Abstract
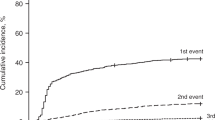
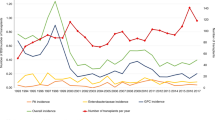
The incidence of bacteremia following hemopoietic SCT (HSCT) changes over time from the procedure. The first 30 days have the highest incidence, both in autologous and allogeneic HSCT recipients. In the following periods, bacteremia is a frequent complication in allogeneic HSCT, especially from alternative donors. Gram-positive cocci represent the most frequent cause of single-agent bacteremia. Knowledge of epidemiology (incidence and etiology) of bacteremias following HSCT is pivotal for planning management strategies (prevention, diagnosis and therapy) that must be distinct in the different post-transplant period.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Ninin E, Milpied N, Moreau P, André-Richet B, Morineau N, Mahé B et al. Longitudinal study of bacterial, viral, and fungal infections in adult recipients of bone marrow transplants. Clin Infect Dis 2001; 33: 41–47.
Romano V, Castagnola E, Dallorso S, Lanino E, Calvi A, Silvestro S et al. Bloodstream infections can develop late (after day 100) and/or in the absence of neutropenia in children receiving allogeneic bone marrow transplantation. Bone Marrow Transplant 1999; 23: 271–275.
Benjamin DK, Miller WC, Bayliff S, Martel L, Alexander KA, Martin PL et al. Infections diagnosed in the first year after pediatric stem cell transplantation. Pediatr Infect Dis J 2002; 21: 227–234.
Sonis ST, Oster G, Fuchs H, Bellm L, Bradford WZ, Edelsberg J et al. Oral mucositis and the clinical and economic outcomes of hematopoietic stem-cell transplantation. J Clin Oncol 2001; 19: 2201–2205.
Sepkowitz KA . Risk and epidemiology of infections after allogeneic hemopoietic stem cell transplantation. In: Bowden RA, Ljungman P, Paya CV, (eds). Transplant Infections. Lippincott Willians & Wilkins: Philadelphia, 2003, pp 31–38.
Anaissie E, Nucci M . Risk and epidemiology of infections after autologous hemopoietic stem cell transplantation. In: Bowden RA, Ljungman P, Paya CV, (eds). Transplant Infections. Lippincott Willians & Wilkins: Philadelphia, 2003, pp. 39–50.
Castagnola E, Conte M, Parodi S, Papio F, Caviglia I, Haupt R . Incidence of bacteremias and invasive mycoses in children with high risk neuroblastoma. Pediatr Blood Cancer 2007; 49: 672–677.
Barker JN, Hough RE, van Burik JA, DeFor TE, MacMillan ML, O’Brien MR et al. Serious infections after unrelated donor transplantation in 136 children: impact of stem cell source. Biol Blood Marrow Transplant 2005; 11: 362–370.
Nagatoshi Y, Kawano Y, Okamura J . Comparison of the outcomes of allogeneic bone marrow transplantation from partially mismatched related donors, matched sibling donors, and matched unrelated donors in Japanese pediatric patients: a single center result. Pediatr Transplant 2004; 8: 260–266.
Nucci M, Andrade F, Vigorito A, Trabasso P, Aranha JF, Maiolino A et al. Infectious complications in patients randomized to receive allogeneic bone marrow or peripheral blood transplantation. Transpl Infect Dis 2003; 5: 167–173.
van Kraaij MG, Verdonck LF, Rozenberg-Arska M, Dekker AW . Early infections in adults undergoing matched related and matched unrelated/mismatched donor stem cell transplantation: a comparison of incidence. Bone Marrow Transplant 2002; 30: 303–309.
Castagnola E, Molinari AC, Fratino G, Viscoli C . Conditions associated with infections of indwelling central venous catheters in cancer patients: a summary. Br J Haematol 2003; 121: 233–239.
Fratino G, Molinari AC, Parodi S, Longo S, Saracco P, Castagnola E et al. Central venous catheter-related complications in children with oncological/hematological diseases: an observational study of 418 devices. Ann Oncol 2005; 16: 648–654.
Viscoli C, Castagnola E . Prophylaxis and empirical therapy for infection in cancer patients. In: Mandell GL, Bennett JE, Doolin R, (eds). Principles and Practice of Infectious Diseases. Churchill Livingstone: Philadelphia, 2005, pp 3442–3462.
Viscoli C, Castagnola E, Giacchino M, Cesáro S, Properzi E, Tucci F et al. Bloodstream infections in children with cancer: a multicentre surveillance study of the Italian Association of Paediatric Haematology and Oncology. Supportive Therapy Group–Infectious Diseases Section. Eur J Cancer 1999; 35: 770–774.
Engelhard D, Geller N, Paterson DL . Gram-positive and Gram-negative infections after hemopoietic stem cell or solid organ transplantation. In: Bowden RA, Ljungman P, Paya CV, (eds). Transplant Infections. Lippincott Willians & Wilkins: Philadelphia, 2003, pp 225–249.
Engelhard D, Cordonnier C, Shaw PJ, Parkalli T, Guenther C, Martino R et al. Early and late invasive pneumococcal infection following stem cell transplantation: a European Bone Marrow Transplantation survey. Br J Haematol 2002; 117: 444–450.
Bucaneve G, Micozzi A, Menichetti F, Martino P, Dionisi MS, Martinelli G et al. Levofloxacin to prevent bacterial infection in patients with cancer and neutropenia. N Engl J Med 2005; 353: 977–987.
Leibovici L, Paul M, Cullen M, Bucaneve G, Gafter-Gvili A, Fraser A et al. Antibiotic prophylaxis in neutropenic patients: new evidence, practical decisions. Cancer 2006; 107: 1743–1751.
Castagnola E, Fioredda F . Prevention of life-threatening infections due to encapsulated bacteria in children with hyposplenia or asplenia: a brief review of current recommendations for practical purposes. Eur J Haematol 2003; 71: 319–326.
Ljungman P, Engelhard D, de la Cámara R, Einsele H, Locasciulli A, Martino R et al. Vaccination of stem cell transplant recipients: recommendations of the Infectious Diseases Working Party of the EBMT. Bone Marrow Transplant 2005; 35: 737–746.
Author information
Authors and Affiliations
Corresponding author
Additional information
Conflict of interest
None of the authors declared any financial interests.
Rights and permissions
About this article
Cite this article
Castagnola, E., Faraci, M., Moroni, C. et al. Bacteremias in children receiving hemopoietic SCT. Bone Marrow Transplant 41 (Suppl 2), S104–S106 (2008). https://doi.org/10.1038/bmt.2008.66
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2008.66
Keywords
This article is cited by
-
MBI-LCBI and CLABSI: more than scrubbing the line
Bone Marrow Transplantation (2019)
-
Safety and feasibility of outpatient autologous stem cell transplantation in pediatric patients with primary central nervous system tumors
Bone Marrow Transplantation (2019)
-
The safety and feasibility of probiotics in children and adolescents undergoing hematopoietic cell transplantation
Bone Marrow Transplantation (2016)
-
Bloodstream infection in paediatric cancer centres—leukaemia and relapsed malignancies are independent risk factors
European Journal of Pediatrics (2015)