Abstract
Background:
Biliary tract cancer (BTC) and benign biliary strictures can be difficult to differentiate using standard tumour markers such as serum carbohydrate antigen 19-9 (CA19-9) as they lack diagnostic accuracy.
Methods:
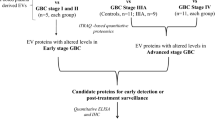
Two-dimensional difference gel electrophoresis and tandem mass spectrometry were used to profile immunodepleted serum samples collected from cases of BTC, primary sclerosing cholangitis (PSC), immunoglobulin G4-associated cholangitis and healthy volunteers. The serum levels of one candidate protein, leucine-rich α-2-glycoprotein (LRG1), were verified in individual samples using enzyme-linked immunosorbent assay and compared with serum levels of CA19-9, bilirubin, interleukin-6 (IL-6) and other inflammatory markers.
Results:
We report increased LRG1, CA19-9 and IL-6 levels in serum from patients with BTC compared with benign disease and healthy controls. Immunohistochemical analysis also demonstrated increased staining of LRG1 in BTC compared with cholangiocytes in benign biliary disease. The combination of receiver operating characteristic (ROC) curves for LRG1, CA19-9 and IL-6 demonstrated an area under the ROC curve of 0.98. In addition, raised LRG1 and CA19-9 were found to be independent predictors of BTC in the presence of elevated bilirubin, C-reactive protein and alkaline phosphatase.
Conclusion:
These results suggest LRG1, CA19-9 and IL-6 as useful markers for the diagnosis of BTC, particularly in high-risk patients with PSC.
Similar content being viewed by others
Main
Cholangiocarcinoma (CCA) and gallbladder carcinoma are often grouped together as biliary tract cancer (BTC) (de Groen et al, 1999). CCA is a rare but devastating disease that accounts for ∼15% of primary liver malignancies (Shaib and El-Serag, 2004). Although the incidence in Western nations has been estimated at 1 per 100 000, there are as yet unexplained increases in the age-adjusted incidence and mortality rates of intrahepatic CCA (Khan et al, 2002b; Shaib et al, 2004).
Disorders of the bile ducts associated with inflammation, stricturing and cholestasis, such as primary sclerosing cholangitis (PSC), have been identified as risk factors for BTC (Broome et al, 1995; Kornfeld et al, 1997; Bergquist et al, 2002; Burak et al, 2004; Claessen et al, 2009). Other inflammatory biliary diseases such as immunoglobulin G4-associated cholangitis (IAC) are also difficult to distinguish from BTC and PSC, occasionally leading to incorrect diagnosis and management. At present, surgical resection is the only curative treatment for BTC, with 5-year survival rates after R0 resection for hilar CCA of 11–41% and for distal extrahepatic CCA of 27–37% (Nakeeb et al, 1996; Neuhaus et al, 1999; Jarnagin et al, 2001; Nagorney and Kendrick, 2006; DeOliveira et al, 2007). Unresectable disease has an associated 5-year survival of less than 10% (Neuhaus et al, 1999; Reddy and Patel, 2006), and confirms the need for more accurate diagnostic biomarkers.
The gold standard for the diagnosis of BTC is cytological or histological confirmation of malignancy within the biliary stricture, either via endoscopic retrograde cholangiopancreatography (ERCP) or percutaneously (Khan et al, 2002a). However, this can be difficult to achieve due to the complex anatomical relationship between the liver hilum and bile ducts and the mode of tumour extension, which is often not mass forming. Approximately 15% of resections performed for suspected, pathologically unconfirmed, hilar BTC are due to benign strictures (Gerhards et al, 2001; Reddy and Patel, 2006).
Carbohydrate antigen 19-9 (CA19-9) is an established serum marker for the diagnosis of BTC, although it is reported to have a wide variation in sensitivity (50–90%) and specificity (54–98%), (Chalasani et al, 2000; Patel et al, 2000; Levy et al, 2005) and is often falsely elevated in benign biliary disease and/or cholangitis, with levels falling after relief of biliary obstruction and sepsis. Additionally, CA19-9 is virtually undetectable in the 7% of the population who are negative for the Lewis antigen (Steinberg, 1990). There is consequently a need to identify better circulating biomarkers for this disease. However, tumour marker proteins may be present at low concentrations in the circulation and masked by abundant blood proteins in proteomic analyses. Consequently, researchers have coupled immunoaffinity depletion with proteomic profiling to specifically remove abundant proteins and increase proteomic coverage (Liu et al, 2006; Qian et al, 2008).
This study analysed differential protein expression in four different pools of serum from patients with BTC, PSC, IAC and healthy volunteers. Using proteomic analysis the putative marker leucine-rich α-2-glycoprotein (LRG1) was shown to be upregulated in BTC, and was validated using a serum enzyme-linked immunosorbent assay (ELISA). The ability of LRG1 to differentiate BTC from benign biliary disease was evaluated and compared with the current standard tumour marker CA19-9, while taking into consideration potentially confounding conditions such as biliary obstruction and inflammation. Immunohistochemistry for LRG1 was performed on normal hepatobiliary tissue, benign biliary disease (PSC and primary biliary cirrhosis (PBC)) and BTC to evaluate differential staining characteristics. Serum interleukin-6 (IL-6) was also measured as it has been recently shown to be a key inflammatory cytokine involved in the carcinogenesis of CCA and may induce LRG1 (Hodge et al, 2005; Shirai et al, 2009).
