Abstract
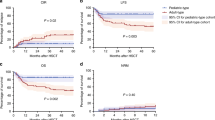
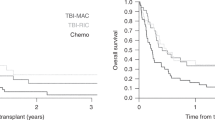
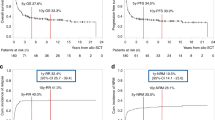
This study aims to provide a detailed analysis of allogeneic stem cell transplantation (allo-SCT) outcomes in a large T-cell acute lymphoblastic leukemia (T-ALL) cohort with a specific emphasis on the effects of pre-transplant minimal residual disease (MRD) and disease subtype, including the aggressive early-thymic precursor (ETP) subtype. Data from 102 allo-SCT patients with a diagnosis of T-ALL from three centers were retrospectively analyzed. Patients were grouped into four T-ALL subtypes: ETP, early, cortical and mature. At 3 years, overall survival (OS), PFS, non-relapse mortality and cumulative incidence (CI) progression were 35, 33, 11 and 55%, respectively. Patients transplanted in first complete remission (CR1) had a 3-year OS of 62% versus those transplanted in CR2 or greater (24%) (hazards ratio 1.6, P=0.2). Patients with MRD positivity at the time of transplant had significantly higher rates of progression compared with those with MRD negativity (76 vs 34%, hazards ratio 2.8, P=0.006). There was no difference in OS, PFS or cumulative incidence (CI) progression between disease subtypes, including ETP (n=16). ETP patients transplanted in CR1 (n=10) had OS of 47%, comparable to other disease subtypes, suggesting that allo-SCT can overcome the poor prognosis associated with ETP. MRD status at transplant was highly predictive of disease relapse, suggesting novel therapies are necessary to improve transplant outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Han X, Kilfoy B, Zheng T, Holford TR, Zhu C, Zhu Y et al. Lymphoma survival patterns by WHO subtype in the United States, 1973-2003. Cancer Causes Control 2008; 19: 841–858.
Kantarjian HM, O'Brien S, Smith TL, Cortes J, Giles FJ, Beran M et al. Results of treatment with hyper-CVAD, a dose-intensive regimen, in adult acute lymphocytic leukemia. J Clin Oncol 2000; 18: 547–561.
Rytting ME, Thomas DA, O'Brien SM, Ravandi-Kashani F, Jabbour EJ, Franklin AR et al. Augmented Berlin-Frankfurt-Munster therapy in adolescents and young adults (AYAs) with acute lymphoblastic leukemia (ALL). Cancer 2014; 120: 3660–3668.
Chang JE, Medlin SC, Kahl BS, Longo WL, Williams EC, Lionberger J et al. Augmented and standard Berlin-Frankfurt-Munster chemotherapy for treatment of adult acute lymphoblastic leukemia. Leuk Lymphoma 2008; 49: 2298–2307.
Rowe JM, Buck G, Burnett AK, Chopra R, Wiernik PH, Richards SM et al. Induction therapy for adults with acute lymphoblastic leukemia: results of more than 1500 patients from the international ALL trial: MRC UKALL XII/ECOG E2993. Blood 2005; 106: 3760–3767.
Marks DI, Paietta EM, Moorman AV, Richards SM, Buck G, DeWald G et al. T-cell acute lymphoblastic leukemia in adults: clinical features, immunophenotype, cytogenetics, and outcome from the large randomized prospective trial (UKALL XII/ECOG 2993). Blood 2009; 114: 5136–5145.
Bakr M, Rasheed W, Mohamed SY, Al-Mohareb F, Chaudhri N, Al-Sharif F et al. Allogeneic hematopoietic stem cell transplantation in adolescent and adult patients with high-risk T cell acute lymphoblastic leukemia. Biol Blood Marrow Transplant 2012; 18: 1897–1904.
Cahu XLM, Giebel S, Socie G et al Myeloablative allogeneic hematopoietic stem cell transplantation for adult patients with T-cell acute lymphoblastic leukemia: a survey from the acute leukemia working party of the european group for blood and marrow transplantation (EBMT). Blood 2012: Abstract 356.
Hoelzer DTE, Arnold R, Joachim Beck, Beelen D et al Successful subtype oriented treatment strategies in adult T-ALL; results of 744 patients treated in three consecutive GMALL studies. Blood 2009: Abstract 324.
