Abstract
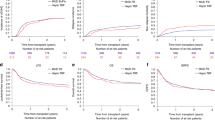
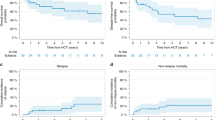
Allogeneic hematopoietic SCT (allo-HCT) is the only curative therapy for myelodysplastic syndrome (MDS). Numerous myeloablative (MA), nonmyeloablative SCT (NST) and reduced conditioning transplant (RIC) studies have included MDS patients. Twenty-four MA HCT studies published from 2000 and 2008 reported OS and disease-free survival (DFS) ranging from 25 and 16% at 2 years to 52 and 50% at 4 years. In these publications, the incidence of grades II–IV acute GVHD was 18–100%, chronic GVHD 13–88%, relapse risk 24% at 1 year to 54.5% at 4 years and TRM 19% at day 100 to 61% at 5 years. From 2003 to 2008, 30 publications combining RIC and NST reported OS and DFS from 22 and 20% at 2 years to 79 and 79% at 4 years. Incidence of grades II–IV acute GVHD ranged from 9 to 63%, chronic GVHD 18 to 80%, relapse risk 6 to 61% and TRM 0% at day 100 to 34% at 5 years. The wide range in the published results leaves many unanswered questions. Although no ideal transplant conditioning has emerged, many of the MA and RIC studies used BU-based regimens and used a recipient age cutoff of 50–55 years for MA HCT. Similarly, there is no agreement on the use of induction or hypomethylating therapy before HCT, but azacitidine and decitabine are gaining increasing attention as a bridge to HCT. Until recently, the International Prognostic Scoring System (IPSS) dictated the use and timing of HCT. The WHO classification and WHO Prognostic Scoring System (WPSS) may be better suited in predicting the outcomes and should probably be incorporated in transplant algorithms. Most published MDS transplant series combine matched related donors (MRD) and matched unrelated donors (MUD). Umbilical cord blood (UCB) grafts will likely broaden the population of MDS patients eligible for allografting, but outcome data for MDS are scant. At this time, it is reasonable to consider the availability of an MRD or MUD as separate from an UCB graft in the decision of transplantation for MDS. The development of RIC, improvements in supportive therapy and alternative donor selection will provide better OS for MDS patients undergoing transplantation. Simultaneously, better understanding and medical therapy of MDS are leading us to re-examine patient selection and the timing of HCT. The results of HCT for MDS continue to improve together with the outlook of patients afflicted with myelodysplasia.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Ma X, Does M, Raza A, Mayne ST . Myelodysplastic syndromes: incidence and survival in the United States. Cancer 2007; 109: 1536–1542.
Silverman LR, Demakos EP, Peterson BL, Kornblith AB, Holland JC, Odchimar-Reissig R et al. Randomized controlled trial of azacitidine in patients with the myelodysplastic syndrome: a study of the Cancer and Leukemia Group B. J Clin Oncol 2002; 20: 2429–2440.
Silverman LR, McKenzie DR, Peterson BL, Holland JF, Backstrom JT, Beach CL et al. Further analysis of trials with azacitidine in patients with myelodysplastic syndrome: studies 8421, 8921, and 9221 by the Cancer and Leukemia Group B. J Clin Oncol 2006; 24: 3895–3903.
Fenaux P, Mufti GJ, Santini V, Finelli C, Giagounidis A, Schoch R et al. Azacitidine treatment prolongs overall survival in higher-risk MDS patients compared with conventional care regimens: results of AZA-001 phase III study. Blood 2007; 110: abstract 817.
Kantarjian H, Issa J-P, Rosenfeld CS, Bennett JM, Albitar M, DiPersio J et al. Decitabine improves patient outcomes in myelodysplastic syndromes: results of a phase III randomized study. Cancer 2006; 106: 1794–1803.
