Abstract
Background:
It is important to regularly update survival estimates of patients with malignant mesothelioma as prognosis may vary according to epidemiologic factors and diagnostic and therapeutic management.
Methods:
We assessed overall (baseline) survival as well as related prognostic variables in a large cohort of 1353 patients with a confirmed diagnosis of malignant mesothelioma between 2005 and 2008.
Results:
About 50% of the patients were 70 years or older at diagnosis and the median latency time since start of asbestos exposure was 49 years. One year after diagnosis, 47% of the patients were alive, 20% after 2 years and 15% after 3 years. Prognostic variables independently associated with worse survival were: older age (HR=1.04 per year 95% CI (1.03–1.06)), sarcomatoid subtype (HR=2.45 95% CI (2.06–2.90)) and non-pleural localisation (HR=1.67 95% CI (1.26–2.22)).
Conclusion:
Survival of patients with malignant mesothelioma is still limited and depends highly on patient age, mesothelioma subtype and localisation. In addition, a substantial part of the patients had a long latency time between asbestos exposure and diagnosis.
Similar content being viewed by others
Main
The prognosis of patients with malignant mesothelioma is usually poor. However, a small fraction of patients is still alive 2 years after diagnosis. Differences in survival are associated with age at diagnosis, gender, health status, and tumour- and environment-related factors (Burgers and Damhuis, 2004).
Several studies have shown that asbestos exposure is negatively correlated with prognosis of patients with malignant mesothelioma, and therefore prognosis can vary across regions with different histories of industrial exposure to asbestos (Spirtas et al, 1988; Christensen et al, 2008). However, geographical differences might also reflect local approaches to diagnostic and therapeutic management. Any delay in making the diagnosis of malignant mesothelioma may have a major effect on survival estimates, when survival is as short as in mesothelioma patients and can affect associations between prognostic factors and survival. Differences in prognosis resulting from differences in asbestos exposure and management of malignant mesothelioma might be expected across countries and over time. Therefore, it is important to regularly, and regionally, update survival estimates, with the use of population-based studies.
The aim of this study, based on recent evidence from a large population-based cohort in the Netherlands, was threefold: (1) to update survival estimates of patients with malignant mesothelioma, (2) to identify general predictors of survival and (3) to assess the predictive accuracy of the combined prognostic factors for prolonged survival.
Patients and methods
Patients
This study involves retrospective analyses of an existing registry comprising 1353 patients with malignant mesothelioma who applied to the Dutch institute for asbestos victims and entered the process for getting financial compensation between 2005 and 2008 (Baas et al, 2006).
After application, the standard procedure is that the patients or relatives were visited at home by a qualified representative of the Dutch asbestos institute who further explained the application procedure and compensation scheme. Patients who decided to participate in this compensation scheme had to give written informed consent for the use of their clinical data and data regarding social status, occupational circumstances and income by the institute for assessing their case and for internal and external analyses and reporting. For such linking and use of data, the most strict rules and potential sanctions are applicable regarding confidentiality and anonymisation. Accordingly, in the present analyses, data were also completely anonymised. The diagnosis of mesothelioma was confirmed by pathologists from the Dutch National Mesothelioma Panel (NMP). When pathological material was not available or insufficient for a confirmed diagnosis by the NMP (N=62), a final diagnosis was reached by three independent pulmonologists of the Mesothelioma Group of the Dutch Thoracic Society (Baas et al, 2006).
Survival (outcome)
Survival was measured from the date of clinical diagnosis till death or censoring. The date of diagnosis was defined as the date on which malignant mesothelioma was diagnosed by the local hospital.
Prognostic variables
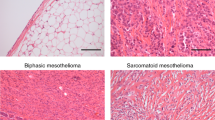
The following prognostic variables were studied: gender, age at diagnosis, year of diagnosis, pathologic morphologic subtype (epithelial, sarcomatoid and biphasic type), tumour location (pleural, peritoneal or other), and various variables associated with asbestos exposure, that is, duration of asbestos exposure, latency time (defined as the time elapsed between first asbestos exposure and diagnosis) and direct exposure (yes, no).
Analysis
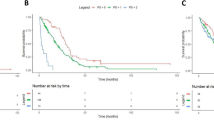
For the first aim, assessing overall survival, Kaplan–Meier analyses were used and survival curves were plotted. To put results into perspective, survival probabilities of our cohort were compared with the overall survival in the general Dutch population after adjustment for gender and age.