Dhedin N, Huynh A, Maury S, Tabrizi R, Beldjord K, Asnafi V et al. Role of allogeneic stem cell transplantation in adult patients with Ph-negative acute lymphoblastic leukemia. Blood 2015; 125: 2486–2496.
Bruggemann M, Raff T, Flohr T, Gokbuget N, Nakao M, Droese J et al. Clinical significance of minimal residual disease quantification in adult patients with standard-risk acute lymphoblastic leukemia. Blood 2006; 107: 1116–1123.
Raff T, Gokbuget N, Luschen S, Reutzel R, Ritgen M, Irmer S et al. Molecular relapse in adult standard-risk ALL patients detected by prospective MRD monitoring during and after maintenance treatment: data from the GMALL 06/99 and 07/03 trials. Blood 2007; 109: 910–915.
Gokbuget N, Kneba M, Raff T, Trautmann H, Bartram CR, Arnold R et al. Adult patients with acute lymphoblastic leukemia and molecular failure display a poor prognosis and are candidates for stem cell transplantation and targeted therapies. Blood 2012; 120: 1868–1876.
Willemse MJ, Seriu T, Hettinger K, d'Aniello E, Hop WC, Panzer-Grumayer ER et al. Detection of minimal residual disease identifies differences in treatment response between T-ALL and precursor B-ALL. Blood 2002; 99: 4386–4393.
Wood BL WSS, Dunsmore KP, Devidas M et al. T-lymphoblastic leukemia (T-ALL) shows excellent outcome, lack of significance of early thymic precursor (ETP) immunophenotype, and validation of the prognostic value of end-induction minimal residual disease (MRD) in children's oncology group (COG) study AALL0434. Blood 2014; 124 Abstract 1.
Zhou Y, Slack R, Jorgensen JL, Wang SA, Rondon G, de Lima M et al. The effect of peritransplant minimal residual disease in adults with acute lymphoblastic leukemia undergoing allogeneic hematopoietic stem cell transplantation. Clin Lymphoma Myeloma Leuk 2014; 14: 319–326.
Bar M, Wood BL, Radich JP, Doney KC, Woolfrey AE, Delaney C et al. Impact of minimal residual disease, detected by flow cytometry, on outcome of myeloablative hematopoietic cell transplantation for acute lymphoblastic leukemia. Leuk Res Treat 2014; 2014: 421723.
Coustan-Smith E, Mullighan CG, Onciu M, Behm FG, Raimondi SC, Pei D et al. Early T-cell precursor leukaemia: a subtype of very high-risk acute lymphoblastic leukaemia. Lancet Oncol 2009; 10: 147–156.
Allen A, Sireci A, Colovai A, Pinkney K, Sulis M, Bhagat G et al. Early T-cell precursor leukemia/lymphoma in adults and children. Leuk Res 2013; 37: 1027–1034.
Patrick K, Wade R, Goulden N, Mitchell C, Moorman AV, Rowntree C et al. Outcome for children and young people with Early T-cell precursor acute lymphoblastic leukaemia treated on a contemporary protocol, UKALL 2003. Br J Haematol 2014; 166: 421–424.
Jain N, Lamb AE, O'Brien S, Ravandi F, Konopleva M, Jabbour E et al. Early T-cell precursor acute lymphoblastic leukemia/lymphoma (ETP-ALL/LBL) in adolescents and adults: a high-risk subtype. Blood 2016; 127: 1863–1869.
Gokbuget N, Basara N, Baurmann H, Beck J, Bruggemann M, Diedrich H et al. High single-drug activity of nelarabine in relapsed T-lymphoblastic leukemia/lymphoma offers curative option with subsequent stem cell transplantation. Blood 2011; 118: 3504–3511.
Fielding AK, Richards SM, Chopra R, Lazarus HM, Litzow MR, Buck G et al. Outcome of 609 adults after relapse of acute lymphoblastic leukemia (ALL); an MRC UKALL12/ECOG 2993 study. Blood 2007; 109: 944–950.
Borowitz MJ CJ. T-Lymphoblastic Leukaemia/Lymphoma. In: Swerdlow SH, Campo E, Harris NL et al. (eds). WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues: World Health Organization Classification of Tumors. International Agency for Research on Cancer (IARC): Lyon, France, 2008.
