Abstract
Aim:
To describe the population pharmacokinetic profile of modafinil acid and to compare the extent of metabolism of modafinil into modafinil acid in 5 major ethnic groups (Han, Mongolian, Korean, Uygur, and Hui) of China.
Methods:
In a multi-center, open-label, single dose clinical trial, 49 healthy volunteers from the 5 ethnic groups received 200 mg of modafinil orally. Blood samples for pharmacokinetic evaluation of modafinil and modafinil acid were drawn before and at different time after the administration. Systematic population pharmacokinetic (PopPK) modeling for modafinil acid was conducted, integrating with our previous PopPK model for modafinil. The influence of ethnicity, gender, height, body weight and body mass index (BMI) was estimated. The extent of metabolism of modafinil into modafinil acid, expressed as the relative conversion fraction, was estimated and compared among the 5 ethnic groups.
Results:
When combined with the PopPK model of modafinil, the concentration of modafinil acid versus time profile was best described with a one-compartment model. The typical clearance and volume of distribution for modafinil acid were 4.94 (l/h) and 2.73 (l), respectively. The Korean group had 25% higher clearance, and the Uygur and Hui groups had 12% higher clearance than the Han group. The median for the relative conversion fraction was 0.53 for Koreans, and 0.24 for the other 4 ethnicities.
Conclusion:
Ethnicity has significant influence on the clearance of modafinil acid. When patients in the 5 ethnic groups are administered drugs or prodrugs catalyzed by esterases and/or amidases, the variability in the extent of drug metabolism should be considered.
Similar content being viewed by others
Introduction
Modafinil (2-[(Diphenylmethyl)sulfinyl]acetamide) is a unique wakefulness-promoting agent for oral administration, which was first marketed in France in the early 1990s as a treatment for the excessive somnolence associated with narcolepsy, shift work sleep disorder and obstructive sleep apnea1,2. Modafinil is generally well tolerated, with mild or moderate side effects3.
Modafinil is well absorbed, with an apparent elimination half-life ranging from 10 to 17 h after a single or multiple-dose administration. The major route of elimination is via metabolism, primarily in the liver, with subsequent renal excretion of the metabolites. Modafinil is primarily hydrolyzed by an esterase and/or amidase into modafinil acid, which is the major metabolite1,3. Renal excretion of modafinil represents ≤5% of the dose, while total urinary recovery of modafinil acid accounts for 35% to 51%3.
Hydrolysis occurs mostly in the liver and is one type of Phase I metabolism, which is mostly triggered by esterase and amidase. Esterase splits esters into an acid and an alcohol in a chemical reaction with water. Amidase is an enzyme that catalyzes the hydrolysis of an amide by acting upon amide bonds4. Esterases and amidases play an important role in maintaining normal physiology and metabolism, detoxifying various drugs and environmental toxicants in living systems. There are a number of drugs and prodrugs that have an ester or amide linkage, and these are vulnerable to the activity of esterases and amidases5.
In the present study, the population pharmacokinetic (PopPK) characteristics of modafinil acid were investigated in five major ethnic groups (Han, Mongolian, Korean, Uygur, and Hui) using NONMEM program. This PopPK analysis of modafinil acid is using same group of subjects with our previous reported modeling of modafinil6. The influence of covariates was also evaluated. The pharmacokinetic analysis of both the parent drug and the major metabolite is a key component in drug development7. In this study, we completed a comprehensive pharmacokinetic evaluation of modafinil by combining the PopPK model of modafinil acid with the model of modafinil. In addition, we also estimated and compared the extent of metabolic transformation of modafinil into modafinil acid among the five ethnic groups. Both inter-individual variability in the apparent volume of distribution and AUC were used to estimate the relative metabolic conversion fraction (relative to the typical value of the Han group). When administering drugs or prodrugs that can be hydrolyzed by esterases/amidases, careful consideration should be given to the difference in metabolic conversion fractions among different ethnic groups as the hydrolization or activation of esterases/amidases can markedly differ among these groups.
