Abstract
Second primary malignancies (SPMs) among multiple myeloma (MM) patients have been reported with an estimated incidence varying from 1 to 15%. We have previously reported that significant disparity exists in MM survival across patients of different ethnicities. We undertook a Surveillance Epidemiology and End Results-based analysis to describe the incidence of SPMs among MM patients of different ethnicities, to explore the variable impact that SPMs might have on MM outcomes of patients across racial subgroups. We found that the risk of developing SPMs among MM patients is variable depending on the patient’s ethnic background. This warrants further exploration of the impact of SPMs on outcomes of MM patients across different racial subgroups, especially in the form of prospective data collection and analyses.
Similar content being viewed by others
Introduction
Second primary malignancies (SPMs) among multiple myeloma (MM) patients have been reported with an estimated incidence that varies from 1 to 15%.1, 2, 3, 4, 5, 6 The incidence of cancer per year of life in the general population is calculated to be 1.7% in those aged 65–69 years, and it increases with advancing age.7 Cancer survivors have a 14% increased risk of developing another malignancy compared to the general population.8 With major advancements in the treatment of MM, there has been an increase in the overall survival. This has led to an increased life expectancy of those diagnosed with MM as a primary malignancy. This has, however, led to the renewed concern about long-term comorbidities including the risk of SPM in surviving MM patients. Recently, an increase in the incidence of SPM in MM patients treated with certain novel anti-myeloma treatments, particularly the immunomodulatory drugs, has been reported in large randomized clinical trials.9, 10, 11 Although the specific causative role of these agents is still not established, several factors including the duration and timing of treatment, the use of various combination regimens and certain patient-related factors such as age and tumor microenvironment have been postulated. We have previously reported a comprehensive analysis of SPM in MM patients utilizing the Surveillance Epidemiology and End Results (SEER) registry database.12 Furthermore, we also noted in a separate analysis that significant disparity exists in MM survival across patients of different ethnicities.13 Considering the rapidly changing US population demographics and the fact that the Hispanic and Asian populations are the two fastest growing racial subgroups in the US, we undertook a SEER-based analysis to describe the incidence of SPM among MM patients of different ethnicities.
Materials and methods
Patients
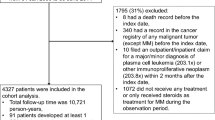
We utilized data from the National Cancer Institute’s SEER program’s original nine registries (Atlanta, Connecticut, Detroit, Hawaii, Iowa, New Mexico, San Francisco-Oakland, Seattle and Utah) with incidence data from over a 35-year interval (1973–2008). Our analysis was restricted to patients with MM as the first primary malignancy and with a microscopic confirmation of diagnosis. We excluded cases whose reporting sources were coded as autopsy or death-certificate-only, cases where MM was not the first primary cancer diagnosis and cases with SPM diagnosed within the first 2 months of MM diagnosis. Mutually exclusive race/ethnicity categories were: African Americans (AA), Asians/Pacific Islanders (API), Hispanic whites (HW), non-Hispanic whites (NHW) and others. The risk of SPM among MM patients was explored by ethnicity, type of SPM and latency period.
Statistical analysis
To estimate SPM risk, we defined a cohort of MM patients with no history of malignancy. Person-years for age strata (5-year age-groups), sex, race (AA, API, HW, NHW and others) and the year of diagnosis were calculated from 2 months after diagnosis of MM to the date of death, date of diagnosis of SPM, date of loss to follow-up, the end of study (31 December 2008) or whichever came first. General population incidence rates for each stratum were multiplied by their respective accumulated person-years-at-risk to estimate the overall expected cancer cases in that cohort of MM patients.
