of donor illness by stem cell transplantation: should screening be different in older donors? Bone Marrow Transplant 2004; 34: 657–665.
Kiss TL, Chang H, Daly A, Messner HA, Jamal N, Spaner D et al. Bone marrow aspirates as part of routine donor assessment for allogeneic blood and marrow transplantation can reveal presence of occult hematological malignancies in otherwise asymptomatic individuals. Bone Marrow Transplant 2004; 33: 855–858.
Tilson MP, Jones RJ, Sexauer A, Griffin CA, Morsberger LA, Batista DA et al. Targeted pathologic evaluation of bone marrow donors identifies previously undiagnosed marrow abnormalities. Biol Blood Marrow Transplant 2013; 19: 1254–1270.
Sorror ML, Storb RF, Sandmaier BM, Maziarz RT, Pulsipher MA, Maris MB et al. Comorbidity-age index: a clinical measure of biologic age before allogeneic hematopoietic cell transplantation. J Clin Oncol 2014; 32: 3249–3256.
O’Donnell PV, Pedersen TL, Confer DL, Rizzo JD, Pulsipher MA, Stroncek D et al. Practice patterns for evaluation, consent, and care of related donors and recipients at hematopoietic cell transplantation centers in the United States. Blood 2010; 115: 5097–5101.
Shaw BE . First do no harm. Blood 2010; 115: 4978–4979.
Joint Accreditation Committee ISCT and EBMT. International Standards For Hematopoietic Cellular Therapy Product Collection, Processing, and Administration, 6th edn, p 38. Available at: http://www.jacie.org (last accessed 15 March 2016).
Anthias C, O’Donnell PV, Kiefer DM, Yared J, Norkin M, Anderlini P et al. European Group for Blood and Marrow Transplantation Centers with FACT-JACIE accreditation have significantly better compliance with related donor care standards. Biol Blood Marrow Transplant 2016; 22: 514–519.
Anthias C, Shaw BE, Kiefer DM, Liesveld JL, Yared J, Kamble RT et al. Significant improvements in the practice patterns of adult related donor care in US transplantation centers. Biol Blood Marrow Transplant 2016; 22: 520–527.
Alousi AM, Le-Rademacher J, Saliba RM, Appelbaum FR, Artz A, Benjamin J et al. Who is the better donor for older hematopoietic transplant recipients: an older-aged sibling or a young, matched unrelated volunteer? Blood 2013; 121: 2567–2573.
Kröger N, Zabelina T, de Wreede, Berger J, Alchalby H, van Biezen A et al. Allogeneic stem cell transplantation for older advanced MDS patients: improved survival with young unrelated donor in comparison with HLA-identical siblings. Leukemia 2013; 27: 604–609.
Acknowledgements
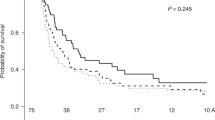
I am indebted to Dr Michael Pulsipher and Deidre Kiefer (National Marrow Donor Program) for sharing data and insight on the RDSafe Study (NCT00948636). I am grateful to Dr Marcelo Pasquini for his assistance in securing data from the CIBMTR. I am also indebted to Charles Martinez for his help in querying our institutional donor database and preparing the figure outlining these data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The author declares no conflict of interest.
Rights and permissions
About this article
Cite this article
Anderlini, P. Sixty as the new forty: considerations on older related stem cell donors. Bone Marrow Transplant 52, 15–19 (2017). https://doi.org/10.1038/bmt.2016.201
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2016.201
This article is cited by
-
Basic characteristics and safety of donation in related and unrelated haematopoietic progenitor cell donors – first 10 years of prospective donor follow-up of Swiss donors
Bone Marrow Transplantation (2022)
-
Prostaglandin E2 Enhances Aged Hematopoietic Stem Cell Function
Stem Cell Reviews and Reports (2021)