Materials and methods
Subjects and data collection
We analyzed 637 plasma concentration data from 49 healthy volunteers of the five ethnic groups6. The clinical trial was approved by the Independent Ethical Committee of Shenyang Northern Hospital, and written informed consent was received from all volunteers before starting the study. The families of the subjects from the four ethnic groups (except Han) were all in the same ethnicity for three generations. No medicine was given before the start of the study. Alcohol and smoking were forbidden for at least 72 h before drug administration and during the sampling schedule. All females were tested during luteal phase of their menstrual cycle. Hepatic function and regular blood and biochemical parameters for the subjects were examined and reported within normal range. The demographic characteristics of the subjects are listed in Table 1. Information of the following potential covariates was collected and analyzed: ethnicity, sex, height, weight, and body mass index (BMI). This clinical trial followed the Declaration of Helsinki.
Drug administration and blood sampling
This study was an open-label, multiple-center, single-dose design performed in healthy young males and females. Subjects were fasted for at least eight hours prior to the administration of modafinil. On the morning of Day 1, all subjects received two 100 mg tablets of modafinil (Jiangzhong Pharmaceutical Co, Ltd, China) with 200 mL of water. Blood samples (4 mL) for the pharmacokinetic evaluation of modafinil and modafinil acid were drawn immediately before dose (pre), and at 0.25, 0.5, 1, 1.5, 2, 3, 4, 6, 8, 12, 24, 36, and 48 h postdose. The samples were centrifuged immediately and stored at -20 °C until analyzed. The concentration of modafinil and modafinil acid were determined by a sensitive, specific and validated high-performance liquid chromatography method with ultraviolet detection8. The limit of quantification was 0.1 mg/L for both modafinil and modafinil acid.
Population pharmacokinetic model development
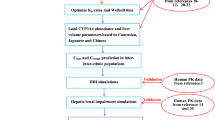
PopPK analysis was performed using the NONMEM program (version VII, level 1, ICON, Ellicott City, MD, USA)9. The first order conditional estimation (FOCE) method with interaction, ADVAN 6 subroutine and L2 option were used. The model structure is shown in Figure 1, and the basic model was characterized by the equations shown below. “A” refers to the amount of modafinil or modafinil acid in the corresponding compartments.
PopPK model structure of modafinil acid, combined with the model of modafinil, comprises of four compartments: gastrointestinal tract (GI), central and peripheral compartment for modafinil, and central compartment for modafinil acid. X1, V1, X2, and V2 are amount (X) and volume of distribution (V) of modafinil in central (systemic circulation and liver) and peripheral (tissues) compartments, respectively. And X3 and V3 are amount and volume of distribution of modafinil acid in its central compartment. Rate constants for the compartments are Ka (absorption), K12, K21, K1m (modafinil is metabolized into modafinil acid) and Km (elimination from central compartment for modafinil acid). F1 is the bioavailability of modafinil, while F2 is the conversion fraction of modafinil to modafinil acid.

PopPK modeling of modafinil acid was performed in a sequential manner10. First, the PopPK model of the parent drug (modafinil) was constructed, and the influence of the candidate covariates was estimated. The candidate covariates are following: age, height, BMI, body weight, gender, ethnicity, ALT, AST, ALP, total bilirubin, total protein, creatinine, BUN, and albumin. Next, we linked the model for modafinil to a one-compartment (Figure 1) and two-compartment models in order to search for a better basic model. A final base model for each compound was built in parallel. Finally, the influence of every candidate covariate was investigated by the forward inclusion-backward elimination method11 resulting in the final PopPK model for modafinil acid. Comparison of the models was based on the objective function value (OFV) provided by NONMEM at a significance level of 0.05 (equal to a decrease of 3.84 in the OFV) for the inclusion, and 0.001 (equal to an increase of 10.83 in the OFV) for the elimination. Besides the change in OFV, the modeling process was also guided by the goodness of fit plots9. Both linear and exponential models were tried for continuous covariates. Discrete covariates, such as ethnicity, were implemented in a categorical way.