Bene MC, Castoldi G, Knapp W, Ludwig WD, Matutes E, Orfao A et al. Proposals for the immunological classification of acute leukemias. European Group for the Immunological Characterization of Leukemias (EGIL). Leukemia 1995; 9: 1783–1786.
Glucksberg H, Storb R, Fefer A, Buckner CD, Neiman PE, Clift RA et al. Clinical manifestations of graft-versus-host disease in human recipients of marrow from HL-A-matched sibling donors. Transplantation 1974; 18: 295–304.
Shulman HM, Sullivan KM, Weiden PL, McDonald GB, Striker GE, Sale GE et al. Chronic graft-versus-host syndrome in man. A long-term clinicopathologic study of 20 Seattle patients. Am J Med 1980; 69: 204–217.
Pullarkat V, Slovak ML, Kopecky KJ, Forman SJ, Appelbaum FR . Impact of cytogenetics on the outcome of adult acute lymphoblastic leukemia: results of Southwest Oncology Group 9400 study. Blood 2008; 111: 2563–2572.
Cassaday RD, Alan Potts D Jr, Stevenson PA, Bar M, Georges GE, Shustov AR et al. Evaluation of allogeneic transplantation in first or later minimal residual disease - negative remission following adult-inspired therapy for acute lymphoblastic leukemia. Leuk Lymphoma 2016; 57: 1–10.
Mohty M, Labopin M, Volin L, Gratwohl A, Socie G, Esteve J et al. Reduced-intensity versus conventional myeloablative conditioning allogeneic stem cell transplantation for patients with acute lymphoblastic leukemia: a retrospective study from the European Group for Blood and Marrow Transplantation. Blood 2010; 116: 4439–4443.
Gorin NC, Giebel S, Labopin M, Savani BN, Mohty M, Nagler A . Autologous stem cell transplantation for adult acute leukemia in 2015: time to rethink? Present status and future prospects. Bone Marrow Transplant 2015; 50: 1495–1502.
Parachnicova EKL, Mendeleeva L, Akhmerzaeva Z, Bondarenko S et al Autologous hematopoietic stem cell transplantation followed by prolonged maintenance provides survival benefit over only-chemotherapy in T-cell acute lymphoblastic leukemia: results of the RALL study group. 40th Annual Meeting of the EBMT, Milan, Italy 2014.
Mansour MR, Sulis ML, Duke V, Foroni L, Jenkinson S, Koo K et al. Prognostic implications of NOTCH1 and FBXW7 mutations in adults with T-cell acute lymphoblastic leukemia treated on the MRC UKALLXII/ECOG E2993 protocol. J Clin Oncol 2009; 27: 4352–4356.
Asnafi V, Buzyn A, Le Noir S, Baleydier F, Simon A, Beldjord K et al. NOTCH1/FBXW7 mutation identifies a large subgroup with favorable outcome in adult T-cell acute lymphoblastic leukemia (T-ALL): a Group for Research on Adult Acute Lymphoblastic Leukemia (GRAALL) study. Blood 2009; 113: 3918–3924.
Acknowledgements
We acknowledge William Dibb for his contributions to data collection and Guang Fan for her contributions regarding pathology data from OHSU. The authors have no source of income for this study to declare.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on Bone Marrow Transplantation website
Supplementary information
Rights and permissions
About this article
Cite this article
Brammer, J., Saliba, R., Jorgensen, J. et al. Multi-center analysis of the effect of T-cell acute lymphoblastic leukemia subtype and minimal residual disease on allogeneic stem cell transplantation outcomes. Bone Marrow Transplant 52, 20–27 (2017). https://doi.org/10.1038/bmt.2016.194
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2016.194
This article is cited by
-
A prognostic score system in adult T‐cell acute lymphoblastic leukemia after hematopoietic stem cell transplantation
Bone Marrow Transplantation (2024)
-
Upfront allogeneic hematopoietic stem cell transplantation for adult T-cell acute lymphoblastic leukemia/lymphoma in first complete remission: a single-center study
Annals of Hematology (2024)
-
PLK1 as a cooperating partner for BCL2-mediated antiapoptotic program in leukemia
Blood Cancer Journal (2023)
-
Idasanutlin and navitoclax induce synergistic apoptotic cell death in T-cell acute lymphoblastic leukemia
Leukemia (2023)
-
Inserting EF1α-driven CD7-specific CAR at CD7 locus reduces fratricide and enhances tumor rejection
Leukemia (2023)