Patients and methods
Patient population and clinical samples
The study was conducted following local ethical approval (06/Q0152/106) and written informed consent. Blood samples were prospectively collected from patients with BTC (n=37), PSC (n=11), IAC (n=7) and healthy volunteers (n=30) using Vacutainer tubes (BD, Franklin Lakes, NJ, USA). Primary sclerosing cholangitis was diagnosed on the basis of well-described clinical characteristics, primarily based on cholangiographic presence of biliary strictures and benign cytological biliary brushings, and where possible, supportive evidence such as the presence of inflammatory bowel disease or liver histology consistent with the diagnosis (Chapman et al, 1980). A diagnosis of IAC was based on the HISORt (HIstology, Serology and Imaging, Other organ involvement and Response to therapy) criteria (Chari, 2007). The clinical and pathological characteristics of the BTC patients who had stricturing ductal cancers rather than mass-forming tumours are presented in Table 1 and in Supplementary Information.
Baseline patient demographics and standard blood tests including liver biochemistry (bilirubin and alkaline phosphatase (ALP)), white cell count (WCC), neutrophil count, C-reactive protein (CRP), IgG4 and CA19-9 (electro-chemiluminescence immunoassay; Roche Modular, Indianapolis, IN, USA) were recorded at the time blood was taken (see Table 2). Blood samples for biochemical analysis were sent to the hospital laboratory for immediate processing, whereas for proteomic analysis, samples were allowed to clot at room temperature for 1 h, and then separated by centrifugation at 2200 r.p.m. for 10 min at 4 °C. Serum was decanted, aliquoted and stored at −80 °C. For proteomic analysis, all samples were thawed and an equal volume of each was pooled into one of four groups; BTC, PSC, IAC and healthy volunteers. The individual pools were vortexed to ensure thorough mixing, then aliquoted into cryovials and stored at −80 °C.
FPLC immunoaffinity depletion using tandem IgY14-Supermix system
IgY14 (12.7 × 39.5 mm, Affinity Column, Seppro (GenWay Biotech, San Diego, CA, USA), 28-288-12014-LC5) and SuperMix (6.4 × 31.5 mm, Affinity Column, Seppro GenWay Biotech, 28-288-23078-LC1) columns were used in series on a cooled AKTA FPLC system (GE Healthcare, Piscataway, NJ, USA) to deplete the serum pools of abundant proteins following the manufacturer's recommendations, and were similar to those described previously (Qian et al, 2008) (described in Supplementary Information).
Sample desalting, concentration and preparation
The protein-depleted serum was concentrated using 4-ml 5 kDa molecular weight cutoff Vivaspin centrifugal concentrators (Sartorius, Goettingen, Germany) at 3200 g and 10 °C, the buffer was exchanged with distilled water and further concentrated before drying down in a SpeedVac (Thermo Scientific, Waltham, MA, USA). Samples were resuspended in 100 μl of 2D lysis buffer (8 M urea, 2 M thiourea, 4% CHAPS, 0.5% IGEPAL, 10 mM Tris, pH 8.3) and protein concentrations determined using the Coomassie Plus protein assay (Pierce, Rockford, IL, USA). To evaluate the effectiveness of the immuno-depletion, samples were analysed by 1D-SDS-PAGE on NuPAGE Novex 4–12% Bis-Tris 1.5 mm × 10 well pre-cast gels (Invitrogen, Carlsbad, CA, USA) and stained with InstantBlue (Expedeon, Cambridge, UK).
Two-dimensional difference gel electrophoresis
For protein labelling, the N-hyroxysuccinimidyl ester cyanine dyes NHS-Cy3 and NHS-Cy5 were synthesised ‘in-house’ as previously described (Chan et al, 2005). Protein labelling and two-dimensional difference gel electrophoresis (2D-DIGE) were performed according to (Gharbi et al, 2002) and is described more detail in Supplementary Information. Briefly, 100 μg each of triplicate immuno-depleted protein pools were labelled with NHS-Cy3 or NHS-Cy5. Equal amounts of protein from all fractions were also pooled together and labelled with NHS-Cy2 (GE Healthcare, Piscataway, NJ, USA) as an internal standard run on all gels against the pairs of Cy3- and Cy5-labelled samples to aid in spot matching and for improved quantitative accuracy. Proteins were separated in the first dimension using isoelectric focusing, with 24 cm, non-linear pH 3-10 IPG strips (GE Healthcare), and in the second dimension on 1.5 mm 12% SDS-PAGE bonded gels. Following scanning and analysis using DeCyder software V5.0 (GE Healthcare), protein spots displaying a ⩾1.5 average-fold change in abundance between clinical conditions with P-values <0.05 were selected for picking on an Ettan automated spot picker (GE Healthcare).
Protein identification by LC-MS/MS
Protein spots were subjected to trypsin digestion and peptide extraction according to a previous protocol (Chan et al, 2005). Liquid chromatography-tandem mass spectrometry (LC-MS/MS) was performed using an Ultimate 3000 nanoflow liquid chromatography system (Dionex, Sunnyvale, CA, USA) coupled via a Picoview nanospray source (New Objective, Inc., Woburn, MA, USA) to an LTQ Orbitrap XL mass spectrometer (Thermo Scientific, Waltham, MA, USA) as previously described (Sinclair et al, 2011). For peptide identification, raw data files produced in Xcaliber software (Thermo Scientific) were transferred to Mascot Daemon for processing by Mascot Distiller V2.2.02, where peak detection was carried out for searching against the IPI human database (v3.53, 73 748 entries) (described in detail in Supplementary Information). Literature searches were carried out to determine previous associations between the identified proteins and cancer, and more specifically BTC. On the basis of this, LRG1 was chosen for further confirmation of differential expression.
