Abstract
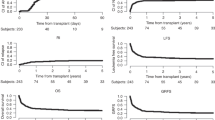
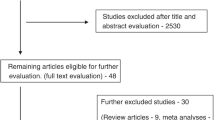
To assess the impact of spleen status on engraftment, and early morbidity and mortality after allogeneic hematopoietic cell transplantation (HCT), we analyzed 9,683 myeloablative allograft recipients from 1990 to 2006; 472 had prior splenectomy (SP), 300 splenic irradiation (SI), 1,471 with splenomegaly (SM), and 7,440 with normal spleen (NS). Median times to neutrophil engraftment (NE) and platelet engraftment (PE) were 15 vs 18 days and 22 vs 24 days for the SP and NS groups, respectively (P<0.001). Hematopoietic recovery at day +100 was not different across all groups, however the odds ratio of days +14 and +21 NE and day +28 PE were 3.26, 2.25 and 1.28 for SP, and 0.56, 0.55, and 0.82 for SM groups compared to NS (P<0.001), respectively. Among patients with SM, use of peripheral blood grafts improved NE at day +21, and CD34+ cell dose >5.7 × 106/kg improved PE at day+28. After adjusting variables by Cox regression, the incidence of GVHD and OS were not different among groups. SM is associated with delayed engraftment, whereas SP prior to HCT facilitates early engraftment without having an impact on survival.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Helenglass G, Treleaven J, Parikh P, Aboud H, Smith C, Powles R . Delayed engraftment associated with splenomegaly in patients undergoing bone marrow transplantation for chronic myeloid leukaemia. Bone Marrow Transplant 1990; 5: 247–251.
Battiwalla M, McCarthy PL . Filgrastim support in allogeneic HSCT for myeloid malignancies: a review of the role of G-CSF and the implications for current practice. Bone Marrow Transplant 2009; 43: 351–356.
Bensinger WI, Martin PJ, Storer B, Clift R, Forman SJ, Negrin R et al. Transplantation of bone marrow as compared with peripheral-blood cells from HLA-identical relatives in patients with hematologic cancers. N Engl J Med 2001; 344: 175–181.
Ozer H, Armitage JO, Bennett CL, Crawford J, Demetri GD, Pizzo PA et alAmerican society of clinical oncology growth factors expert panel. Update of recommendations for the use of hematopoietic colony-stimulating factors: evidence-based, clinical practice guidelines. J Clin Oncol 2000; 18: 3558–3585.
Baughan AS, Worsley AM, McCarthy DM, Hows JM, Catovsky D, Gordon-Smith EC et al. Haematological reconstitution and severity of graft-versus-host disease after bone marrow transplantation for chronic granulocytic leukaemia: the influence of previous splenectomy. Br J Haematol 1984; 56: 445–454.
Gluckman E, Devergie A, Bernheim A, Berger R . Splenectomy and bone marrow transplantation in chronic granulocytic leukaemia. Lancet 1983; 1: 1392–1393.
Gratwohl A, Goldman J, Gluckman E, Zwaan F . Effect of splenectomy before bone-marrow transplantation on survival in chronic granulocytic leukaemia. Lancet 1985; 2: 1290–1291.
Deeg HJ, Gooley TA, Flowers ME, Sale GE, Slattery JT, Anasetti C et al. Allogeneic hematopoietic stem cell transplantation for myelofibrosis. Blood 2003; 102: 3912–3918.
Li Z, Deeg HJ . Pros and cons of splenectomy in patients with myelofibrosis undergoing stem cell transplantation. Leukemia 2001; 15: 465–467.
Li Z, Gooley T, Applebaum FR, Deeg HJ . Splenectomy and hemopoietic stem cell transplantation for myelofibrosis. Blood 2001; 97: 2180–2181.
Martino R, Altes A, Muniz-Diaz E, Brunet S, Sureda A, Domingo-Albos A et al. Reduced transfusion requirements in a splenectomized patient undergoing bone marrow transplantation. Acta Haematol 1994; 92: 167–168.