For the second aim, associations between possible prognostic variables and survival were estimated using Cox proportional hazards regression. Missing values were imputed with multiple imputation, conforming with current guidelines, since missing values occurred on various predictor variables (see Supplementary Appendix 1) (Donders et al, 2006). Bootstrapping was used to correct for overfitting (Harrell, 2001; Royston et al, 2009).
Finally, for our third aim, we estimated the predictive accuracy of all prognostic variables combined using both discrimination and calibration statistics. The discrimination was tested by Harrell’s c-statistic for censored data, and corrected for overfitting (Harrell, 2001). The calibration was performed based on survival after 1 year. Predicted 1-year survival probabilities were calculated according to different prognostic factors.
All analyses were performed with SAS enterprise guide 4.3 (SAS Institute Inc., Cary, NC, USA) and R version 2.10.1 (The R Foundation for Statistical Computing, Vienna, Austria).
Results
Patients
The baseline characteristics of the 1353 included patients are described in Table 1 (left column). In our cohort, the mean age at the time of diagnosis was 69 years and the majority of patients were male (91%). In almost all patients (96%) the tumour was located in the pleura. Epithelial morphology was the most frequent mesothelioma type (78%). In 78% of the patients, a history of direct exposure to asbestos was identified. About half of the patients had an asbestos exposure duration ⩾20 years. The latency time since first exposure ranged from 19 to 78 years with a median of 49 years.
Overall survival
Figure 1 shows the overall survival curve from the time of clinical diagnosis. Median survival was 333 days (95% CI: 309–368); 47% of the patients survived longer than 1 year and 20% more than 2 years. Less than 15% of the patients were alive 3 years after diagnosis in contrast to 90% of individuals with similar age and gender distribution in the general Dutch population.
Kaplan–Meier survival curve showing the overall survival and 95% CI from the time of the diagnosis of mesothelioma for (1) the entire study cohort and (2) of the general Dutch population. The 95% CI is presented by the broken line. The Dutch population was adjusted (i.e., standardised) to the age and gender distribution of the study cohort. The number of study patients at risk is indicated at the bottom of the plot (above the x axis).
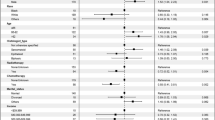
Prognostic factors and predictive accuracy
In a univariable analysis, all variables, except direct exposure, were significantly associated with survival at a significance level of 0.05 (Table 1, middle column). In the multivariable model, only age, morphology and localisation of malignant mesothelioma had a significant independent association with survival (Table 1, last column). Hence, worse survival was independently associated with older age, sarcomatoid subtype, or non-pleural localisation.
Table 2 shows the predicted 1-year survival probabilities stratified by tumour location, pathologic subtype and age based on our multivariable model. The 1-year survival given a diagnosis of pleural malignant mesothelioma of epithelial subtype was estimated to be 77% for a patient of 50 years and 38% for a patient of 80 years. Conversely, the 1-year survival given a diagnosis of pleural malignant mesothelioma of sarcomatoid subtype was estimated to be 53% for a patient of 50 years and 9% for a patient of 80 years. These estimated survival probabilities are much lower than those in the general Dutch population, where a man aged 50 or aged 80 has a 1-year survival probability of 99.7% and 92.5%, respectively. The multivariable model showed a c-statistic of 0.66 (95% CI: 0.64–0.68) and very good calibration (Hosmer–Lemeshow χ2=7.63, P-value=0.57).
Discussion
To date, the survival of malignant mesothelioma patients remains poor. After 1 year, only 47% of the patients were still alive. Predictors strongly associated with survival were patient age, mesothelioma localisation and subtype. These results are consistent with other population-based studies (Chapman et al, 2008; Mirabelli et al, 2009; Montanaro et al, 2009; Milano and Zhang, 2010). This study showed that the discriminative ability of these general predictors was moderate and the calibration was good.