LRG1 and IL-6 ELISA
The levels of LRG1 in undepleted serum samples from a subset of individual BTC patients (n=31), PSC/IAC patients (n=11/2) and healthy volunteers (n=15) were evaluated using a commercially available quantitative human LRG1 ELISA Assay Kit (Immuno-Biological Laboratories Co Ltd, Takasaki, Gunma, Japan). The assay gave a CV of 5.5% when tested on replicate samples used in this study. Serum IL-6 levels were evaluated using a commercially available quantitative human IL-6 ELISA Assay Kit (Pierce) in a subset of BTC patients (n=24), PSC/IAC patients (n=10/2) and healthy volunteers (n=6) and gave a CV of 6.7%.
LRG1 immunohistochemistry
Immunohistochemistry for LRG1 was performed on formalin-fixed paraffin-embedded tissues from one normal liver, one gallbladder with mild chronic cholecystitis, two liver biopsies showing PSC and PBC, and two CCA specimens using a commercially available affinity-purified rabbit polyclonal antibody, at a dilution of 1 : 1000 (13224-1-AP, ProteinTech, Chicago, IL, USA) (described in detail in Supplementary Information).
Statistical analysis
Statistical analyses were carried out using the GraphPad Prism V5 (La Jolla, CA, USA) and SPSS v10 (Chicago, IL, USA) software packages. All sample size calculations were performed using an α of 0.05 and β of 0.80 in MedCalc v11.4.2 (Mariakerke, Belgium). Continuous data between clinical groups were compared using the Mann–Whitney U-test for non-parametric data, and the Student's t-test for normally distributed data. Spearman's rank correlation was used to examine associations between two continuous variables. Associations between categorical variables were examined using Fisher's exact test. Multiple logistic regression analysis was used to examine the inter-relationships between serum proteins, biliary obstruction, patient age and cancer likelihood. As the CA19-9, bilirubin, CRP and ALP data were skewed, logarithmic transformation was applied before carrying out regression analyses. Normal cutoffs were defined for LRG1 (57.5 μg ml−1) and IL-6 (48.4 pg ml−1) as the optimum point at which sensitivity and specificity was maximised, whereas a cutoff of 37 U ml−1 for CA19-9 was recommended by the manufacturer. The sensitivity, specificity, positive and negative predictive values and accuracy were calculated for all three markers. Receiver operating characteristic (ROC) curves were generated and the area under the ROC curves (area under the curve (AUC)) defined. The combined AUC for a panel of biomarkers was calculated to define the diagnostic accuracy of discriminating benign from malignant biliary strictures. A P-value of <0.05 was considered significant.
Results
Identification of differentially expressed serum proteins in immuno-depleted fractions using 2D-DIGE/MS
Immunodepletion using FPLC over three or four runs for each of the four clinical pools were consistent, as were protein yields over all runs (Supplementary Information, Supplementary Figures S1 and S2). The depleted flow-through fractions contained four peaks, which were collected separately and protein contents compared with crude serum and eluates from the two columns (obtained by acid stripping) by 1D-SDS-PAGE with colloidal Coomassie Blue staining (Figures 1A and B). Protein bands were observed in the flow-through peak lanes that were not detected in both crude serum and column eluates, demonstrating the depletion of abundant proteins.
(A) Liquid chromatogram of flow-through fractions following immunoaffinity binding of high- and medium-abundance serum proteins. Protein peaks 1 to 4 were separately collected for analysis. (B) 1D-SDS PAGE and protein staining of flow-through peaks 3 and 4 obtained by FPLC immunoaffinity serum depletion confirming efficient depletion of high-abundance proteins. Diluted crude serum (1 : 100) and eluates from both IgY14 and SuperMix columns were run on the gel for comparison. A volume of 4.3 μg protein was loaded per lane. (C) Master gel image from 2D-DIGE experiment. The Cy2-labelled internal standard is shown. Highlighted spots were consistently differentially expressed between two or more of the clinical groups.
Immuno-depleted fractions were analysed by 2D-DIGE in triplicate to identify proteins whose expression differed significantly between sample groups. Image analysis revealed ∼1500 protein spots with protein abundance differences of >1.5-fold (P<0.05) considered as proteins of interest (Figure 1C). A total of 56 protein spots were altered between BTC and healthy volunteers, 47 between BTC and PSC and 31 spots between PSC and IAC. Spots of interest were excised from SyproRuby (Molecular Probes, Inc., Eugene, OR, USA) post-stained DIGE gels and subjected to LC-MS/MS-based analysis and database searching for identification. A total of 133 high-confidence protein identifications were made with many of the spots containing multiple proteins, as expected (Supplementary Information, Supplementary Table S1). Several proteins with a potential role in carcinogenesis were identified, including LRG1 and tetranectin/CLEC3B (Table 3). Isoforms of LRG1 were found in seven separate gel spots, all significantly upregulated in BTC vs healthy, PSC and IAC pools. One form found as a single identification in one gel spot was upregulated 4.49-fold in the BTC vs healthy pools, 3.57-fold in BTC vs PSC and 2.95-fold in BTC vs IAC. The altered expression of LRG1 was thus further examined in individual serum samples using a commercial ELISA.