Inter-individual variability in parameters was modeled using a statistical model, which is exponentially expressed as following:

where Pij represents the jth basic pharmacokinetic parameter of the ith individual (=individual parameter). It was assumed that all of the values of Pij were log-normally distributed9. PTVj is the typical population value of the jth parameter, and ηij is the deviation of Pij from PTVj with a mean of 0, and an estimated variance of ωj2.
A combined proportional and additive error model was used to describe the residual unexplained variability representing the variance between the observed concentrations and those predicted by the model:

Cobs and Cpred denote the observed and predicted concentrations, respectively. ɛ1 represents random deviation between the predicted and the observed concentration, with a zero mean and variances of σ12.
Model evaluation
The final model was evaluated using nonparametric bootstrap and visual predictive check (VPC)12,13. The resampling was performed 200 times for the bootstrap. The median and the precision of the parameters obtained by this analysis were compared with the ones obtained by NONMEM from the whole original data. VPC was performed by simulating 1000 times from the final model to assess the predictive performance. A graphical comparison was made between the observed data and the model predicted median and 90% prediction interval (90% PI) over time.
Metabolic conversion fraction of modafinil to modafinil acid
Modafinil was primarily hydrolyzed into modafinil acid. The absolute metabolic transformation extent cannot be estimated due to the absence of urinary concentration data for modafinil. In the present study, we estimated the relative metabolic conversion fraction (relative to the typical value of the Han group), instead of calculating the absolute values. We then compared this relative conversion fraction level among the five ethnic groups. The total amount of drug in the body is V×AUC0–∞. The absolute conversion fraction (F2) of modafinil to modafinil acid for the ith individual is as follows.

Where V1i and V3i are the ith individual's volume of distribution of modafinil and modafinil acid, respectively. Equation 1 was combined with equation 3 to give the following (equation 4):

Where V1TV and V3TV are the typical value of volume of distributions for modafinil and modafinil acid, respectively. The actual value of volume of distribution (V1TV, V3TV) cannot be assessed, since we only have oral concentration data. But the difference of V1TV and V3TV among the five ethnicities was estimated by incorporating ethnicity in the PopPK model in a categorical way, which is expressed as θV1×f1 (or θV3×f3). θV1 and θV3 are the typical values of V for Han. f1 and f3 were fixed to 1 for Han, and these were estimated for the four other ethnic groups. Since θV1, as well as θV3, is same for all of the five ethnicities, the relative change of conversion fraction among the five ethnicities is available when replacing the V1TV and V3TV by f1 and f3, respectively, which leads to the relative metabolic conversion fraction (F2', equation 5). Since the inter-individual variability was also included in equation 5, F2' is actually relative to the typical value of the Han group. The AUC0–∞s were calculated by non-compartmental analysis14.

Results
PopPK model of modafinil acid
Compared with the two-compartment model, modafinil acid concentration versus time profile was better described using a one-compartment open model, with lower objective function value (ΔOFV=23.2), which was connected with a two-compartment model of modafinil. The parameters of apparent systemic clearance (CL3/F1F2) and central volume of distribution (V3/F1F2) of modafinil acid corrected by bioavailability (F1) and the conversion fraction from modafinil to modafinil acid (F2) were estimated by this model. The PopPK parameters and the influence of the key covariates of modafinil were also estimated simultaneously. The distribution of random residual errors was expressed using a proportional model to best interpret the unexplained intra-individual variability.
Estimates of the pharmacokinetic parameters of the final model are presented in Table 2. Figure 2 shows the scatter plots of the observed concentration versus the population (Figure 2A) and individual (Figure 2B) predicted concentrations. A good correlation was observed, suggesting that the resulting model fits the observed data. A scatter plot of the conditional weighted residual from the final population model is also shown in Figure 2C, which was symmetrically distributed around the null ordinate with no marked trend over concentrations. The conditional weighted residuals ranged between -3.22 and 3.83. The plot of individual prediction and observation versus time was shown individually in Figure 3.