List A, Kurtin S, Roe DJ, Buresh A, Mahadevan D, Fuchs D et al. Efficacy of lenalidomide in myelodysplastic syndromes. N Engl J Med 2005; 352: 549–557.
List A, Dewald G, Bennett J, Giagounidis A, Raza A, Feldman E et al. Lenalidomide in the myelodysplastic syndrome with chromosome 5q deletion. N Engl J Med 2006; 355: 1456–1465.
Witherspoon RP, Deeg HJ, Storer B, Anasetti C, Storb R, Appelbaum FR . Hematopoietic stem-cell transplantation for treatment-related leukemia or myelodysplasia. J Clin Oncol 2001; 19: 2134–2141.
Castro-Malaspina H, Harris RE, Gajewski J, Ramsay N, Collins R, Dharan B et al. Unrelated donor marrow transplantation for myelodysplastic syndromes: outcome analysis in 510 transplants facilitated by the National Marrow Donor Program. Blood 2002; 99: 1943–1951.
Deeg HJ, Storer B, Slattery JT, Anasetti C, Doney KC, Hansen JA et al. Conditioning with targeted busulfan and cyclophosphamide for hemopoietic stem cell transplantation from related and unrelated donors in patients with myelodysplastic syndrome. Blood 2002; 100: 1201–1207.
Wallen H, Gooley TA, Deeg HJ, Pagel JM, Press OW, Appelbaum FR et al. Ablative allogeneic hematopoietic cell transplantation in adults 60 years of age and older. J Clin Oncol 2005; 23: 3439–3446.
Cutler CS, Lee SJ, Greenberg P, Deeg HJ, Perez WS, Anasetti C et al. A decision analysis of allogeneic bone marrow transplantation for the myelodysplastic syndromes: delayed transplantation for low-risk myelodysplasia is associated with improved outcome. Blood 2004; 104: 579–585.
Kantarjian H, O'Brien S, Ravandi F, Cortes J, Shan J, Bennett JM et al. Proposal for a new risk model in myelodysplastic syndrome that accounts for events not considered in the original international prognostic scoring system. Cancer 2008; 113: 1351–1361.
Alessandrino EP, Della Porta MG, Bacigalupo A, Van Lint MT, Falda M, Onida F et al. WHO classification and WPSS predict post transplant outcome in patients with myelodysplastic syndrome: a study from the GITMO (gruppo italiano trapianto di midollo osseo). Blood 2008; 112: 895–902.
de Witte T, Suciu S, Verhoef G, Labar B, Archimbaud E, Aul C et al. Intensive chemotherapy followed by allogeneic or autologous stem cell transplantation for patients with myelodysplastic syndromes (MDSs) and acute myeloid leukemia following MDS. Blood 2001; 98: 2326–2331.
Nakai K, Kanda Y, Fukuhara S, Sakamaki H, Okamoto S, Kodera Y et al. Value of chemotherapy before allogeneic hematopoietic stem cell transplantation from an HLA-identical sibling donor for myelodysplastic syndrome. Leukemia 2005; 19: 396–401.
Kahl C, Storer BE, Sandmaier BM, Mielcarek M, Maris MB, Blume KG et al. Relapse risk in patients with malignant disease given allogeneic hematopoietic cell transplantation after nonmyeloablative conditioning. Blood 2007; 110: 2744–2748.
Kantarjian HM, O'Brien S, Huang X, Garcia-Manero G, Ravandi F, Cortes J et al. Survival advantage with decitabine versus intensive chemotherapy in patients with higher risk myelodysplastic syndrome: comparison with historical experience. Cancer 2007; 109: 1133–1137.
De Padua Silva L, de Lima M, Kantarjian H, Champlin R, Faderl S, Giralt S et al. Outcome of allogeneic stem cell transplantation after hypomethylating therapy with 2′-deoxy-5 azacytidine for patients with myelodysplastic syndrome. Blood 2007; 110: abstract 1468.