Confirmation of differential expression of LRG1
To validate the 2D-DIGE result for LRG1 expression, an ELISA was run using serum from a subset of 59 individual patients that were used for the original pools. Figure 2A demonstrates that LRG1 levels were significantly elevated in the BTC group (median 67.4 μg ml−1, inter-quartile range (IQR) 58.6–83.4 μg ml−1) when compared with either the benign (PSC/IAC) (median 41.8 μg ml−1, IQR 32.9–53.4 μg ml−1; P=0.0001) or healthy volunteer groups (median 25.0 μg ml−1, IQR 18.7–30.4 μg ml−1; P<0.0001). Unlike the values for CA19-9 and serum bilirubin, LRG1 values were centrally distributed with skewness <0.5 (Figures 2A and B). The serum levels of LRG1 in individual patients belonging to the three clinical groups were thus in concordance with the 2D-DIGE analysis of pooled groups of samples.
Scatter plots of serum levels of (A) LRG1, (B) CA19-9, (C) CRP in samples from BTC patients (n=31), PSC/IAC patients (n=11/2) and healthy volunteers (n=15) used in the LRG1 validation experiment. (D) Scatter plot of serum IL-6 levels in a subgroup of BTC patients (n=24), benign biliary disease (PSC n=10, IAC n=2) and healthy volunteers (n=6) showing significant differences between groups. P-values (Mann–Whitney U-test) are shown.
Association between LRG1, CA19-9, biliary obstruction, raised inflammatory markers and likelihood of BTC
The BTC group had significant elevations of median CA19-9 (P=0.0005), bilirubin (P=0.04), CRP (P=0.006), ALP (P=0.0002) and neutrophil count (P=0.02) compared with the benign group, but not for WCC (Table 4, Figure 2 and data not shown). Serum bilirubin was elevated (>21 μmol l−1) in 24/31 BTC patients and 4/13 PSC/IAC patients. Serum LRG1 was positively correlated with bilirubin (Spearman's ρ=0.303, P=0.045) and ALP levels (ρ=0.670, P<0.0001). A significant correlation was also observed between LRG1 and CRP (ρ=0.687, P<0.0001), neutrophil count (ρ=0.541, P<0.0001) and WCC (ρ=0.455, P=0.002). Logistic regression analysis was undertaken to assess the independence of the association between LRG1 and likelihood of BTC from the effects of obstructive jaundice and inflammation. Given the skewed distribution of CA19-9, bilirubin, ALP and CRP, levels were normalised for subsequent regression analyses by logarithmic transformation. When LRG1, log10CA19-9, log10CRP, log10ALP and log10bilirubin were included on a univariate logistic regression model, all factors except log10bilirubin were independently associated with BTC. On multivariate analysis, only increased levels of LRG1 (odds ratio (OR)=1.09 (95% CI: 1.02–1.17); P=0.017) and CA19-9 (OR=4.24 (95% CI: 1.19–15.10); P=0.026) continued to exhibit an independent association with BTC likelihood. Patient age was a confounding factor for LRG1, with increasing age being significantly correlated with higher levels of LRG1 (ρ=0.345, P=0.022). Given the reported involvement of the inflammatory cytokine IL-6 in the carcinogenesis of CCA and its ability to induce LRG1, serum IL-6 levels were also measured in a subset of the samples. Median IL-6 levels were 62.1 pg ml−1 (IQR, 57.5–84.6 pg ml−1) for the BTC group, 17.1 pg ml−1 (IQR, 14.6–36.8 pg ml−1) for the benign group and <0.2 pg ml−1 for the healthy controls. Thus, IL-6 levels were significantly higher in BTC vs both the benign and healthy volunteer groups (P<0.0001) (Figure 2F). LRG1 was also positively correlated with serum IL-6 level (Spearman, ρ=0.631, P<0.001).
ROC curve analysis and diagnostic performance
The ROC curve AUC for LRG1 and CA19-9 were 0.87 (95% CI: 0.77–0.98) and 0.84 (95% CI: 0.69–0.98), respectively, whereas their combination was 0.92 (P<0.001) (Figure 3A). The AUC for serum IL-6 was 0.93 (95% CI 0.82–1.0). The AUC for the combination of LRG1 and IL-6 ROC curves was 0.97 (P=0.03). Finally, the combination of ROC curves for LRG1, CA19-9 and IL-6 gave an AUC of 0.98 (P=0.01) (Figure 3B). The sensitivity, specificity, positive predictive value, negative predictive value and accuracy for LRG1 (cutoff >57.5 μg ml−1) in distinguishing malignant from benign biliary strictures were 83, 92, 95, 73 and 86%, respectively. The corresponding figures for CA19-9 (cutoff >37 U ml−1) and IL-6 (cutoff >48.4 pg ml−1) were 83, 67, 83, 67 and 78%; and 92, 92, 96, 85 and 92%, respectively.
LRG1 immunohistochemistry
The pattern of LRG1 protein expression was assessed by immunohistochemistry in morphologically normal, benign and malignant hepatobiliary resection tissue. In normal liver, bile ducts did not stain for LRG1, whereas hepatocytes showed weak to moderate staining (Figure 4A). Biliary epithelium from a gallbladder showing chronic cholecystitis demonstrated negative staining for LRG1 (Figure 4B). In the PSC (Figure 4C) and PBC (Figure 4D) liver biopsies the biliary epithelium was negative for LRG1, but there was positive staining of hepatocytes, which was most marked in the periportal zones and greater than that seen in normal livers. Two CCAs (Figures 4E and F) showed positive staining for LRG1, both in the malignant cells and non-neoplastic hepatocytes in the liver adjacent to the carcinomas, most marked in the periportal zones.