Observed-to-expected ratio (O/E) of SPM was calculated using incidence rates of cancers for the general population. The 95% confidence interval (CI) were constructed using Fisher’s exact test. We used likelihood ratio tests based on Poisson regression models that included SEER registry general population rates to evaluate linear trends and heterogeneity across different SPM sites. We included at least five observed occurrences in each stratum. We further performed multivariate Poisson regression analysis adjusted for age, sex and latency to compare the standardized incidence ratios across different year categories. All analyses were completed using SEER*Stat version 7.0.5 statistical software (Surveillance Research Program, National Cancer Institute, http://www.seer.cancer.gov/seerstat) and Stata version 11.2 (StataCorp LP, College Station, TX, USA).
Results
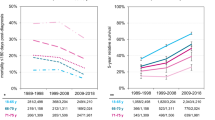
A total of 3090 cases of MM with SPM were diagnosed between 1973 and 2008, of which, 2021 patients met our inclusion criteria. Stratification of SPM by ethnicity revealed: 387 AA (19%), 72 API (4%), 51 HW (3%), 1500 NHW (74%) and 11 other (<1%) cases. There was an average 4.7 year latency period between diagnosis of MM and SPM (mean age 68.2 and 72.9 years, respectively). The latency period was not significantly different by type of SPM (solid organ versus hematological) or ethnicity. AA had the youngest age at diagnosis for both MM and SPM (65.6 and 70.1 years, respectively; Figure 1). Detailed results of the SPM in MM analysis other than that related to patient race/ethnicity have been previously reported.12 The overall risk of observed SPM was not different from expected rates by ethnicity, with the exception of HW who had a significantly decreased overall SPM risk (O/E 0.67; 95% CI 0.50–0.88; Figure 2). Table 1 summarizes the SPM sites that had a significant difference (marked by a) in observed and expected risks by race. HW were also less likely to develop all solid-organ SPM (0.66; 95% CI 0.48–0.89). Within solid-organ sites, HW had a significantly decreased O/E risk of developing lung/bronchus (O/E 0.34; 95% CI 0.08–0.88) and prostate SPM (O/E 0.48; 95% CI 0.19–0.99). NHW were the only ethnic subgroup with an increased O/E risk of developing melanoma of the skin (O/E 1.38; 95% CI 1.06–1.78) and non-Hodgkin lymphoma (O/E 1.28; 95% CI 1.01–1.61), while the O/E risk of developing SPM of the kidney/renal pelvis was increased only among AA (O/E 2.17; 95% CI 1.31–3.39). The O/E risk of acute non-lymphocytic leukemia as SPM was significantly increased among AA (O/E 6.24; 95% CI 3.41–10.47), API (O/E 6.32; 95% CI 1.72–16.19) and among NHW (O/E 6.85; 95% CI 5.55–8.38).
Discussion
Major advancements in the treatment options for MM have led to a significant increase in overall survival. This may have translated into an increase in the observed incidence of SPM in MM patients. Mailankody et al.14 demonstrated a twofold increase in risk of SPM in the Swedish population of MM patients compared to their age and sex-matched general population, irrespective of the year of diagnosis and the treatment received. They also duplicated the 11-fold increased risk of developing acute myeloid leukemia/myelodysplastic syndrome in MM patients as compared to the general population, as has been demonstrated in prior studies here in the United States.2,4,15,16 They further established an eight-fold increased risk of developing acute myeloid leukemia/myelodysplastic syndrome in patients with monoclonal gammopathy of undetermined significance (MGUS). Similarly a 2.4-fold increased risk of myelodysplastic syndrome in MGUS patients was reported by Roeker et al.17 at the Mayo clinic. However, they observed no increase in the incidence of acute myeloid leukemia in their screened population, which was comprised of individuals from Olmsted County in Minnesota, and is noticeably different from the Scandinavian population in the Swedish study.