Ethnicity was proven to have a significant influence on the clearance of modafinil acid. We saw a remarkable improvement in the fit of our model with the inclusion of ethnicity. The OFV decreased 68.327 in the forward process with addition of ethnicity in the clearance of modafinil acid. Compared with the subjects of Han, the clearance showed an increase of 1.25 fold in Korean, 1.15 fold in Uygur or Hui, and the Mongolian group had a similar clearance with Han.
Model evaluation
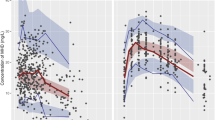
The mean parameter estimates resulting from the bootstrap procedure very closely agreed with the corresponding values from the final population model, indicating that the estimates for the parameters in the final model were accurate and the model was stable. From 200 bootstrap runs, 199 were minimized successfully and were included in the bootstrap analysis. The results of the bootstrap analysis are summarized in Table 2. Figure 4 shows the median and the 5th and 95th percentiles from the simulation as well as the observed data. These plots, representing a visual internal validation, show that most of the observed concentrations fell within the 5th-95th percentile interval. The VPC shows that the final model adequately describes the majority of the data.
Conversion fraction of modafinil to modafinil acid
The relative conversion fraction (F2') of modafinil to modafinil acid was calculated for each individual. The Han, Uygur, Mongolian, and Hui groups have a similar relative conversion fraction (Figure 5A). Hence, we combined these data in one group and compared this with Korean group using a t test. We saw a significant difference between the Korean group and the combination of the other four ethnic groups (P=0.0020, Figure 5B). The Korean group gained a higher relative conversion fraction (0.53±0.43) than the other four ethnicities combined (0.24±0.16).
Discussion
The publication of the FDA Metabolism in Safety Testing (MIST) guidance in 2008 has brought metabolite safety, including the pharmacokinetic analysis of metabolites, into sharper focus15. In this study, we performed a comprehensive pharmacokinetic evaluation of modafinil acid, which completed the entire pharmacokinetic analysis of modafinil by integrating with the previously reported model of modafinil. Covariates were also included in the model to estimate their effects on the pharmacokinetic behavior of modafinil acid.
As shown in the final model, ethnicity has a significant influence on the clearance of modafinil acid. During the modeling process, we observed that Uygur and Hui have a similar influence on the clearance with an increase of 1.13 and 1.15 fold on the Han group. Hence, the data of the Uygur and Hui subjects were combined, and estimates were made from a combined group. It is logical that Uygur and Hui have a similar impact on the pharmacokinetics of modafinil acid, as they live geographically close to each other in China. This result suggests that environmental factors (such as diet) play a significant role in drug metabolism. The Korean group had the highest clearance (1.25 fold higher than the Han group). Modafinil acid is primarily eliminated from the body by kidneys3. The reason for the higher clearance in Koreans is unknown.
Esterases and amidases constitute the third largest group of reactions on drugs and pesticides, behind P450s and UGTs4. Moreover, esterases and amidases are prominent for the prodrugs in transformation steps to yield the active parent drugs. Developing esters or amides is the most common strategy in the development of prodrugs16. It is estimated that approximately 49% of all marketed prodrugs are activated by enzymatic hydrolysis17. In our study, the relative conversion fraction refers to the extent of the metabolism of modafinil into modafinil acid. It is shown to be different among the five ethnic groups (Figure 5). If patients were to take the same dose of an ester prodrug, it could be expected that the Korean group would experience the lowest drug exposure among the five ethnic groups. The mechanism of the esterase/amidase-mediated metabolism is not clear for some drugs, since esterases can overlap in activity with amidases4. Because of this, the differences in drug exposure among the five ethnicities can only be predicted empirically, not quantitatively. The difference in the relative conversion fraction among these five groups seems to suggest that there are very likely gene mutations in the enzymes. We can make a reasonable assumption to perform a genotyping study on the responsible enzyme after the mechanism of the metabolism of modafinil is identified.