LRG1 immunohistochemistry analysis demonstrating: (A) moderate expression of LRG1 in normal liver (arrowheads) with no expression in biliary epithelium (arrow) (original magnification × 400), (B) no expression of LRG1 in normal biliary epithelium from gallbladder (original magnification × 400), (C) PSC showing positive staining of hepatocytes with no staining of the biliary epithelium (arrow) (original magnification × 400), (D) PBC showing positive staining of hepatocytes with no staining of the biliary epithelium (arrow) (original magnification × 400), (E). cholangiocarcinoma showing positive expression in malignant cells (arrow) and in (arrow) adjacent non-neoplastic hepatocytes of the liver (arrowheads) (original magnification × 200), (F) cholangiocarcinoma showing positive expression of LRG (original magnification × 400).
Discussion
Recent applications of proteomic technologies have identified putative serum markers in a variety of gastrointestinal malignancies (Lin et al, 2009). However, relatively few proteomic studies of BTC using cell lines, bile or tissue have been performed, and only two have investigated circulating markers (Scarlett et al, 2006; Wang et al, 2009). In this rare cancer (Shaib and El-Serag, 2004), our discovery analysis of pooled serum samples using immunoaffinity depletion, 2D-DIGE and LC-MS/MS was able to detect differential protein expression between the BTC, benign and healthy groups, including upregulation of the putative marker LRG1. This upregulation was further verified in individual samples using an ELISA, which confirmed significant elevation of serum LRG1 in BTC compared with benign biliary disease (PSC and IAC) and healthy volunteers.
In hepatobiliary cancer, an ideal tumour marker should distinguish malignant from benign disease in the context of confounding factors such as obstructive jaundice and inflammation. In clinical practice, bile duct stenoses in BTC can be difficult to differentiate from those secondary to PSC and IAC (Chapman, 1999), as patients may share similar clinical, biochemical and radiological characteristics. Diagnosing CCA in patients with underlying PSC-related strictures using ERCP-guided biliary brush cytology or endoscopic ultrasound-guided fine needle aspiration can be challenging as sensitivity and specificity for brush cytology is inconsistent, and mass lesions are uncommon in early CCA. The positive predictive value of ultrasound, computed tomography and magnetic resonance imaging in identifying cancer in these PSC patients is also limited (Charatcharoenwitthaya et al, 2008). Recent studies of PSC have reported a 7–9% 10-year cumulative incidence of developing BTC (Burak et al, 2004; Claessen et al, 2009), and a lifetime risk of 20% (Bergquist et al, 2002; Burak et al, 2004). However, this may be an underestimation of the true prevalence, because the occurrence of CCA in autopsies or explanted livers of PSC patients undergoing transplantation maybe as high as 30% (Broome et al, 1996; Chalasani et al, 2000). These factors underline the need for effective markers of BTC in these high-risk groups.
Biliary obstruction and cholestatic liver enzymes can confound the significance of protein biomarkers in the context of pancreaticobiliary cancer (Yan et al, 2009). Here, by multivariate logistic regression, LRG1 was shown to be an independent predictor of BTC in the presence of elevated bilirubin, ALP and CRP. Carbohydrate antigen 19-9 was also an independent predictor of cancer. An LRG1 level of 57.5 μg ml−1 had a positive predictive value of 95% in discriminating BTC from benign biliary strictures, highlighting its potential use as a screening tool in PSC patients. The AUC for LRG1 was similar to that for CA19-9 (0.87 vs 0.84), whereas the combination of the two markers yielded a significantly higher (P<0.001) AUC of 0.92 compared with either marker alone. However, it should be emphasised that the sample size – particularly in the cohort with benign biliary strictures – was relatively small, so that these promising results will require validation in a larger sample set.
To minimise the likelihood of elevated acute-phase response proteins being due to infection, patients with symptoms or signs of ascending cholangitis were excluded from the study. Any elevation of CRP and IL-6 was thus interpreted to reflect inflammation secondary to benign or malignant biliary disease, rather than infection. The inflammatory cytokine IL-6 is increased in the biliary tract and systemic circulation in patients with CCA (Goydos et al, 1998; Sugawara et al, 1998; Tangkijvanich et al, 2004; Cheon et al, 2007), and has been proposed as a crucial cytokine involved in the pathogenesis of CCA (Okada et al, 1994; Park et al, 1999; Yokomuro et al, 2000; Wehbe et al, 2006; Yamagiwa et al, 2006; Isomoto et al, 2007). Recent work has also targeted IL-6 for the development of novel therapies for CCA (Braconi et al, 2011). Furthermore, the induction of LRG1 by IL-6 has been shown to be upregulated synergistically with mediators of inflammation such as TNFα in cell culture (Shirai et al, 2009). We thus assessed the utility of serum IL-6 levels in differentiating malignant from the benign inflammatory biliary diseases PSC and IAC. We showed a significant increase in serum IL-6 levels in BTC compared with benign biliary disease and healthy volunteers, and a positive correlation with LRG1 in BTC patients. A combination of the ROC curves for LRG1, IL-6 and CA19-9 yielded an AUC of 0.98 for the diagnosis of BTC vs PSC/IAC, supporting the concept that a combination of these markers may be an appropriate strategy for differential diagnosis in the clinic.
On immunohistochemical analysis, LRG1 expression was demonstrated in hepatocytes from normal livers with overexpression in hepatocytes, but not biliary epithelium, in the PSC and PBC benign cholestatic conditions. In CCA there was overexpression in malignant biliary epithelium in addition to increased hepatocyte staining, which may therefore account for the observed increase in LRG1 serum levels in BTC patients compared with PSC/IAC patients and healthy volunteers. Although the immunohistochemistry was performed on a small number of samples and is thus preliminary, the data suggest the potential of LRG1 staining to differentiate benign and malignant strictures in cytological brushings obtained at ERCP.
