Abstract
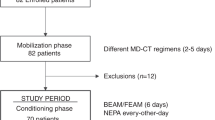
Complete protection from nausea/vomiting is currently achieved in a minority of patients receiving high-dose chemotherapy (HDC). Currently the use of 5-HT3-antagonists and dexamethasone (DEX) represents the standard of care. The role of the NK-1-antagonist aprepitant in HDC remains to be better defined. A total of 64 patients undergoing multiple days of HDC received granisetron, DEX plus aprepitant during chemotherapy. After the end of chemotherapy aprepitant plus DEX was given for a further 2 days. Primary end point was CR defined as no vomiting and no use of rescue medication in the overall phase (day 1 until 5 days after end of chemotherapy). Acute/delayed and overall CR were achieved in 83%/70% and 63%, respectively. Acute and delayed nausea were observed in 20 and 38% of the patients. The tolerability of the aprepitant regimen over 4–5 days was comparable with the 3-day antiemetic regimen. In our study, aprepitant demonstrated good tolerability. Taking into account the methodological constraints of comparing our results with those from the available literature, the addition of aprepitant to the antiemetic treatment regimen may provide improved prevention of chemotherapy-induced nausea and vomiting during HDC.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Coates A, Abraham S, Kaye SB, Sowerbutts T, Frewin C, Fox RM et al. On the receiving end--patient perception of the side-effects of cancer chemotherapy. Eur J Cancer Clin Oncol 1983; 19: 203–208.
Griffin AM, Butow PN, Coates AS, Childs AM, Ellis PM, Dunn SM et al. On the receiving end V: patient perceptions of the side effects of cancer chemotherapy in 1993. Ann Oncol 1996; 7: 189–195.
Einhorn LH, Rapoport B, Koeller J, Grunberg SM, Feyer P, Rittenberg C et al. Antiemetic therapy for multiple-day chemotherapy and high-dose chemotherapy with stem cell transplant: review and consensus statement. Support Care Cancer 2005; 13: 112–116.
Kris MG, Hesketh PJ, Somerfield MR, Feyer P, Clark-Snow R, Koeller JM et al. American Society of Clinical Oncology guideline for antiemetics in oncology: update 2006. J Clin Oncol 2006; 24: 2932–2947.
Roila F, Herrstedt J, Aapro M . Guideline update for MASCC and ESMO in the prevention of chemotherapy- and radiotherapy-induced nausea and vomiting: results of the Perugia consensus conference. Ann Oncol 2010; 21 (Suppl 5): v232–v243.
Trigg ME, Inverso DM . Nausea and vomiting with high-dose chemotherapy and stem cell rescue therapy: a review of antiemetic regimens. Bone Marrow Transplant 2008; 42: 501–506.
Bubalo JS, Leis JF, Curtin PT, Maziarz RT, Kovascovics TJ, Meyers G A randomized, double blinded, pilot trial of aprepitant added to standard antiemetics during conditioning therapy for hematopoietic stem cell transplant (HSCT). J Clin Oncol 2007; 25 (no. 18 s): 9112.
Paul B, Trovato JA, Thompson J, Badros AZ, Goloubeva O . Efficacy of aprepitant in patients receiving high-dose chemotherapy with hematopoietic stem cell support. J Oncol Pharm Pract 2010; 16: 45–51.
Roila F, Del Favero A, Gralla R . Prevention of chemotherapy and radiotherapy-induced emesis: results of the Perugia consensus conference. Ann Oncol 1998; 9: 811–819.
Viner CV, Selby PJ, Zulian GB, Gore ME, Butcher ME, Wootton CM et al. Ondansetron--a new safe and effective antiemetic in patients receiving high-dose melphalan. Cancer Chemother Pharmacol 1990; 25: 449–453.
Barbounis V, Koumakis G, Hatzichristou H, Vassilomanolakis M, Tsoussis S, Efremidis A . The anti-emetic efficacy of tropisetron plus dexamethasone in patients treated with high-dose chemotherapy and stem cell transplantation. Support Care Cancer 1999; 7: 79–83.
Or R, Drakos P, Nagler A, Naparstek E, Kapelushnik J, Cass Y . The anti-emetic efficacy and tolerability of tropisetron in patients conditioned with high-dose chemotherapy (with and without total body irradiation) prior to bone marrow transplantation. Support Care Cancer 1994; 2: 245–248.
Frakes LA, Brehm TL, Kosty MP, Miller WE, McMillan RL, Mason J et al. An all oral antiemetic regimen for patients undergoing high-dose chemotherapy with peripheral blood stem cell transplant. Bone Marrow Transplant 1997; 20: 473–478.
Lopez-Jimenez J, Martin-Ballesteros E, Sureda A, Uralburu C, Lorenzo I, del Campo R et al. Chemotherapy-induced nausea and vomiting in acute leukemia and stem cell transplant patients: results of a multicenter, observational study. Haematologica 2006; 91: 84–91.
