Abstract
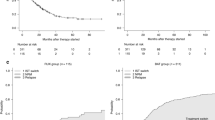
The relationship between tacrolimus concentration and acute GVHD is not well known, with few published data available for lower target levels. We hypothesized that lower levels of tacrolimus would correlate with higher incidence of acute GVHD and poorer prognosis. Receiver operator characteristic curves (ROC) were used to quantify tacrolimus blood levels as predictors of grade II–IV acute GVHD. A total of 97 pediatric patients with hematological malignancies met the study criteria. On the ROC, a cutoff of 7 ng/ml provided the best balance between sensitivity and specificity (62.8 vs 68.2%, respectively). Cumulative incidence of acute GVHD was 65.9% (range 58.5–73.3%) in patients with mean tacrolimus concentration of ⩽7 ng/ml and 34.8% (range 27.8–41.8%) in patients with mean tacrolimus concentration of >7 ng/ml (P=0.002). Incidence of non-relapse mortality (NRM) was higher in patients with tacrolimus of ⩽7 ng/ml (42.9%; range 35.6–50.2%) than in patients with tacrolimus of >7 ng/ml (28.3%; range 17.4–39.2%; P=0.008). This translated into better EFS in patients with tacrolimus of >7 ng/ml (48.9%; range 39.8–58.0%) than in patients with tacrolimus of ⩽7 ng/ml (31.8%; range 25.0–38.6%; P=0.031). Multivariate analysis showed that tacrolimus concentration was significantly associated with clinical outcomes. Mean whole-blood level of tacrolimus as continuous infusion should be maintained at ⩾7 ng/ml for pediatric patients.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Wingard JR, Nash RA, Przepiorka D, Klein JL, Weisdorf DJ, Fay JW et al. Relationship of tacrolimus (FK506) whole blood concentrations and efficacy and safety after HLA-identical sibling bone marrow transplantation. Biol Blood Marrow Transplant 1998; 4: 157–163.
Przepiorka D, Saliba R, Cleary K, Fischer H, Tonai R, Fritsche H et al. Tacrolimus does not abrogate the increased risk of acute graft-versus-host disease after unrelated-donor marrow transplantation with allelic mismatching at HLA-DRB1 and HLA-DQB1. Biol Blood Marrow Transplant 2000; 6: 190–197.
Morishima Y, Morishita Y, Tanimoto M, Ohno R, Saito H, Horibe K et al. Low incidence of acute graft-versus-host disease by the administration of methotrexate and cyclosporine in Japanese leukemia patients after bone marrow transplantation from human leukocyte antigen compatible siblings; possible role of genetic homogeneity. The Nagoya Bone Marrow Transplantation Group. Blood 1989; 74: 2252–2256.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J et al. 1994 Consensus conference on acute GVHD grading. Bone Marrow Transplant 1995; 15: 825–828.
Przepiorka D, Nash RA, Wingard JR, Zhu J, Maher RM, Fitzsimmons WE et al. Relationship of tacrolimus whole blood levels to efficacy and safety outcomes after unrelated donor marrow transplantation. Biol Blood Marrow Transplant 1999; 5: 94–97.
Nishida T, Hamaguchi M, Hirabayashi N, Haneda M, Terakura S, Atsuta Y et al. Intestinal thrombotic microangiopathy after allogeneic bone marrow transplantation: a clinical imitator of acute enteric graft-versus-host disease. Bone Marrow Transplant 2004; 33: 1143–1150.
Fujino M, Kim Y, Ito M . Intestinal thrombotic microangiopathy induced by FK506 in rats. Bone Marrow Transplant 2007; 39: 367–372.
Nakamae H, Yamane T, Hasegawa T, Nakamae M, Terada Y, Hagihara K et al. Risk factor analysis for thrombotic microangiopathy after reduced-intensity or myeloablative allogeneic hematopoietic stem cell transplantation. Am J Hematol 2006; 81: 525–531.
Oran B, Donato M, Aleman A, Hosing C, Korbling M, Detry MA et al. Transplant-associated microangiopathy in patients receiving tacrolimus following allogeneic stem cell transplantation: risk factors and response to treatment. Biol Blood Marrow Transplant 2007; 13: 469–477.
Przepiorka D, Blamble D, Hilsenbeck S, Danielson M, Krance R, Chan KW . Tacrolimus clearance is age-dependent within the pediatric population. Bone Marrow Transplant 2000; 26: 601–605.
Wong R, Shahjahan M, Wang X, Thall PF, De Lima M, Khouri I et al. Prognostic factors for outcomes of patients with refractory or relapsed acute myelogenous leukemia or myelodysplastic syndromes undergoing allogeneic progenitor cell transplantation. Biol Blood Marrow Transplant 2005; 11: 108–114.
Nakamura Y, Takeuchi H, Okuyama K, Akashi T, Jojima Y, Konno O et al. Evaluation of appropriate blood level in continuous intravenous infusion from trough concentrations after oral administration based on area under trough level in tacrolimus and cyclosporine therapy. Transplant Proc 2005; 37: 1725–1727.
Acknowledgements
This work was supported by a grant from the Ministry of Health, Labour, and Welfare of Japan, Tokyo.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Watanabe, N., Matsumoto, K., Muramatsu, H. et al. Relationship between tacrolimus blood concentrations and clinical outcome during the first 4 weeks after SCT in children. Bone Marrow Transplant 45, 1161–1166 (2010). https://doi.org/10.1038/bmt.2009.327
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2009.327
Keywords
This article is cited by
-
Intrapatient variability in concentration/dose ratio of tacrolimus predicts transplant-associated thrombotic microangiopathy
International Journal of Hematology (2021)
-
Prophylactic and therapeutic treatment of graft-versus-host disease in Japan
International Journal of Hematology (2015)