The physiological function of LRG1 is not known. LRG1 has been previously detected in the bile of a CCA patient using proteomic methods (Kristiansen et al, 2004), suggesting that it may be a glycoprotein which is synthesised in the liver and undergoes biliary excretion. Elevated plasma LRG1 has also been reported in patients with pancreatic cancers (Kakisaka et al, 2007), though its relationship to the presence or absence of biliary obstruction in these patients was not reported.
Given the rarity of BTC, PSC and IAC, only a limited number of patient samples were used in this study. However, assuming an AUC of 0.69 for CA19-9 and 0.85 for a useful biomarker panel in the diagnosis of BTC, only 22 patients in each of the malignant/benign groups would be required to detect a 0.16 AUC difference in diagnostic efficacy of the biomarker panel over CA19-9. Furthermore, the success of correctly diagnosing BTC vs benign PSC strictures using CA19-9 alone may be as low as 50% at a CA19-9 cutoff of 37 U ml−1 (Charatcharoenwitthaya et al, 2008). Based on our findings, further validation studies are warranted.
In conclusion, in this preliminary study of circulating biomarkers in patients with benign and malignant biliary strictures, a serum immunodepletion 2D-DIGE/MS strategy was used to identify LRG1 as a novel serum biomarker for detection of BTC. LRG1 had a discriminatory power similar to CA19-9 in differentiating benign from malignant biliary strictures, independent of biliary obstruction and inflammation. LRG1 is overexpressed in CCA cells compared with benign biliary epithelium. Serum IL-6 levels were significantly elevated in BTC compared with benign biliary disease, and a combination of LRG1, CA19-9 and IL-6 strongly discriminates BTC from benign biliary disease. This circulating serum biomarker panel may have important diagnostic implications for BTC, particularly in the context of high-risk groups such as patients with PSC.
Change history
29 March 2012
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Bergquist A, Ekbom A, Olsson R, Kornfeldt D, Loof L, Danielsson A, Hultcrantz R, Lindgren S, Prytz H, Sandberg-Gertzen H, Almer S, Granath F, Broome U (2002) Hepatic and extrahepatic malignancies in primary sclerosing cholangitis. J Hepatol 36: 321–327
Braconi C, Swenson E, Kogure T, Huang N, Patel T (2011) Targeting the IL-6 dependent phenotype can identify novel therapies for cholangiocarcinoma. PLoS One 5: e15195
Broome U, Lofberg R, Veress B, Eriksson LS (1995) Primary sclerosing cholangitis and ulcerative colitis: evidence for increased neoplastic potential. Hepatology 22: 1404–1408
Broome U, Olsson R, Loof L, Bodemar G, Hultcrantz R, Danielsson A, Prytz H, Sandberg-Gertzen H, Wallerstedt S, Lindberg G (1996) Natural history and prognostic factors in 305 Swedish patients with primary sclerosing cholangitis. Gut 38: 610–615
Burak K, Angulo P, Pasha TM, Egan K, Petz J, Lindor KD (2004) Incidence and risk factors for cholangiocarcinoma in primary sclerosing cholangitis. Am J Gastroenterol 99: 523–526
Chalasani N, Baluyut A, Ismail A, Zaman A, Sood G, Ghalib R, McCashland TM, Reddy KR, Zervos X, Anbari MA, Hoen H (2000) Cholangiocarcinoma in patients with primary sclerosing cholangitis: a multicenter case-control study. Hepatology 31: 7–11
Chan HL, Gharbi S, Gaffney PR, Cramer R, Waterfield MD, Timms JF (2005) Proteomic analysis of redox- and ErbB2-dependent changes in mammary luminal epithelial cells using cysteine- and lysine-labelling two-dimensional difference gel electrophoresis. Proteomics 5: 2908–2926
Chapman RW (1999) Risk factors for biliary tract carcinogenesis. Ann Oncol 10 (Suppl 4): 308–311
Chapman RW, Arborgh BA, Rhodes JM, Summerfield JA, Dick R, Scheuer PJ, Sherlock S (1980) Primary sclerosing cholangitis: a review of its clinical features, cholangiography, and hepatic histology. Gut 21: 870–877
Charatcharoenwitthaya P, Enders FB, Halling KC, Lindor KD (2008) Utility of serum tumor markers, imaging, and biliary cytology for detecting cholangiocarcinoma in primary sclerosing cholangitis. Hepatology (Baltimore, Md) 48: 1106–1117
Chari ST (2007) Diagnosis of autoimmune pancreatitis using its five cardinal features: introducing the Mayo Clinic′s HISORt criteria. J Gastroenterol 42 (Suppl 18): 39–41
Cheon YK, Cho YD, Moon JH, Jang JY, Kim YS, Lee MS, Lee JS, Shim CS (2007) Diagnostic utility of interleukin-6 (IL-6) for primary bile duct cancer and changes in serum IL-6 levels following photodynamic therapy. Am J Gastroenterol 102: 2164–2170