Our observed survival was only marginally higher than in two older Dutch studies, in which survival among patients diagnosed with malignant mesothelioma between 1970–1994 and 1987–1989 was studied (van Gelder et al, 1994; Janssen-Heijnen et al, 1999). In these studies the probability of 1-year survival was about 42%, suggesting that survival has not improved substantially over the years. Lack of improvement was also observed by a recent Italian and American study (Montanaro et al, 2009; Milano and Zhang, 2010). However, if the mix of patients has changed over the years due to, for example, improved diagnosis in patients with suspected mesothelioma, then direct comparisons between older studies and our study are hard to make. Moreover, in the Dutch study of van Gelder et al (1994), in which patients diagnosed between 1987 and 1989 were studied, 42% of the patients were 65 years or younger, whereas in our study only 30% of the patients were younger than 65 years (data not shown).
The higher age in our cohort likely relates to currently longer latency times between asbestos exposure and diagnosis. Our results showed an average latency time of 49 years between initial asbestos exposure and diagnosis.
The prognostic value of patient age, malignant mesothelioma subtype and localisation can assist in the selection of patients more likely to benefit from intensive treatment modalities, especially for patient selection in future therapeutic randomised trials. However, in the current study not all potentially relevant predictors were available that might contribute to the discrimination of survival among malignant mesothelioma patients. For example, there is some evidence that patients’ general well-being and weight loss are important prognostic factors in patients with malignant mesothelioma (Edwards et al, 2000; Ak et al, 2009; Nowak et al, 2010). Therefore, we expect that predictive accuracy might improve, when these predictors would also be taken into account. We did not observe a significant association between characteristics of asbestos exposure and survival. However, in our data set asbestos exposure was mainly based on self-reporting, which could mean that exposure estimates are of lower quality than the other predictors considered.
Recently, more treatment options have become available for patients with malignant mesothelioma. Although these may benefit selected patients, their results are still far from satisfactory for the majority of the patients (Mott, 2012). In our study, patients received treatment according to latest insights, suggesting that, in general, the impact of treatment is still limited.
To improve the effect of treatment, an early diagnosis of malignant mesothelioma is of great value. This may hold in particular for patients with peritoneal mesothelioma, as the observed difference in survival between peritoneal mesothelioma and pleural mesothelioma may be explained by a delayed diagnosis of peritoneal mesothelioma due to the complexity of the disease (Manzini et al, 2010).
In conclusion, we showed that overall survival in patients with malignant mesothelioma remains poor and depends highly on patient age, malignant mesothelioma subtype and localisation. Additionally, we found that half of the patients are 70 years or older and a substantial part of the patients has a long latency time since asbestos exposure. A trend towards longer latency times may have profound implications for future lawsuits and reimbursements as in several countries financial compensation depends (partially) on latency times (Baas et al, 2006). Furthermore, the future prevalence of mesothelioma might still remain high as a result of these long latency times.
Change history
23 January 2013
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Ak G, Metintas S, Metintas M, Yildirim H, Erginel S, Kurt E, Alatas F, Cadirci O (2009) Prognostic factors according to the treatment schedule in malignant pleural mesothelioma. J Thorac Oncol 4: 1425–1430
Baas P, van ‘t Hullenaar N, Wagenaar J, Kaajan JP, Koolen M, Schrijver M, Schlosser N, Burgers JA (2006) Occupational asbestos exposure: how to deal with suspected mesothelioma cases – the Dutch approach. Ann Oncol 17: 848–852
Burgers JA, Damhuis RA (2004) Prognostic factors in malignant mesothelioma. Lung Cancer 45 (Suppl 1): S49–S54
Chapman A, Mulrennan S, Ladd B, Muers MF (2008) Population based epidemiology and prognosis of mesothelioma in Leeds, UK. Thorax 63: 435–439
