Abstract
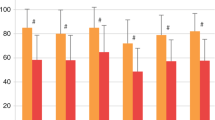
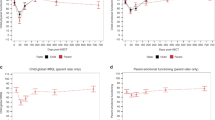
In this cross-sectional study, we compared the quality of life (QOL) in transfusion-dependent thalassemic patients who survived matched sibling hematopoietic SCT (HSCT, n=24) with patients treated conventionally with transfusion and iron chelation (n=74). WHOQOL-BREF(HK) and PedsQL questionnaires were administered to patients aged >18 years and 5–12 years, respectively. Patients aged 12–18 years received both questionnaires. WHOQOL-BREF(HK) revealed post transplant patients rated overall health better than those treated conventionally (score 3.67 vs 3.06, P=0.01). They are less dependent on medical aids (3.87 vs 2.96, P=0.006), having higher activity level (4.00 vs 3.36, P=0.026) and better personal relationships (4.13 vs 3.69, P=0.014). Physical health domain score was better (75.20 vs 63.94, P=0.007). These differences remained significant after adjustment for comorbidities. PedsQL revealed post transplant patients rated better for running (3.53 vs 2.72, P=0.001) and sports (3.20 vs 2.64, P=0.038), even after adjustment for comorbidities, but were less satisfied for school absence to attend hospital (2.53 vs 3.29, P=0.03). Post transplant patients were significantly more likely to consider marriage (100 vs 75.7%, P=0.033), but not childbearing (66.7 vs 51.4%, P=0.28). In conclusion, transplanted thalassemic patients enjoy better QOL, mainly in physical health, compared with conventionally treated patients. This information is important to patients considering HSCT.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Hussain MA, Green N, Flynn DM, Hussein S, Hoffbrand AV . Subcutaneous infusion and intramuscular injection of desferrioxamine in patients with transfusional iron overload. Lancet 1976; 2: 1278–1280.
Olivieri NF, Brittenham GM . Iron-chelating therapy and the treatment of thalassemia. Blood 1997; 89: 739–761.
Ismail A, Campbell MJ, Ibrahim HM, Jones GL . Health related quality of life in Malaysian children with thalassaemia. Health Qual Life Outcomes 2006; 4: 39.
Telfer P, Constantinidou G, Andreou P, Christou S, Modell B, Angastiniotis M . Quality of life in thalassemia. Ann NY Acad Sci 2005; 1054: 273–282.
Goldbeck L, Baving A, Kohne E . [Psychosocial aspects of beta-thalassemia: distress, coping and adherence]. Klinische Padiatrie 2000; 212: 254–259.
Aydinok Y, Erermis S, Bukusoglu N, Yilmaz D, Solak U . Psychosocial implications of thalassemia major. Pediatr Int 2005; 47: 84–89.
Tsiantis J, Dragonas T, Richardson C, Anastasopoulos D, Masera G, Spinetta J . Psychosocial problems and adjustment of children with beta-thalassemia and their families. Eur Child Adolesc Psychiatry 1996; 5: 193–203.
Mikelli A, Tsiantis J . Brief report: depressive symptoms and quality of life in adolescents with b-thalassaemia. J Adolesc 2004; 27: 213–216.
Lucarelli G, Galimberti M, Polchi P, Angelucci E, Baronciani D, Giardini C et al. Bone marrow transplantation in patients with thalassemia. N Engl J Med 1990; 322: 417–421.
Hongeng S, Pakakasama S, Chaisiripoomkere W, Chuansumrit A, Sirachainan N, Ungkanont A et al. Outcome of transplantation with unrelated donor bone marrow in children with severe thalassaemia. Bone Marrow Transplant 2004; 33: 377–379.
Pakakasama S, Hongeng S, Chaisiripoomkere W, Chuansumrit A, Sirachainun N, Jootar S . Allogeneic peripheral blood stem cell transplantation in children with homozygous beta-thalassemia and severe beta-thalassemia/hemoglobin E disease. J Pediatr Hematol Oncol 2004; 26: 248–252.
Khojasteh HN, Zakerinia M, Ramzi M, Haghshenas M . Bone marrow transplantation in thalassaemia patients in Shiraz, Islamic Republic of Iran. Eastern Mediterr Health J 2001; 7: 835–837.