Racial disparity has been proven in multiple studies to be an independent risk factor in the incidence of MGUS and MM.18, 19, 20, 21, 22, 23, 24, 25, 26, 27 Although, exploring SPMs in MGUS, MM and in patients who develop MM from previously reported MGUS would be very insightful, such an analysis is not feasible from the SEER database due to the lack of uniform reporting of MGUS in SEER as well as a much less than universal reporting of sequential diagnoses of MGUS and MM. Hence, we performed one of the largest population-based analyses for the risk of SPM developing in patients with an established diagnosis of MM, stratified by race/ethnicity. We found that the risk of developing SPM among MM patients is variable depending on the patient’s ethnic background. For all SPM sites analyzed together, there was no significant difference between the observed and expected incidence. However, O/E risk was significantly decreased for solid-organ SPM and increased for hematological malignancies, with the highest risk being for acute non-lymphocytic leukemia. This was consistent with the observation by Chakraborty et al.28 We also had similar findings in terms of the increased incidence of melanoma in NHW and kidney cancer in the AA population. Our analysis had two additional subgroups of HW and API, and revealed further differences among the incidence of SPM (Table 1).
Recently, Tzeng et al. reported several differences in the characteristics of SPM in the Asian population of Taiwan. They reported a 13-fold increased risk in the overall incidence of SPM, which increased 24-fold for myeloid leukemia.29 These incidence rates were significantly different than what was reported for our API population, but our API population was not strictly Asian and not regionally constrained. They were also quite different from the incidence established in the Swedish population study (twofold and 11-fold increase in overall SPM and myelodysplastic syndrome/acute myeloid leukemia, respectively).14 The latency period for occurrence of these SPMs was also shorter (1.9 years) compared to our API population (6.7 years) and the Western population (~4 years).14 Interestingly, Tzeng et al.29 and colleagues also demonstrated a decreased risk of developing SPM with increasing age in this Asian population. This has not been observed in any other patient population so far and likely highlights the importance of disparity not only in race but also possibly in environmental, behavioral and host genetic factors as proposed by others in studies of SPM after MM.30,31 These have looked at the effect of various treatment modalities and the molecular disease heterogeneity as possible explanations for the causality of SPM.
Palumbo et al.32 recently published results of meta-analyses of seven trials for the cumulative incidence of all SPM in newly diagnosed MM patients who had received lenalidomide therapy. They demonstrated an increased incidence of SPM in this patient population, but no subset data were presented for ethnic miscellany. Autologous stem cell transplant remains one of the primary modalities in the treatment of MM. The post-autologous stem cell transplant incidence of SPM was reportedly increased in a single German institution analysis of MM patients.33 Recently, Krishnan et al. also identified a possible causal association between autologous stem cell transplant and the development of SPM. Their study population included patients from a single institution with a relatively larger HW population mix, which maybe because it is based out of Los Angeles, California. Their patient population had an augmented exposure to sunlight, which had the authors also include non-melanoma skin cancers in their analysis. They identified race/ethnicity as an independent risk factor and reported an increase in the incidence of SPM (particularly non-melanoma skin cancers) only among NHW population, after adjustment for sex and year of autologous stem cell transplant.34 Our analysis also identifies that NHW have an increased incidence of both melanoma and non-melanoma skin cancers, but we did not have individual treatment data, and therefore no patient-level comparison can be made (Table 1).
Merrill et al.35 have reported an overall increased incidence of cancer in NHW as compared to HW, which was adjusted for sex. Our analysis revealed that among all ethnicities, HW had the lowest overall O/E ratio for development of SPM, both hematological and solid-organ type. They also had the lowest overall O/E incidence of prostate cancer. Socioeconomic status and access to healthcare has been ascertained as one of the primary reasons for different outcomes in prostate cancer among various racial groups. Tyson and Castle36 recently published that Hispanics with equal access to treatment for prostate cancer have similar overall survival compared to the white population. They also showed that the Asian population did better after adjustment for the receipt of treatment, while the AA population did worse. Socioeconomic status has been associated with survival in cancer patients.37,38 A patient’s address/postal code could be used as a surrogate for their socioeconomic status, but unfortunately this information is not included in the SEER database and hence precludes this analysis in our study. In our analyses, AA patients had a higher incidence of kidney/renal pelvis SPM compared to other ethnicities. Historically, the incidence of primary renal cell cancer has been higher among AA patients.39 Chow et al.40 verified that AA patients with renal cell cancer had a worse outcome in terms of survival compared to the white population, and this was irrespective of age, sex, tumor stage or size, histological subtype or surgical treatment. Most studies so far have evaluated the disparities among the two most prevalent races in the United States, NHW and AA. With the diversification of patient population in the United States and worldwide, it has become imperative to further define prognostic factors and treatment modalities on the basis of racial dissimilarity.