Tian et al18 reported an analysis of East Asian population genetic substructure using genome-wide SNP arrays. Mongolian and Korean show differences with Han Chinese. Han group is approximately midway between the Mongolian and Korean groups. In our study, the relative conversion fraction of Han fell between Mongolian and Korean, which is consistent with Tian's results (Figure 5A).
The apparent clearance of modafinil acid (4.94 l/h) is significantly higher than the apparent clearance of modafinil (3.51 l/h) (P<0.0001)6, which follows the idea that metabolism increases polarity and thus increases clearance7. In general, decreasing lipophilicity will reduce the affinity for tissue and plasma protein due to decreased hydrophobic interaction. Both modafinil and modafinil acid have relatively small apparent distribution volumes. In the modeling process, there was a slight influence of age on the volume of distribution and of gender on the clearance, which did not reach the stricter significant criteria during the backward procedure. This discrepancy may be due to the limited age range of the subjects (18–26 years old) in this study. These two covariates should also be considered when younger or older patients receive modafinil19. Gender is one of the key covariates in the model of modafinil, but it does not show any effect on the pharmacokinetics of modafinil acid, which is probably due to joint structure in the model of modafinil and modafinil acid. The clinical biochemical indices (ALT, AST, ALP, total bilirubin, total protein, creatinine, BUN, and albumin) did not show any evident effects on the pharmacokinetics of modafinil and modafinil acid. This needs to be further investigated, since there are only healthy young volunteers in our study.
It is illustrated that the final model fits the observed concentrations well (Figure 2). The conditional weighted residuals were fairly acceptable and evenly distributed around the zero line (Figure 3). The M3 method was applied for the concentration points below LOQ, but it did not improve the model20.
The limitation of this study is whether or not our model will stand for the whole population of gender and ethnicity in China. This study focuses more on the difference in metabolic conversion extent among the five ethnic groups, rather than on prediction of concentration. There is another paper concerning PopPK of modafinil and modafinil acid21. They used AUC ratio of the parent drug and the metabolite as the fraction of metabolic conversion. However, it is well known that the metabolic conversion fraction cannot be estimated without urinary elimination concentration or metabolite alone administration concentration, because the rate of conversion of the parent to the metabolite and the distribution volume of the metabolite are structurally not simultaneously identifiable22. In the current study, we estimated and compared the relative metabolic conversion fraction (relative to the typical value of the Han group) to avoid over-parameterization. The volume of distribution is involved in the calculation of the relative metabolic ratio, which is different with some ideas of the independence between clearance and volume of distribution.
Author contribution
Ke-hua WU, Wei LU, Chen-hui DENG, Zheng GUAN, Liang LI, and Tian-yan ZHOU contributed to the model development. Tao GUO contributed to the clinical trial.
References
Minzenberg MJ, Carter CS . Modafinil: a review of neurochemical actions and effects on cognition. Neuropsychopharmacology 2008; 33: 1477–502.
Wisor JP, Dement WC, Aimone L, Williams M, Bozyczko-Coyne D . Armodafinil, the R-enantiomer of modafinil: Wake-promoting effects and pharmacokinetic profile in the rat. Pharmacol Biochem Behav 2006; 85: 492–9.
Robertson P Jr, Hellriegel ET . Clinical pharmacokinetic profile of modafinil. Clin Pharmacokinet 2003; 42: 123–37.
Guengerich FP . Oxidative, reductive, and hydrolytic metabolism of drugs. In: Zhang DL, Zhu M, Humphreys WG, editors. Drug Metabolism in Drug Design and Development. USA: Wiley; 2008. p 29–31.
Coleman M . Conjugation and transport processes. In: Coleman M, editor. Human Drug Metabolism: An Introduction. London: Wiley-Blackwell; 2010. p 152.