Climent MA, Palau J, Ruiz A, Soriano V, Aznar E, Olmos T et al. The antiemetic efficacy of granisetron plus dexamethasone, haloperidol and loracepam in breast cancer patients treated with high-dose chemotherapy with peripheral blood stem-cell support. Support Care Cancer 1998; 6: 287–290.
Bubalo J, Seelig F, Karbowicz S, Maziarz RT . Randomized open-label trial of dolasetron for the control of nausea and vomiting associated with high-dose chemotherapy with hematopoietic stem cell transplantation. Biol Blood Marrow Transplant 2001; 7: 439–445.
Junagadhwalla MCJ, Gentile T . Prolonged administration of aprepitant does not increase toxicity in patients undergoing high dose chemotherapy and autologous stem cell transplant. Blood 2005; 106: (517b).
Barnet CMOM, Popat U . Evaluation of aprepitant for treatment of acute and delayed chemotherapy-induced nausea and vomiting in patients undergoing autologous stem cell transplantation. Blood 2004; 104: (343b).
Szer JGA, Grigg AP, Roberts AP, Raunow H . Aprepitant in the prevention of acute and delayed nausea and vomiting following haematopoietic stem cell transplantation: a pilot study. Bone Marrow Transplant 2006; 37 (Suppl I): 112.
Stiff P, Fox-Geimann MP, Kiley K, Fletcher-Gonzalez D, Porter N, Rychlik K et al. A prospective, randomized phase III trial of oral ondansetron and dexamethasone alone vs oral ondansetron, dexamethasone and the NK-1 Inhibitor, Aprepitant (Emend) for the prevention of nausea and vomiting associated with highly emetogenic preparative regimens prior to stem cell transplantation. ASH 2009; 22: 2267.
Jordan K, Kinitz I, Voigt W, Behlendorf T, Wolf HH, Schmoll HJ . Safety and efficacy of a triple antiemetic combination with the NK-1 antagonist aprepitant in highly and moderately emetogenic multiple-day chemotherapy. Eur J Cancer 2009; 45: 1184–1187.
Hesketh PJ, Grunberg SM, Gralla RJ, Warr DG, Roila F, de Wit R et al. The oral neurokinin-1 antagonist aprepitant for the prevention of chemotherapy-induced nausea and vomiting: a multinational, randomized, double-blind, placebo-controlled trial in patients receiving high-dose cisplatin--the Aprepitant Protocol 052 Study Group. J Clin Oncol 2003; 21: 4112–4119.
Poli-Bigelli S, Rodrigues-Pereira J, Carides AD, Julie MAG, Eldridge K, Hipple A et al. Addition of the neurokinin 1 receptor antagonist aprepitant to standard antiemetic therapy improves control of chemotherapy-induced nausea and vomiting. Results from a randomized, double-blind, placebo-controlled trial in Latin America. Cancer 2003; 97: 3090–3098.
Durand JP, Gourmel B, Mir O, Goldwasser F . Antiemetic neurokinin-1 antagonist aprepitant and ifosfamide-induced encephalopathy. Ann Oncol 2007; 18: 808–809.
Howell JE, Szabatura AH, Hatfield Seung A, Nesbit SA . Characterization of the occurrence of ifosfamide-induced neurotoxicity with concomitant aprepitant. J Oncol Pharm Pract 2008; 14: 157–162.
Acknowledgements
We thank Dr H-J Olbert for assistance in preparing the paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
K Jordan and H-J Schmoll have received compensation as members of the scientific advisory board of MSD Merck Sharp and Dohme. The remaining authors declare no conflict of interest
Rights and permissions
About this article
Cite this article
Jordan, K., Jahn, F., Jahn, P. et al. The NK-1 receptor-antagonist aprepitant in high-dose chemotherapy (highdose melphalan and high-dose T-ICE: paclitaxel, ifosfamide, carboplatin, etoposide): efficacy and safety of a triple antiemetic combination. Bone Marrow Transplant 46, 784–789 (2011). https://doi.org/10.1038/bmt.2010.205
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2010.205
Keywords
This article is cited by
-
Aprepitant, fosaprepitant and risk of ifosfamide-induced neurotoxicity: a systematic review
Cancer Chemotherapy and Pharmacology (2022)
-
Antiemetic Strategies in Patients Who Undergo Hematopoietic Stem Cell Transplantation
Clinical Hematology International (2022)
-
Multiple-day administration of fosaprepitant combined with tropisetron and olanzapine improves the prevention of nausea and vomiting in patients receiving chemotherapy prior to autologous hematopoietic stem cell transplant: a retrospective study
Annals of Hematology (2022)
-
Netupitant/palonosetron without dexamethasone for preventing nausea and vomiting in patients with multiple myeloma receiving high-dose melphalan for autologous stem cell transplantation: a single-center experience
Supportive Care in Cancer (2022)
-
Prevention of chemotherapy-induced nausea and vomiting after high-dose melphalan and stem cell transplantation: review of the evidence and suggestions
Supportive Care in Cancer (2019)