Claessen MM, Vleggaar FP, Tytgat KM, Siersema PD, van Buuren HR (2009) High lifetime risk of cancer in primary sclerosing cholangitis. J Hepatol 50: 158–164
de Groen PC, Gores GJ, LaRusso NF, Gunderson LL, Nagorney DM (1999) Biliary tract cancers. N Engl J Med 341: 1368–1378
DeOliveira ML, Cunningham SC, Cameron JL, Kamangar F, Winter JM, Lillemoe KD, Choti MA, Yeo CJ, Schulick RD (2007) Cholangiocarcinoma: thirty-one-year experience with 564 patients at a single institution. Ann Surg 245: 755–762
Gerhards MF, Vos P, van Gulik TM, Rauws EA, Bosma A, Gouma DJ (2001) Incidence of benign lesions in patients resected for suspicious hilar obstruction. Br J Surg 88: 48–51
Gharbi S, Gaffney P, Yang A, Zvelebil MJ, Cramer R, Waterfield MD, Timms JF (2002) Evaluation of two-dimensional differential gel electrophoresis for proteomic expression analysis of a model breast cancer cell system. Mol Cell Proteomics 1: 91–98
Goydos JS, Brumfield AM, Frezza E, Booth A, Lotze MT, Carty SE (1998) Marked elevation of serum interleukin-6 in patients with cholangiocarcinoma: validation of utility as a clinical marker. Ann Surg 227: 398–404
Hodge DR, Hurt EM, Farrar WL (2005) The role of IL-6 and STAT3 in inflammation and cancer. Eur J Cancer 41: 2502–2512
Isomoto H, Mott JL, Kobayashi S, Werneburg NW, Bronk SF, Haan S, Gores GJ (2007) Sustained IL-6/STAT-3 signaling in cholangiocarcinoma cells due to SOCS-3 epigenetic silencing. Gastroenterology 132: 384–396
Jarnagin WR, Fong Y, DeMatteo RP, Gonen M, Burke EC, Bodniewicz BJ, Youssef BM, Klimstra D, Blumgart LH (2001) Staging, resectability, and outcome in 225 patients with hilar cholangiocarcinoma. Ann Surg 234: 507–517; discussion 517–519
Kakisaka T, Kondo T, Okano T, Fujii K, Honda K, Endo M, Tsuchida A, Aoki T, Itoi T, Moriyasu F, Yamada T, Kato H, Nishimura T, Todo S, Hirohashi S (2007) Plasma proteomics of pancreatic cancer patients by multi-dimensional liquid chromatography and two-dimensional difference gel electrophoresis (2D-DIGE): up-regulation of leucine-rich alpha-2-glycoprotein in pancreatic cancer. J Chromatogr B Analyt Technol Biomed Life Sci 852: 257–267
Khan SA, Davidson BR, Goldin R, Pereira SP, Rosenberg WM, Taylor-Robinson SD, Thillainayagam AV, Thomas HC, Thursz MR, Wasan H (2002a) Guidelines for the diagnosis and treatment of cholangiocarcinoma: consensus document. Gut 51 (Suppl 6): VI1–VI9
Khan SA, Taylor-Robinson SD, Toledano MB, Beck A, Elliott P, Thomas HC (2002b) Changing international trends in mortality rates for liver, biliary and pancreatic tumours. J Hepatol 37: 806–813
Kornfeld D, Ekbom A, Ihre T (1997) Is there an excess risk for colorectal cancer in patients with ulcerative colitis and concomitant primary sclerosing cholangitis? A population based study. Gut 41: 522–525
Kristiansen TZ, Bunkenborg J, Gronborg M, Molina H, Thuluvath PJ, Argani P, Goggins MG, Maitra A, Pandey A (2004) A proteomic analysis of human bile. Mol Cell Proteomics 3: 715–728
Levy C, Lymp J, Angulo P, Gores GJ, Larusso N, Lindor KD (2005) The value of serum CA 19-9 in predicting cholangiocarcinomas in patients with primary sclerosing cholangitis. Dig Dis Sci 50: 1734–1740
Lin Y, Dynan WS, Lee JR, Zhu ZH, Schade RR (2009) The current state of proteomics in GI oncology. Dig Dis Sci 54: 431–457
Liu T, Qian WJ, Mottaz HM, Gritsenko MA, Norbeck AD, Moore RJ, Purvine SO, Camp II DG, Smith RD (2006) Evaluation of multiprotein immunoaffinity subtraction for plasma proteomics and candidate biomarker discovery using mass spectrometry. Mol Cell Proteomics 5: 2167–2174
Nagorney DM, Kendrick ML (2006) Hepatic resection in the treatment of hilar cholangiocarcinoma. Adv Surg 40: 159–171
Nakeeb A, Pitt HA, Sohn TA, Coleman J, Abrams RA, Piantadosi S, Hruban RH, Lillemoe KD, Yeo CJ, Cameron JL (1996) Cholangiocarcinoma. A spectrum of intrahepatic, perihilar, and distal tumors. Ann Surg 224: 463–473; discussion 473–5
Neuhaus P, Jonas S, Bechstein WO, Lohmann R, Radke C, Kling N, Wex C, Lobeck H, Hintze R (1999) Extended resections for hilar cholangiocarcinoma. Ann Surg 230: 808–818; discussion 819
Okada K, Shimizu Y, Nambu S, Higuchi K, Watanabe A (1994) Interleukin-6 functions as an autocrine growth factor in a cholangiocarcinoma cell line. J Gastroenterol Hepatol 9: 462–467
Park J, Tadlock L, Gores GJ, Patel T (1999) Inhibition of interleukin 6-mediated mitogen-activated protein kinase activation attenuates growth of a cholangiocarcinoma cell line. Hepatology 30: 1128–1133
Patel AH, Harnois DM, Klee GG, LaRusso NF, Gores GJ (2000) The utility of CA 19-9 in the diagnoses of cholangiocarcinoma in patients without primary sclerosing cholangitis. Am J Gastroenterol 95: 204–207