Tao G, Longshan Z, Kehua W, Dongya X, Wei L, Zheng G, et al. Population pharmacokinetics of Modafinil in Chinese Han, Mongolian, Korean, Uygur, and Hui healthy subjects determined by nonlinear mixed-effects modeling. Ther Drug Monit 2010; 32: 189–93.
Nedderman A, Walker D . Metabolite testing in drug development. In: Bonate PL, Howard DR, editors. Pharmacokinetics in Drug Development: Advances and Applications, V 3. USA: Springer; 2011. p 134.
Zhao LS, Xia DY, Guo T . RP-HPLC determination of modafinil and modafinil acid in human plasma. Chin J Pharm anal 2008; 27: 1863–6.
Beal SL, Sheiner LB . NONMEM Users Guides. San Francisco, University of California, 1998.
Lehr T, Staab A, Tillmann C, Trommeshauser D, Raschig A, Schaefer HG, et al. Population pharmacokinetic modeling of NS2330 (tesofensine) and its major metabolite in patients with Alzheimer's disease. Br J Clin Pharmacol 2007; 64: 36–48.
Mandema JW, Verotta D, Sheiner LB . Building population pharmacokinetic-pharmacodynamic models. I. Models for covariate effects. J Pharmacokinet Biopharm 1992; 20: 511–28.
Yano Y, Beal SL, Sheiner LB . Evaluating pharmacokinetic/pharmacodynamic models using the posterior predictive check. J Pharmacokinet Pharmacodyn 2001; 28: 171–92.
Karlsson MO, Holford N . A tutorial on visual predictive checks. Presented at: Annual meeting of the population approach group in Europe (PAGE); June 18–20, 2008: Marseille, Frence.
Weiss M . Drug metabolite kinetics: noncompartmental analysis. Br J Clin Pharmacol 1985; 19: 855–6.
FDA. FDA guidance for industry. Safety testing of drug metabolites. 2008. http://www.fda.gov/cder/guidance/6897fnl.pdf.
Rautio J, Kumpulainen H, Heimbach T, Oliyai R, Oh D, Järvinen T, et al. Prodrugs: design and clinical applications. Nat Rev Drug Discov 2008; 7: 255–70.
Ettmayer P, Amidon GL, Clement B, Testa B . Lessons learned from market and investigational prodrugs. J Med Chem 2004; 47: 2393–404.
Tian C, Kosoy R, Lee A, Ransom M, Belmont JW, Gregersen PK, et al. Analysis of East Asia genetic substructure using genome-wide SNP arrays. PLoS One 2008; 3: e3862.
Xu P, Li HD, Zhang BK, Xiao YW, Yuan HY, Zhu YG . Pharmacokinetics and tolerability of modafinil tablets in Chinese subjects. J Clin Pharm Ther 2008; 33: 429–37.
Ahn JE, Karlsson MO, Dunne A, Ludden TM . Likelihood based approaches to handling data below the quantification limit using NONMEM VI. J Pharmacokinet Pharmacodyn 2008; 35: 401–21.
Seng KY, Fan L, Lee HS, Yong WP, Goh BC, Lee LS . Population pharmacokinetics of modafinil and its acid and sulfone metabolites in Chinese males. Ther Drug Monit 2011; 33: 719–29.
Cosson V, Jorga K, Fuseau E . Modeling of metabolite pharmacokinetics. in: Williams PJ, Ette EI, editors, Pharmacometrics: The Science of Quantitative Pharmacology. USA: Wiley;2007.p 1108.
Acknowledgements
We thank Long-shan ZHAO and Dong-ya XIA for collecting data for this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wu, Kh., Guo, T., Deng, Ch. et al. Population pharmacokinetics of modafinil acid and estimation of the metabolic conversion of modafinil into modafinil acid in 5 major ethnic groups of China. Acta Pharmacol Sin 33, 1401–1408 (2012). https://doi.org/10.1038/aps.2012.124
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2012.124
Keywords
This article is cited by
-
Pharmacometrics: a quantitative tool of pharmacological research
Acta Pharmacologica Sinica (2012)