Field T, Perkins J, Alsina M, Ayala E, Fernandez HF, Janssen W et al. Pre-transplant 5-Azacitidine may improve outcome of allogeneic hematopoietic cell transplantation (HCT) in patients with myelodysplastic syndrome (MDS). Blood 2006; 108: abstract 3664.
SEER Cancer Statistics Review 1975–2004. National Cancer Institute.
Ditschkowski M, Elmaagacli AH, Trenschel R, Steckel NK, Koldehoff M, Beelen DW . Myeloablative allogeneic hematopoietic stem cell transplantation in elderly patients. Clin Transplant 2006; 20: 127–131.
Du W, Dansey R, Abella EM, Baynes R, Peters WP, Klein J et al. Successful allogeneic bone marrow transplantation in selected patients over 50 years of age—a single institution's experience. Bone Marrow Transplant 1998; 21: 1043–1047.
Alyea EP, Kim HT, Ho V, Cutler C, Gribben J, DeAngelo DJ et al. Comparative outcome of nonmyeloablative and myeloablative allogeneic hematopoietic cell transplantation for patients older than 50 years of age. Blood 2005; 105: 1810–1814.
Stem Cell Trialists' Collaborative Group. Allogeneic peripheral blood stem-cell compared with bone marrow transplantation in the management of hematologic malignancies: an individual patient data meta-analysis of nine randomized trials. J Clin Oncol 2005; 23: 5074–5087.
Cutler C, Giri S, Jeyapalan S, Paniagua D, Viswanathan A, Antin JH . Acute and chronic graft-versus-host disease after allogeneic peripheral-blood stem-cell and bone marrow transplantation: a meta-analysis. J Clin Oncol 2001; 19: 3685–3691.
Dey BR, Shaffer J, Yee AJ, McAfee S, Caron M, Power K et al. Comparison of outcomes after transplantation of peripheral blood stem cells versus bone marrow following an identical nonmyeloablative conditioning regimen. Bone Marrow Transplant 2007; 40: 19–27.
Guardiola P, Runde V, Bacigalupo A, Ruutu T, Locatelli F, Boogaerts MA et al. Retrospective comparison of bone marrow and granulocyte colony-stimulating factor-mobilized peripheral blood progenitor cells for allogeneic stem cell transplantation using HLA identical sibling donors in myelodysplastic syndromes. Blood 2002; 99: 4370–4378.
Ducastelle S, Adès L, Gardin C, Dombret H, Prébet T, Deconinck E et al. Long-term follow-up of autologous stem cell transplantation after intensive chemotherapy in patients with myelodysplastic syndrome or secondary acute myeloid leukemia. Haematologica 2006; 91: 373–376.
de Witte T, Brand R, van Biezen A, Delforge M, Biersack H, Or R et al. The role of stem cell source in autologous hematopoietic stem cell transplantation for patients with myelodysplastic syndromes. Haematologica 2006; 91: 750–756.
Kroger N, Brand R, van Biezen A, Cahn J-Y, Slavin S, Blaise D et al. Autologous stem cell transplantation for therapy-related acute myeloid leukemia and myelodysplastic syndrome. Bone Marrow Transplant 2006; 37: 183–189.
de Witte T, Hermans J, Vossen J, Bacigalupo A, Meloni G, Jacobsen N et al. Haematopoietic stem cell transplantation for patients with myelodysplastic syndromes and secondary acute myeloid leukaemias: a report on behalf of the chronic leukaemia working party of the European Group for Blood and Marrow Transplantation. Br J Haematol 2000; 110: 620–630.
Al-Ali HK, Brand R, van Biezen A, Finke J, Boogaerts M, Fauser AA et al. A retrospective comparison of autologous and unrelated donor hematopoietic cell transplantation in myelodysplastic syndrome and secondary acute myeloid leukemia: a report on behalf of the Chronic Leukemia Working Party of the European Group for Blood and Marrow Transplantation (EBMT). Leukemia 2007; 21: 1945–1951.