The strength of our study lies in the large number of population-based MM and SPM cases identified in the time period analyzed. We were also able to eliminate selection bias, which is generally introduced when data from hospital-based populations are utilized. The SEER ascertainment also helped expand the generalizability of the findings to patients who are not enrolled in clinical trials. MM is a relatively rare cancer and the survival time is shorter compared with other hematological malignancies, making SPM case ascertainment a challenge. Therefore, we chose to exclude cases diagnosed with a second cancer within the first 2 months of MM diagnosis. To address the issue of surveillance bias within the first year of a primary cancer diagnosis, we performed a sensitivity analysis excluding SPM cases diagnosed within the first year, and the results were similar.12 The SEER database does not provide us with individual-level treatment information; thus we were unable to test the effect/association of treatment modalities on the variance in incidence of SPM among the different ethnic groups.
Conclusion
Exploring potential causes of outcome disparities is important for evaluating disease characteristics and optimal triaging of healthcare resources for specific patient populations. The demonstration of an increased risk of developing specific SPMs in MM patients of certain ethnicity may be utilized in clinical practice to target the defined population for appropriate screening. We have performed the largest population-based analysis for the risk of SPM in MM patients stratified by race/ethnicity. We found that the risk of developing SPM among MM patients is variable depending on the patient’s ethnic background. This warrants further exploration of the impact of SPM on outcomes of MM patients across different racial subgroups, especially in the form of prospective data collection and analyses.
References
Law IP, Blom J . Second malignancies in patients with multiple myeloma. Oncology 1977; 34: 20–24.
Bergsagel DE, Bailey AJ, Langley GR, MacDonald RN, White DF, Miller AB . The chemotherapy of plasma-cell myeloma and the incidence of acute leukemia. N Engl J Med 1979; 301: 743–748.
Cuzick J, Erskine S, Edelman D, Galton DAG . A comparison of the incidence of the myelodysplastic syndrome and acute myeloid leukaemia following melphalan and cyclophosphamide treatment for myelomatosis. Br J Cancer 1987; 55: 523–529.
Govindarajan R, Jagannath S, Flick JT, Vesole DH, Sawyer J, Barlogie B et al. Preceding standard therapy is the likely cause of MDS after autotransplants for multiple myeloma. Br J Haematol 1996; 95: 349–353.
Olivanen T . Acute leukaemia and other secondary neoplasms in patients treated with conventional chemotherapy for multiple myeloma: a Finnish Leukaemia Group study. Eur J Haematol 2000; 65: 123–127.
Przepiorka D, Buadi F, McClune B, Franz G, Walsh W, White F . Myelodysplastic syndrome after autologous peripheral blood stem cell transplantation for multiple myeloma. Bone Marrow Transplant 2007; 40: 759–764.
Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF et al SEER Cancer Statistics Review, 1975-2011. National Cancer Institute: Bethesda, MD, USA. http://seer.cancer.gov/csr/1975_2011/, based on November 2013 SEER data submission posted to the SEER web site in April 2014.
Curtis RE, Freedman DM, Ron E, Ries LAG, Hacker DG, Edwards BK et al New Malignancies Among Cancer Survivors: SEER Cancer Registries, 1972-2000. National Cancer Institute: Bethesda, MD, 2006, NIH Publ. No. 05-5302.
Palumbo A, Hajek R, Delforge M, Kropff M, Petrucci MT, Catalano J et al. Continuous lenalidomide treatment for newly diagnosed multiple myeloma. N Engl J Med 2012; 366: 1759–1769.