Nuss SL, Wilson ME . Health-related quality of life following hematopoietic stem cell transplant during childhood. J Pediatr Oncol Nurs 2007; 24: 106–115.
Caocci G, Pisu S, Argiolu F, Giardini C, Locatelli F, Vacca A et al. Decision-making in adult thalassemia patients undergoing unrelated bone marrow transplantation: quality of life, communication and ethical issues. Bone Marrow Transplant 2006; 37: 165–169.
Lucarelli G, Andreani M, Angelucci E . The cure of thalassemia by bone marrow transplantation. Blood Rev 2002; 16: 81–85.
Piga A, Longo F, Voi V, Facello S, Miniero R, Dresow B . Late effects of bone marrow transplantation for thalassemia. Ann NY Acad Sci 1998; 850: 294–299.
Heiney SP, Neuberg RW, Myers D, Bergman LH . The aftermath of bone marrow transplant for parents of pediatric patients: a post-traumatic stress disorder. Oncol Nurs Forum 1994; 21: 843–847.
Caro JJ, Ward A, Green TC, Huybrechts K, Arana A, Wait S et al. Impact of thalassemia major on patients and their families. Acta Haematol 2002; 107: 150–157.
Saeed N . My life. UK Thalassaemia Soc Matters 2004; 99: 10.
Arboretti R, Tognoni G, Alberti D . Pharmacosurveillance and quality of care of thalassaemic patients. A large scale epidemiological survey. Eur J Clin Pharmacol 2001; 56: 915–922.
Ratip S, Skuse D, Porter J, Wonke B, Yardumian A, Modell B . Psychosocial and clinical burden of thalassaemia intermedia and its implications for prenatal diagnosis. Arch Dis Child 1995; 72: 408–412.
Smiley M . Beta thalassaemia in Papua New Guinea. Ann Trop Paediatr 1986; 6: 175–177.
Abetz L, Baladi JF, Jones P, Rofail D . The impact of iron overload and its treatment on quality of life: results from a literature review. Health Qual Life Outcomes 2006; 4: 73.
Basran RK, Fasson FF, Shaw D, Olivieri NF . Assessment of the relative quality of life in patients receiving subcutaneous deferoxamine and the orally active iron chelating agent L1. Blood 1994; 84: 261a.
Cappellini MD, Cohen A, Piga A, Bejaoui M, Perrotta S, Agaoglu L et al. A phase 3 study of deferasirox (ICL670), a once-daily oral iron chelator, in patients with beta-thalassemia. Blood 2006; 107: 3455–3462.
Delea TE, Sofrygin O, Thomas SK, Baladi JF, Phatak PD, Coates TD . Cost effectiveness of once-daily oral chelation therapy with deferasirox versus infusional deferoxamine in transfusion-dependent thalassaemia patients: US healthcare system perspective. Pharmacoeconomics 2007; 25: 329–342.
Acknowledgements
This project was supported by research fund from Hong Kong Children's Thalassemia Foundation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cheuk, D., Mok, A., Lee, A. et al. Quality of life in patients with transfusion-dependent thalassemia after hematopoietic SCT. Bone Marrow Transplant 42, 319–327 (2008). https://doi.org/10.1038/bmt.2008.165
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2008.165
Keywords
This article is cited by
-
Magnetic resonance imaging assessment of the changes of cardiac and hepatic iron load in thalassemia patients before and after hematopoietic stem cell transplantation
Scientific Reports (2023)
-
Health-related quality of life among thalassemia patients in Bangladesh using the SF-36 questionnaire
Scientific Reports (2023)
-
Long-term health-related quality of life in patients with β-thalassemia after unrelated hematopoietic stem cell transplantation
Bone Marrow Transplantation (2022)
-
Health-related quality of life in pediatric patients with β-thalassemia major after hematopoietic stem cell transplantation
Bone Marrow Transplantation (2022)
-
Anxiety, depression, and mental health-related quality of life in survivors of pediatric allogeneic hematopoietic stem cell transplantation: a systematic review
Bone Marrow Transplantation (2020)