Deeg HJ, Shulman HM, Anderson JE, Bryant EM, Gooley TA, Slattery JT et al. Allogeneic and syngeneic marrow transplantation for myelodysplastic syndrome in patients 55 to 66 years of age. Blood 2000; 95: 1188–1194.
Yakoub-Agha I, de La Salmoniere P, Ribaud P, Sutton L, Wattel E, Kuentz M et al. Allogeneic bone marrow transplantation for therapy-related myelodysplastic syndrome and acute myeloid leukemia: a long-term study of 70 patients—Report of the French Society of Bone Marrow Transplantation. J Clin Oncol 2000; 18: 963–971.
Bibawi S, Abi-Said D, Fayad L, Anderlini P, Ueno NT, Mehra R et al. Thiotepa, busulfan, and cyclophosphamide as a preparative regimen for allogeneic transplantation for advanced myelodysplastic syndrome and acute myelogenous leukemia. Am J Hematol 2001; 67: 227–233.
de Witte T, Pikkemaat F, Hermans J, van Biezen A, Mackinnan S, Cornelissen J et al. Genotypically nonidentical related donors for transplantation of patients with myelodysplastic syndromes: comparison with unrelated donor transplantation and autologous stem cell transplantation. Leukemia 2001; 15: 1878–1884.
Jurado M, Deeg HJ, Storer B, Anasetti C, Anderson JE, Bryant E et al. Hematopoietic stem cell transplantation for advanced myelodysplastic syndrome after conditioning with busulfan and fractionated total body irradiation is associated with low relapse rate but considerable nonrelapse mortality. Biol Blood Marrow Transplant 2002; 8: 161–169.
Sierra J, Perez WS, Rozman C, Carreras E, Klein JP, Rizzo JD et al. Bone marrow transplantation from HLA-identical siblings as treatment for myelodysplasia. Blood 2002; 100: 1997–2004.
Kojima R, Kami M, Kanda Y, Kusumi E, Kishi Y, Tanaka Y et al. Comparison between reduced intensity and conventional myeloablative allogeneic stem-cell transplantation in patients with hematologic malignancies aged between 50 and 59 years. Bone Marrow Transplant 2005; 36: 667–674.
Solomon SR, Savani BN, Childs R, Montero A, Boss C, Read EJ et al. Improved outcome for peripheral blood stem cell transplantation for advanced primary myelodysplastic syndrome. Biol Blood Marrow Transplant 2005; 11: 619–626.
Wong R, Shahjahan M, Wang X, Thall PF, de Lima M, Khouri I et al. Prognostic factors for outcomes of patients with refractory or relapsed acute myelogenous leukemia or myelodysplastic syndromes undergoing allogeneic progenitor cell transplantation. Biol Blood Marrow Transplant 2005; 11: 108–114.
Alyea EP, Kim HT, Ho V, Cutler C, DeAngelo DJ, Stone R et al. Impact of conditioning regimen intensity on outcome of allogeneic hematopoietic cell transplantation for advanced acute myelogenous leukemia and myelodysplastic syndrome. Biol Blood Marrow Transplant 2006; 12: 1047–1055.
Martino R, Iacobelli S, Brand R, Jansen T, van Biezen A, Finke J et al. Retrospective comparison of reduced-intensity conditioning and conventional high-dose conditioning for allogeneic hematopoietic stem cell transplantation using HLA-identical sibling donors in myelodysplastic syndromes. Blood 2006; 108: 836–846.
Scott BL, Sandmaier BM, Storer B, Maris MB, Sorror ML, Maloney DG et al. Myeloablative vs nonmyeloablative allogeneic transplantation for patients with myelodysplastic syndrome or acute myelogenous leukemia with multilineage dysplasia: a retrospective analysis. Leukemia 2006; 20: 128–135.