Attal M, Lauwers-Cances V, Marit G, Caillot D, Moreau P, Facon T et al. Lenalidomide maintenance after stem-cell transplantation for multiple myeloma. N Engl J Med 2012; 366: 1782–1791.
McCarthy PL, Owzar K, Hofmeister CC, Hurd DD, Hassoun H, Richardson PG et al. Lenalidomide after stem-cell transplantation for multiple myeloma. N Engl J Med 2012; 366: 1770–1781.
Razavi P, Rand KA, Cozen W, Chanan-Khan A, Usmani S, Ailawadhi S . Patterns of second primary malignancy risk in multiple myeloma patients before and after the introduction of novel therapeutics. Blood Cancer J 2013; 3: e121.
Ailawadhi S, Aldoss IT, Yang D, Razavi P, Cozen W, Sher T et al. Outcome disparities in multiple myeloma: a SEER-based comparative analysis of ethnic subgroups. Br J Haematol 2012; 158: 91–98.
Mailankody S, Pfeiffer RM, Kristinsson SY, Korde N, Bjorkholm M, Goldin LR et al. Risk of acute myeloid leukemia and myelodysplastic syndromes after multiple myeloma and its precursor disease (MGUS). Blood 2011; 118: 4086–4092.
Kyle RA, Pierre RV, Bayrd ED . Multiple myeloma and acute myelomonocytic leukemia. N Engl J Med 1970; 283: 1121–1125.
Andersen E, Videbaek A . Stem cell leukaemia in myelomatosis. Scand J Haematol 1970; 7: 201–207.
Roeker LE, Larson DR, Kyle RA, Kumar S, Dispenzieri A, Rajkumar SV . Risk of acute leukemia and myelodysplastic syndromes in patients with monoclonal gammopathy of undetermined significance (MGUS): a population-based study of 17 315 patients. Leukemia 2013; 27: 1391–1393.
Benjamin M, Reddy S, Brawley OW . Myeloma and race: a review of the literature. Cancer Metastasis Rev 2003; 22: 87–93.
Iwanaga M, Tagawa M, Tsukasaki K, Kamihira S, Tomonaga M . Prevalence of monoclonal gammopathy of undetermined significance: study of 52,802 persons in Nagasaki City, Japan. Mayo Clin Proc 2007; 82: 1474–1479.
Gebregziabher M, Bernstein L, Wang Y, Cozen W . Risk patterns of multiple myeloma in Los Angeles County, 1972-1999 (United States). Cancer Causes Control 2006; 17: 931–938.
Besson C, Gonin C, Brebion A, Delaunay C, Panelatti G, Plumelle Y . Incidence of hematological malignancies in Martinique, French West Indies, overrepresentation of multiple myeloma and adult T cell leukemia/lymphoma. Leukemia 2001; 15: 828–831.
Munshi NC . Monoclonal gammopathy of undetermined significance: genetic vs environmental etiologies. Mayo Clin Proc 2007; 82: 1457–1459.
Waxman AJ, Mink PJ, Devesa SS, Anderson WF, Weiss BM, Kristinsson SY et al. Racial disparities in incidence and outcome in multiple myeloma: a population-based study. Blood 2010; 116: 5501–5506.
Cohen HJ, Crawford J, Rao MK, Pieper CF, Currie MS . Racial differences in the prevalence of monoclonal gammopathy in a community-based sample of the elderly. Am J Med 1998; 104: 439–444.
Albain KS, Unger JM, Crowley JJ, Coltman CA, Hershman DL . Racial disparities in cancer survival among randomized clinical trials patients of the southwest oncology group. J Natl Cancer Inst 2009; 101: 984–992.
Landgren O, Gridley G, Turesson I, Caporaso NE, Goldin LR, Baris D et al. Risk of monoclonal gammopathy of undetermined significance (MGUS) and subsequent multiple myeloma among African American and white veterans in the United States. Blood 2006; 107: 904–906.
Landgren O, Weiss BM . Patterns of monoclonal gammopathy of undetermined significance and multiple myeloma in various ethnic/racial groups: support for genetic factors in pathogenesis. Leukemia 2009; 23: 1691–1697.