Stewart WA, Pearce R, Kirkland KE, Bloor A, Thomson K, Apperley J et al. The role of allogeneic SCT in primary myelofibrosis: a British society for blood and marrow transplantation study. Bone Marrow Transplant 2010; 45: 1587–1593.
Ringden O, Nilsson B . Death by graft-versus-host disease associated with HLA mismatch, high recipient age, low marrow cell dose, and splenectomy. Transplantation 1985; 40: 39–44.
Sundin M, Le Blanc K, Ringden O, Barkholt L, Omazic B, Lergin C et al. The role of HLA mismatch, splenectomy and recipient Epstein-Barr virus seronegativity as risk factors in post-transplant lymphoproliferative disorder following allogeneic hematopoietic stem cell transplantation. Haematologica 2006; 91: 1059–1067.
Elliott MA, Tefferi A . Splenic irradiation in myelofibrosis with myeloid metaplasia: a review. Blood Rev 1999; 13: 163–170.
Pasquini MC, Wang Z, Horowitz M, Gale RP . 2010 report from the center for international blood and marrow transplant research (CIBMTR): current uses and outcomes of hematopoietic cell transplant for blood and bone marrow disorders. In: Cecka JM, Terazaki PI, (eds). Clinical Transplants 2010. The Terasaki Foundation Laboratory: Los Angeles,, 2011.
Bacigalupo A, Ballen K, Rizzo D, Giralt S, Lazarus H, Ho V et al. Defining the intensity of conditioning regimens: working definitions. Biol Blood Marrow Transplant 2009; 15: 1628–1633.
Shulman HM, Sullivan KM, Weiden PL, McDonald GB, Striker GE, Sale GE et al. Chronic graft-versus-host syndrome in man. A long-term clinicopathologic study of 20 Seattle patients. Am J Med 1980; 69: 204–217.
Jetmore A, Plett PA, Tong X, Wolber FM, Breese R, Abonour R et al. Homing efficiency, cell cycle kinetics, and survival of quiescent and cycling human CD34(+) cells transplanted into conditioned NOD/SCID recipients. Blood 2002; 99: 1585–1593.
Szilvassy SJ, Bass MJ, Van Zant G, Grimes B . Organ-selective homing defines engraftment kinetics of murine hematopoietic stem cells and is compromised by ex vivo expansion. Blood 1999; 93: 1557–1566.
van Hennik PB, de Koning AE, Ploemacher RE . Seeding efficiency of primitive human hematopoietic cells in nonobese diabetic/severe combined immune deficiency mice: implications for stem cell frequency assessment. Blood 1999; 94: 3055–3061.
Wright DE, Wagers AJ, Gulati AP, Johnson FL, Weissman IL . Physiological migration of hematopoietic stem and progenitor cells. Science 2001; 294: 1933–1936.
Plett PA, Frankovitz SM, Orschell CM . Distribution of marrow repopulating cells between bone marrow and spleen early after transplantation. Blood 2003; 102: 2285–2291.
Smith LH, McKinley TW . Recovery from radiation injury with and without bone marrow transplantation: effects of splenectomy. Radiat Res 1970; 44: 248–261.
Tanaka N . Experimental studies on role of spleen in recovery from radiation injury in mice. 3. Effect of splenectomy on survival of mice with spleen and bone marrow transplantation following lethal x-irradiation. Hiroshima J Med Sci 1966; 15: 347–378.
Richard C, Romon I, Perez-Encinas M, Baro J, Rabunal MJ, Mazorra F et al. Splenectomy for poor graft function after allogeneic bone marrow transplantation in patients with chronic myeloid leukemia. Leukemia 1996; 10: 1615–1618.