Shimoni A, Hardan I, Shem-Tov N, Yeshurun M, Yerushalmi R, Avigdor A et al. Allogeneic hematopoietic stem-cell transplantation in AML and MDS using myeloablative versus reduced-intensity conditioning: the role of dose intensity. Leukemia 2006; 20: 322–328.
Yakoub-Agha I, Mesnil F, Kuentz M, Boiron JM, Ifrah N, Milpied N et al. Allogeneic marrow stem-cell transplantation from human leukocyte antigen-identical siblings versus human leukocyte antigen-allelic-matched unrelated donors (10/10) in patients with standard-risk hematologic malignancy: a prospective study from the French Society of Bone Marrow Transplantation and Cell Therapy. J Clin Oncol 2006; 24: 5695–5702.
Chang CK, Storer BE, Scott BL, Bryant EM, Shulman HM, Flowers ME et al. Hematopoietic cell transplantation in patients with myelodysplastic syndrome or acute myeloid leukemia arising from myelodysplastic syndrome: Similar outcomes in patients with de novo disease and disease following prior therapy or antecedent hematologic disorders. Blood 2007; 110: 1379–1387.
Flynn CM, Hirsch B, DeFor T, Barker JN, Miller JS, Wagner JE et al. Reduced intensity compared with high dose conditioning for allotransplantation in acute myeloid leukemia and myelodysplastic syndrome: a comparative clinical analysis. Am J Hematol 2007; 82: 867–872.
Maruyama D, Fukuda T, Kato R, Yamasaki S, Usui E, Morita-Hoshi Y et al. Comparable antileukemia/lymphoma effects in nonremission patients undergoing allogeneic hematopoietic cell transplantation with conventional cytoreductive or reduced-intensity regimen. Biol Blood Marrow Transplant 2007; 13: 932–941.
Martino R, Valcarcel D, Brunet S, Sureda A, Sierra J . Comparable non-relapse mortality and survival after HLA-identical sibling blood stem cell transplantation with reduced or conventional-intensity preparative regimens for high-risk myelodysplasia or acute myeloid leukemia in first remission. Bone Marrow Transplant 2008; 41: 33–38.
Nevill TJ, Hogge DE, Toze CL, Nantel SH, Power MM, Abou Mourad YR et al. Predictors of outcome following myeloablative allo-SCT for therapy-related myelodysplastic syndrome and AML. Bone Marrow Transplant 2008; 42: 659–666.
Scott B, Deeg HJ, Storer B, Chauncey T, Petersdorf S, Slattery J et al. Targeted busulfan and cyclophosphamide as compared to busulfan and TBI as preparative regimens for transplantation in patients with advanced MDS or transformation to AML. Leuk Lymphoma 2004; 45: 2409–2417.
de Lima M, Anagnostopoulos A, Munsell M, Shahjahan M, Ueno N, Ippoliti C et al. Nonablative versus reduced-intensity conditioning regimens in the treatment of acute myeloid leukemia and high-risk myelodysplastic syndrome: dose is relevant for long-term disease control after allogeneic hematopoietic stem cell transplantation. Blood 2004; 104: 865–872.
Chan GW, Foss FM, Klein AK, Sprague K, Miller KB . Reduced-intensity transplantation for patients with myelodysplastic syndrome achieves durable remission with less graft-versus-host disease. Biol Blood Marrow Transplant 2003; 9: 753–759.
Kroger N, Bornhauser M, Ehninger G, Schwerdtfeger R, Biersack H, Sayer HG et al. Allogeneic stem cell transplantation after a fludarabine/busulfan-based reduced-intensity conditioning in patients with myelodysplastic syndrome or secondary acute myeloid leukemia. Ann Hematol 2003; 82: 336–342.
Taussig DC, Davies AJ, Cavenagh JD, Oakervee H, Syndercombe-Court D, Kelsey S et al. Durable remissions of myelodysplastic syndrome and acute myeloid leukemia after reduced-intensity allografting. J Clin Oncol 2003; 21: 3060–3065.