Qian WJ, Kaleta DT, Petritis BO, Jiang H, Liu T, Zhang X, Mottaz HM, Varnum SM, Camp II DG, Huang L, Fang X, Zhang WW, Smith RD (2008) Enhanced detection of low abundance human plasma proteins using a tandem IgY12-SuperMix immunoaffinity separation strategy. Mol Cell Proteomics 7: 1963–1973
Reddy SB, Patel T (2006) Current approaches to the diagnosis and treatment of cholangiocarcinoma. Curr Gastroenterol Rep 8: 30–37
Scarlett CJ, Saxby AJ, Nielsen A, Bell C, Samra JS, Hugh T, Baxter RC, Smith RC (2006) Proteomic profiling of cholangiocarcinoma: diagnostic potential of SELDI-TOF MS in malignant bile duct stricture. Hepatology 44: 658–666
Shaib Y, El-Serag HB (2004) The epidemiology of cholangiocarcinoma. Semin Liver Dis 24: 115–125
Shaib YH, Davila JA, McGlynn K, El-Serag HB (2004) Rising incidence of intrahepatic cholangiocarcinoma in the United States: a true increase? J Hepatol 40: 472–477
Shirai R, Hirano F, Ohkura N, Ikeda K, Inoue S (2009) Up-regulation of the expression of leucine-rich alpha(2)-glycoprotein in hepatocytes by the mediators of acute-phase response. Biochem Biophys Res Commun 382: 776–779
Sinclair J, Metodieva G, Dafou D, Gayther SA, Timms JF (2011) Profiling signatures of ovarian cancer tumour suppression using 2D-DIGE and 2D-LC-MS/MS with tandem mass tagging. J Proteomics 74: 451–465
Steinberg W (1990) The clinical utility of the CA 19-9 tumor-associated antigen. Am J Gastroenterol 85: 350–355
Sugawara H, Yasoshima M, Katayanagi K, Kono N, Watanabe Y, Harada K, Nakanuma Y (1998) Relationship between interleukin-6 and proliferation and differentiation in cholangiocarcinoma. Histopathology 33: 145–153
Tangkijvanich P, Thong-ngam D, Theamboonlers A, Hanvivatvong O, Kullavanijaya P, Poovorawan Y (2004) Diagnostic role of serum interleukin 6 and CA 19-9 in patients with cholangiocarcinoma. Hepato-Gastroenterology 51: 15–19
Wang X, Dai S, Zhang Z, Liu L, Wang J, Xiao X, He D, Liu B (2009) Characterization of apolipoprotein A-I as a potential biomarker for cholangiocarcinoma. Eur J Cancer Care (Engl) 18: 625–635
Wehbe H, Henson R, Meng F, Mize-Berge J, Patel T (2006) Interleukin-6 contributes to growth in cholangiocarcinoma cells by aberrant promoter methylation and gene expression. Cancer Res 66: 10517–10524
Yamagiwa Y, Meng F, Patel T (2006) Interleukin-6 decreases senescence and increases telomerase activity in malignant human cholangiocytes. Life Sci 78: 2494–2502
Yan L, Tonack S, Smith R, Dodd S, Jenkins RE, Kitteringham N, Greenhalf W, Ghaneh P, Neoptolemos JP, Costello E (2009) Confounding effect of obstructive jaundice in the interpretation of proteomic plasma profiling data for pancreatic cancer. J Proteome Res 8: 142–148
Yokomuro S, Tsuji H, Lunz III JG, Sakamoto T, Ezure T, Murase N, Demetris AJ (2000) Growth control of human biliary epithelial cells by interleukin 6, hepatocyte growth factor, transforming growth factor beta1, and activin A: comparison of a cholangiocarcinoma cell line with primary cultures of non-neoplastic biliary epithelial cells. Hepatology 32: 26–35
Acknowledgements
This work was supported by NIH grant P01CA8420 and the Bowel Cancer & Digestive Research Institute Australia, and was undertaken at UCLH/UCL, which received a proportion of funding from the Department of Health's NIHR Biomedical Research Centres funding scheme.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Supplementary Information accompanies the paper on British Journal of Cancer website
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Sandanayake, N., Sinclair, J., Andreola, F. et al. A combination of serum leucine-rich α-2-glycoprotein 1, CA19-9 and interleukin-6 differentiate biliary tract cancer from benign biliary strictures. Br J Cancer 105, 1370–1378 (2011). https://doi.org/10.1038/bjc.2011.376
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2011.376
Keywords
This article is cited by
-
Latrophilin-2 is a novel receptor of LRG1 that rescues vascular and neurological abnormalities and restores diabetic erectile function
Experimental & Molecular Medicine (2022)
-
Colorectal cancer-associated fibroblasts promote metastasis by up-regulating LRG1 through stromal IL-6/STAT3 signaling
Cell Death & Disease (2021)
-
Serum leucine-rich alpha-2-glycoprotein-1 with fucosylated triantennary N-glycan: a novel colorectal cancer marker
BMC Cancer (2018)
-
LRG1 modulates epithelial-mesenchymal transition and angiogenesis in colorectal cancer via HIF-1α activation
Journal of Experimental & Clinical Cancer Research (2016)
-
The role of TGFβ1 and LRG1 in cardiac remodelling and heart failure
Biophysical Reviews (2015)