Christensen BC, Godleski JJ, Roelofs CR, Longacker JL, Bueno R, Sugarbaker DJ, Marsit CJ, Nelson HH, Kelsey KT (2008) Asbestos burden predicts survival in pleural mesothelioma. Environ Health Perspect 116: 723–726
Donders AR, van der Heijden GJ, Stijnen T, Moons KG (2006) Review: a gentle introduction to imputation of missing values. J Clin Epidemiol 59: 1087–1091
Edwards JG, Abrams KR, Leverment JN, Spyt TJ, Waller DA, O’Byrne KJ (2000) Prognostic factors for malignant mesothelioma in 142 patients: validation of CALGB and EORTC prognostic scoring systems. Thorax 55: 731–735
Harrell FE (2001) Regression Modeling Strategies: with Applications to Linear Models, Logistic Regression, and Survival Analysis. Springer-Verlag: New York
Janssen-Heijnen ML, Damhuis RA, Klinkhamer PJ, Schipper RM, Coebergh JW (1999) Increased but low incidence and poor survival of malignant mesothelioma in the southeastern part of The Netherlands since 1970: a population-based study. Eur J Cancer Prev 8: 311–314
Manzini VP, Recchia L, Cafferata M, Porta C, Siena S, Giannetta L, Morelli F, Oniga F, Bearz A, Torri V, Cinquini M (2010) Malignant peritoneal mesothelioma: a multicenter study on 81 cases. Ann Oncol 21: 348–353
Milano MT, Zhang H (2010) Malignant pleural mesothelioma: a population-based study of survival. J Thorac Oncol 5: 1841–1848
Mirabelli D, Roberti S, Gangemi M, Rosato R, Ricceri F, Merler E, Gennaro V, Mangone L, Gorini G, Pascucci C, Cavone D, Nicita C, Barbieri PG, Marinaccio A, Magnani C, Montanaro F (2009) Survival of peritoneal malignant mesothelioma in Italy: a population-based study. Int J Cancer 124: 194–200
Montanaro F, Rosato R, Gangemi M, Roberti S, Ricceri F, Merler E, Gennaro V, Romanelli A, Chellini E, Pascucci C, Musti M, Nicita C, Barbieri PG, Marinaccio A, Magnani C, Mirabelli D (2009) Survival of pleural malignant mesothelioma in Italy: a population-based study. Int J Cancer 124: 201–207
Mott FE (2012) Mesothelioma: a review. Ochsner J 12: 70–79
Nowak AK, Francis RJ, Phillips MJ, Millward MJ, van der Schaaf AA, Boucek J, Musk AW, McCoy MJ, Segal A, Robins P, Byrne MJ (2010) A novel prognostic model for malignant mesothelioma incorporating quantitative FDG-PET imaging with clinical parameters. Clin Cancer Res 16: 2409–2417
Royston P, Moons KG, Altman DG, Vergouwe Y (2009) Prognosis and prognostic research: developing a prognostic model. BMJ 338: b604
Spirtas R, Connelly RR, Tucker MA (1988) Survival patterns for malignant mesothelioma: the SEER experience. Int J Cancer 41: 525–530
van Gelder T, Damhuis RA, Hoogsteden HC (1994) Prognostic factors and survival in malignant pleural mesothelioma. Eur Respir J 7: 1035–1038
Acknowledgements
This study was funded by the Institute for Asbestos Victims, The Netherlands.
Disclaimer
BAJMM is a board member of the Institute for Asbestos Victims. MJV is chairman of the Dutch National Mesothelioma Panel. JAB is chairman of the Mesothelioma Group of the Dutch Thoracic Society. Conclusions of this paper reflect the opinions of the authors and do not represent any determination or policy of the Institute for Asbestos Victims.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
BAJMM is a board member of the Institute for Asbestos Victims. MJV is chairman of the Dutch National Mesothelioma Panel. JAB is chairman of the Mesothelioma Group of the Dutch Thoracic Society. Conclusions of this paper reflect the opinions of the authors and do not represent any determination or policy of the Institute for Asbestos Victims.
Additional information
Supplementary Information accompanies the paper on British Journal of Cancer website
Supplementary information
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
van der Bij, S., Koffijberg, H., Burgers, J. et al. Prognosis and prognostic factors of patients with mesothelioma: a population-based study. Br J Cancer 107, 161–164 (2012). https://doi.org/10.1038/bjc.2012.245
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2012.245
Keywords
This article is cited by
-
Development of a prognostic nomogram for patients with malignant mesothelioma with bone metastasis
Scientific Reports (2023)
-
Genomic and transcriptomic analysis of a diffuse pleural mesothelioma patient-derived xenograft library
Genome Medicine (2022)
-
Integrated genomics point to immune vulnerabilities in pleural mesothelioma
Scientific Reports (2021)
-
Overexpression of fibulin-3 in tumor tissue predicts poor survival of malignant mesothelioma patients from hand-spinning asbestos exposed area in eastern China
Scientific Reports (2020)
-
A Nomogram to Predict Prognosis in Malignant Pleural Mesothelioma
World Journal of Surgery (2018)