Wong R, Giralt SA, Martin T, Couriel DR, Anagnostopoulos A, Hosing C et al. Reduced-intensity conditioning for unrelated donor hematopoietic stem cell transplantation as treatment for myeloid malignancies in patients older than 55 years. Blood 2003; 102: 3052–3059.
Ho AYL, Pagliuca A, Kenyon M, Parker JE, Mijovic A, Devereux S et al. Reduced-intensity allogeneic hematopoietic stem cell transplantation for myelodysplastic syndrome and acute myeloid leukemia with multilineage dysplasia using fludarabine, busulphan, and alemtuzumab (FBC) conditioning. Blood 2004; 104: 1616–1623.
Malladi RK, Peniket AJ, Norton AE, Campbell AJ, Collins GP, Samol J et al. Favourable outcome for patients with myeloid disorders treated with fludarabine-melphalan reduced-intensity conditioning and allogeneic bone marrow stem cell transplantation without the use of T-lymphocyte-depleting antibodies. Eur J Haematol 2004; 73: 85–92.
Gupta V, Daly A, Lipton JH, Hasegawa W, Chun K, Kamel-Reid S et al. Nonmyeloablative stem cell transplantation for myelodysplastic syndrome or acute myeloid leukemia in patients 60 years or older. Biol Blood Marrow Transplant 2005; 11: 764–772.
Schmid C, Schleuning M, Ledderose G, Tischer J, Kolb H-J . Sequential regimen of chemotherapy, reduced-intensity conditioning for allogeneic stem-cell transplantation, and prophylactic donor lymphocyte transfusion in high-risk acute myeloid leukemia and myelodysplastic syndrome. J Clin Oncol 2005; 23: 5675–5687.
Tauro S, Craddock C, Peggs K, Begum G, Mahendra P, Cook G et al. Allogeneic stem-cell transplantation using a reduced-intensity conditioning regimen has the capacity to produce durable remissions and long-term disease free survival in patient with high-risk acute myeloid leukemia and myelodysplasia. J Clin Oncol 2005; 23: 9387–9393.
Hallemeier CL, Girgis MD, Blum WG, Brown RA, Khoury HJ, Devine SM et al. Long-term remissions in patients with myelodysplastic syndrome and secondary acute myelogenous leukemia undergoing allogeneic transplantation following a reduced intensity conditioning regimen of 550 cGy total body irradiation and cyclophosphamide. Biol Blood Marrow Transplant 2006; 12: 749–757.
Lim ZY, Ho AYL, Ingram W, Kenyon M, Pearce L, Czepulkowski B et al. Outcomes of alemtuzumab-based reduced intensity conditioning stem cell transplantation using unrelated donors for myelodysplastic syndromes. Br J Haematol 2006; 135: 201–209.
Lim ZY, Pearce L, Ho AYL, Barber L, Ingram W, Usai M et al. Delayed attainment of full donor chimaerism following alemtuzumab-based reduced-intensity conditioning haematopoietic stem cell transplantation for acute myeloid leukaemia and myelodysplastic syndromes is associated with improved outcomes. Br J Haematol 2007; 138: 517–526.
Nakamura R, Rodriguez R, Palmer J, Stein A, Naing A, Tsai N et al. Reduced-intensity conditioning for allogeneic hematopoietic stem cell transplantation with fludarabine and melphalan is associated with durable disease control in myelodysplastic syndrome. Bone Marrow Transplant 2007; 40: 843–850.
Oran B, Giralt S, Saliba R, Hosing C, Popat U, Khouri I et al. Allogeneic hematopoietic stem cell transplantation for the treatment of high-risk acute myelogenous leukemia and myelodysplastic syndrome using reduced-intensity conditioning with fludarabine and melphalan. Biol Blood Marrow Transplant 2007; 13: 454–462.