Robin M, Esperou H, de Latour RP, Petropoulou AD, Xhaard A, Ribaud P et al. Splenectomy after allogeneic haematopoietic stem cell transplantation in patients with primary myelofibrosis. Br J Haematol 150: 721–724.
von Bueltzingsloewen A, Bordigoni P, Dorvaux Y, Witz F, Schmitt C, Chastagner P et al. Splenectomy may reverse pancytopenia occurring after allogeneic bone marrow transplantation. Bone Marrow Transplant 1994; 14: 339–340.
Park AE, Birgisson G, Mastrangelo MJ, Marcaccio MJ, Witzke DB . Laparoscopic splenectomy: outcomes and lessons learned from over 200 cases. Surgery 2000; 128: 660–667.
Bacigalupo A, Soraru M, Dominietto A, Pozzi S, Geroldi S, Van Lint MT et al. Allogeneic hemopoietic SCT for patients with primary myelofibrosis: a predictive transplant score based on transfusion requirement, spleen size and donor type. Bone Marrow Transplant 2010; 45: 458–463.
Acknowledgements
The CIBMTR is supported by Public Health Service Grant/Cooperative Agreement U24-CA76518 from the National Cancer Institute, the National Heart, Lung and Blood Institute (NHLBI) and the National Institute of Allergy and Infectious Diseases (NIAID); a Grant/Cooperative Agreement 5U01HL069294 from NHLBI and NCI; a contract HHSH234200637015C with Health Resources and Services Administration (HRSA/DHHS); two grants N00014-06-1-0704 and N00014-08-1-0058 from the Office of Naval Research; and grants from Allos, Inc.; Amgen, Inc.; Angioblast; anonymous donation to the Medical College of Wisconsin; Ariad; Be the Match Foundation; Blue Cross and Blue Shield Association; Buchanan Family Foundation; CaridianBCT; Celgene Corporation; CellGenix, GmbH; Children’s Leukemia Research Association; Fresenius-Biotech North America, Inc.; Gamida Cell Teva Joint Venture Ltd.; Genentech, Inc.; Genzyme Corporation; GlaxoSmithKline; Kiadis Pharma; The Leukemia and Lymphoma Society; the Medical College of Wisconsin; Millennium Pharmaceuticals, Inc.; Milliman USA, Inc.; Miltenyi Biotec, Inc.; National Marrow Donor Program; Optum Healthcare Solutions, Inc.; Otsuka America Pharmaceutical, Inc.; Seattle Genetics; Sigma-Tau Pharmaceuticals; Soligenix, Inc.; Swedish Orphan Biovitrum; THERAKOS, Inc.; and Wellpoint, Inc. The views expressed in this article do not reflect the official policy or position of the National Institute of Health, the Department of the Navy, the Department of Defense or any other agency of the U.S. Government.
Author contributions: GA designed the study, interpreted results, and drafted the manuscript; BL, MAA analyzed data and interpreted results; MCP, HML, DIM, MB, OR, RTM, VG, UP, DM, BJB, JDR, KKB, KRC, PLM and VTH critically reviewed and revised the manuscript; and all authors approved the final version.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Akpek, G., Pasquini, M., Logan, B. et al. Effects of spleen status on early outcomes after hematopoietic cell transplantation. Bone Marrow Transplant 48, 825–831 (2013). https://doi.org/10.1038/bmt.2012.249
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2012.249
Keywords
This article is cited by
-
The application of JAK inhibitors in the peri-transplantation period of hematopoietic stem cell transplantation for myelofibrosis
Annals of Hematology (2024)
-
Pretransplant hepatomegaly is linked to relapse in patients with leukemia and myelodysplastic syndrome not in remission
International Journal of Hematology (2024)
-
Pretransplant spleen volume and outcome after hematopoietic stem cell transplantation (HSCT) in patients with acute myeloid leukemia (AML)
Annals of Hematology (2023)
-
Comparing cord blood transplantation and matched related donor transplantation in non-remission acute myeloid leukemia
Leukemia (2022)
-
The role of JAK inhibitors in hematopoietic cell transplantation
Bone Marrow Transplantation (2022)