Chakraborty S, Hauke RJ, Bonthu N, Tarantolo SR . Increased incidence of a second lymphoproliferative malignancy in patients with multiple myeloma—A SEER based study. Anticancer Res 2012; 32: 4507–4515.
Tzeng HE, Lin CL, Tsai CH, Tang CH, Hwang WL, Cheng YW et al. Time trend of multiple myeloma and associated secondary primary malignancies in Asian patients: a Taiwan population-based study. PLoS One 2013; 8: 7.
Thomas A, Mailankody S, Korde N, Kristinsson SY, Turesson I, Landgren O . Second malignancies after multiple myeloma: from 1960s to 2010s. Blood 2012; 119: 2731–2737.
Cannon MJ, Flanders WD, Pellett PE . Occurrence of primary cancers in association with multiple myeloma and Kaposi's sarcoma in the United States, 1973-1995. Int J Cancer 2000; 85: 453–456.
Palumbo A, Bringhen S, Kumar SK, Lupparelli G, Usmani S, Waage A et al. Second primary malignancies with lenalidomide therapy for newly diagnosed myeloma: a meta-analysis of individual patient data. Lancet Oncol 2014; 15: 333–342.
Fenk R, Neubauer F, Bruns I, Schröder T, Germing U, Haas R et al. Secondary primary malignancies in patients with multiple myeloma treated with high-dose chemotherapy and autologous blood stem cell transplantation. Br J Haematol 2012; 156: 683–686.
Krishnan AY, Mei M, Sun CL, Thomas SH, Teh JB, Kang T et al. Second primary malignancies after autologous hematopoietic cell transplantation for multiple myeloma. Biol Blood Marrow Transplant 2013; 19: 260–265.
Merrill RM, Harris JD, Merrill JG . Differences in incidence rates and early detection of cancer among non-Hispanic and Hispanic Whites in the United States. Ethn Dis 2013; 23: 349–355.
Tyson MD 2nd, Castle EP . Racial disparities in survival for patients with clinically localized prostate cancer adjusted for treatment effects. Mayo Clin Proc 2014; 89: 300–307.
Cella DF, Orav EJ, Kornblith AB, Holland JC, Silberfarb PM, Lee KW et al. Socioeconomic status and cancer survival. J Clin Oncol 1991; 9: 1500–1509.
Tao L, Foran JM, Clarke CA, Gomez SL, Keegan TH . Socioeconomic disparities in mortality after diffuse large B-cell lymphoma in the modern treatment era. Blood 2014; 123: 3553–3562.
Lipworth L, Tarone RE, McLaughlin JK . Renal cell cancer among African Americans: an epidemiologic review. BMC Cancer 2011; 11: 133.
Chow WH, Shuch B, Linehan WM, Devesa SS . Racial disparity in renal cell carcinoma patient survival according to demographic and clinical characteristics. Cancer 2013; 119: 388–394.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Ailawadhi, S., Swaika, A., Razavi, P. et al. Variable risk of second primary malignancy in multiple myeloma patients of different ethnic subgroups. Blood Cancer Journal 4, e243 (2014). https://doi.org/10.1038/bcj.2014.63
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bcj.2014.63
This article is cited by
-
Racial differences as predictors of outcomes in young patients with multiple myeloma
Blood Cancer Journal (2022)
-
Treatment-related sequelae in Hodgkin’s lymphoma after mediastinal irradiation
International Journal of Hematology (2022)
-
Effect of autologous hematopoietic stem cell transplant on the development of second primary malignancies in multiple myeloma patients
Blood Cancer Journal (2021)
-
Trends in the risk of second primary malignancies among survivors of chronic lymphocytic leukemia
Blood Cancer Journal (2019)
-
Type of second primary malignancy after achieving complete response by definitive chemoradiation therapy in patients with esophageal squamous cell carcinoma
International Journal of Clinical Oncology (2018)