Strahm B, Locatelli F, Bader P, Ehlert K, Kremens B, Zintl F et al. Reduced intensity conditioning in unrelated donor transplantation for refractory cytopenia in childhood. Bone Marrow Transplant 2007; 40: 329–333.
Huisman C, Meijer E, Petersen EJ, Lokhorst HM, Verdonck LF . Hematopoietic stem cell transplantation after reduced intensity conditioning in acute myelogenous leukemia patients older than 40 years. Biol Blood Marrow Transplant 2008; 14: 181–186.
Laport GG, Sandmaier BM, Storer BE, Scott BL, Stuart MJ, Lange T et al. Reduced-intensity conditioning followed by allogeneic hematopoietic cell transplantation for adult patients with myelodysplastic syndrome and myeloproliferative disorders. Biol Blood Marrow Transplant 2008; 14: 246–255.
Valcarcel D, Martino R, Caballero D, Martin J, Ferra C, Nieto JB et al. Sustained remissions of high-risk acute myeloid leukemia and myelodysplastic syndrome after reduced-intensity conditioning allogeneic hematopoietic transplantation: Chronic graft-versus-host disease is the strongest factor improving survival. J Clin Oncol 2008; 26: 577–584.
Marks R, Potthoff K, Hahn J, Ihorst G, Bertz H, Spyridonidis A et al. Reduced-toxicity conditioning with fludarabine, BCNU, and melphalan in allogeneic hematopoietic cell transplantation: particular activity against advanced hematologic malignancies. Blood 2008; 112: 415–425.
Laughlin MJ, Eapen M, Rubinstein P, Wagner JE, Zhang M-J, Champlin RE et al. Outcomes after transplantation of cord blood or bone marrow from unrelated donors in adults with leukemia. N Engl J Med 2004; 351: 2265–2275.
Ooi J, Iseki T, Takahashi S, Tomonari A, Ishii K, Takasugi K et al. Unrelated cord blood transplantation for adult patients with advanced myelodysplastic syndrome. Blood 2003; 101: 4711–4713.
Majhail NS, Brunstein CG, Tomblyn M, Thomas AJ, Miller JS, Arora M . Reduced-intensity allogeneic transplant in patients older than 55 years: unrelated umbilical cord blood is safe and effective for patients without a matched related donor. Biol Blood Marrow Transplant 2008; 14: 282–289.
Andersson BS, de Lima M, Thall PF, Wang X, Couriel D, Korbling M et al. Once daily IV busulfan and fludarabine (IV Bu-Flu) compares favorably with IV busulfan and cyclophosphamide (IV BuCy2) as pretransplant conditioning therapy in AML/MDS. Biol Blood Marrow Transplant 2008; 14: 672–684.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kindwall-Keller, T., Isola, L. The evolution of hematopoietic SCT in myelodysplastic syndrome. Bone Marrow Transplant 43, 597–609 (2009). https://doi.org/10.1038/bmt.2009.28
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2009.28
Keywords
This article is cited by
-
Meta-analysis of the benefit of hypomethylating agents before allogeneic hematopoietic stem cell transplantation in myelodysplastic syndromes
Clinical and Experimental Medicine (2021)
-
Hypomethylating agents for patients with myelodysplastic syndromes prior to hematopoietic stem cell transplantation: a systematic review and meta-analysis
Annals of Hematology (2019)
-
Impending relapse of myelodysplastic syndrome after allogeneic transplant is difficult to diagnose and requires a multi-modal approach
BMC Clinical Pathology (2017)
-
Minimal residual disease monitoring and preemptive immunotherapy in myelodysplastic syndrome after allogeneic hematopoietic stem cell transplantation
Annals of Hematology (2016)
-
Feasibility of hypomethylating agents followed by allogeneic hematopoietic cell transplantation in patients with myelodysplastic syndrome
Bone Marrow Transplantation (2012)