Abstract
Glycogen storage disease type III (GSD III) is an autosomal recessive disease caused by the deficiency of glycogen-debranching enzyme (AGL). The overall incidence of the disease is about 1:100,000 life births in the USA; however, it is unusually frequent among North African Jews in Israel (prevalence 1:5,400, carrier prevalence 1:35). All North African Jewish GSD III patients examined have both liver and muscle involvement. While all patients showed the characteristic features related to the liver enzyme deficiency, the peripheral muscular impairment varied from minimal to severe, with neuromuscular involvement. A single mutation in the AGL gene, the deletion of T at position 4,455 (4),455delT) in homozygous form, was found in this patient population. The mutation 4,455delT results in the change of 17 amino acids at the carboxy terminus of the AGL protein (1),486–1,502) and truncation of the last 30 amino acids of the normal AGL 1,532 amino acids. The mutation appears to be ethnic specific as it was not seen in 18 patients of different ethnic origins. This is the first report of a mutation in the AGL gene affecting a considerable number of GSD III patients in a defined population.
Similar content being viewed by others
Introduction
Glycogen storage disease type III (GSD III; McKusick, 232,400) is an autosomal recessive disease caused by the deficiency of glycogen-debranching enzyme (amylo-1,6-glucosidase, AGL). AGL contains two catalytic activities: oligo1,4-1,4 glucantransferase (EC 2.4.1.25) and amylo 1,6 glucosidase (EC 3.2.1.33) at two separate sites on a single polypeptide chain with a molecular weight of 174,751 kD [1, 2]. Clinically, deficiency of AGL in humans presents during infancy or early childhood, with hepatomegaly with increased hepatic content of glycogen and triacylglycerol, hypoglycemia, hyperlipidemia (fasting hypertriglyceridemia and hypercholesterolemia) with elevated transaminase, retarded physical growth and a variable degree of myopathy and cardiomyopathy. Patients with this disease show marked heterogeneity both clinically and enzymatically [reviewed in ref. 3, 4]. In most patients, AGL deficiency affects both liver and muscle (subtype IIIa). In patients with GSD type IIIb (∼ 15%), the enzyme is deficient in the liver, but is retained in muscle. The relationships between enzyme deficiency, degree of glycogen accumulation in muscle and clinical features are not clear. Different mutations may provide the molecular basis accounting for the variability in organ involvement and the heterogeneity observed in enzymatic activities. The gene for AGL has been isolated and characterized. It is comprised of 35 exons which span 85 Kb of DNA [5–7]. The length of the cDNA is 7 Kb, and the coding region contains 4,596 bp [5, 7]. Recently, a nonsense mutation due to a single-base insertion in the 3′ coding region of the AGL gene (4),529insA) was shown to be associated with a severe phenotype [8]; a donor splice mutation and a DNA rearrangement were identified in a compound heterozygous Japanese patient [9], and two transition mutations causing stop codons R864X and R1228X were identified in heterozygous form at frequencies of 10.3 and 5.2%, respectively, among 29 Caucasian GSD IIIa and IIIb patients of different ethnic origins (collected in the USA and UK) [10]. Two mutations, 17delAG and Q6X, were shown to be associated with GSD IIIb, but the mechanism underlying the tissue-specific expression of the enzyme is not clear [10].
The overall incidence of the disease is about 1:100,000 life births in the USA; however, it is unusually frequent among North African Jews in Israel (prevalence 1:5,400, carrier prevalence (1:35) [11]. All of them had both liver and muscle involvement; but while characteristic features which relate to the liver enzyme deficiency did not show any unusual pattern, the peripheral muscular impairment varied from minimal to severe, with neuromuscular involvement found in only 1 patient. The present report identifies the mutation causing GSD III in this population.
Materials and Methods
Patients
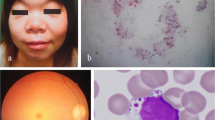
The study was approved by the Soroka Medical Center and Duke University Medical Center institutional review boards. Only patients with enzymatically confirmed diagnosis of GSD III were included in the study. Enzyme activity in all was less than 5% in blood leukocytes or deficient in liver and/or muscle. All presented at young age, with the characteristic hepatic features of disease, i.e. hepatomegaly, fasting hypoglycemia, hyperlipidemia and increased serum transaminase levels. Muscle AGL activity ranged from 0 to 20% of normal; activity was measured as reported elsewhere [12]. Phenotypically, all North African patients had increased serum creatinine kinase activities. Regarding their clinical muscle involvement out of 12 patients studied, 4 had no clinical evidence of myopathy, 6 presented with marked early-onset myopathy which partly improved with age, 1 presented with early-onset myopathy which continues into adult age, while another patient, BN. Y., who developed a rare picture of severely incapacitating late-onset neuromyopathy, is described below. Patients were treated by frequent meals.
BN. Y. presented with typical features of GSD III, with characteristic progress of the disease; he was short and plump and had hepatomegaly and slight transient myopathic features in young age. The patient functioned physically reasonably well until the age of 23, when he developed gradually progressive muscular weakness of the pelvic girdle and extremities, associated with paresthesia. Serum creatinine kinase activities were increased, reaching a maximum of 1,321 U/l (compared to normal activities of up to 190U/l). Electrophysiological studies revealed evidence of myopathic and some neuropathic features. A muscle biopsy showed 18% of normal AGL activity and increased glycogen (4% compared to control 1.2%). Electron microscopic studies of myofibrils showed severe ultrastructural damage. A sural nerve biopsy showed abnormal glycogen accumulation within Schwann cells and axoplasm. After the provision of a high-protein diet and a noctural intragastric administration of an amino acid-glucose solution, he initially responded both clinically and in terms of muscle function tests; however, after a period of poor compliance, his condition deteriorated and did not improve after reinstituting the diet described above. As a result, he became increasingly quadriplegic, suffered from swallowing disturbances causing recurrent aspirations, severe obesity and attacks of sleep apnea which required intranasal continuous positive-pressure ventilation. In addition, he developed severe venous and lymph congestion in his legs, with pressure ulcers. During the years, a gradual and slight functional improvement in selected muscles was noted, enabling him to partially take care of himself and even drive a specially outfitted car. He is presently 40, not keeping any special diet and suffering, in addition to his neuromyopathy, from obesity and peripheral circulatory disturbances. One of his 2 affected brothers, BN. N., aged 36 years, has evidence of nonprogressive slight myopathy, the other brother, BN. J., aged 30 years, has minimal functional limitations.
Single-Strand Conformation Polymorphism Analysis
Single-strand conformation polymorphism (SSCP) analysis was carried out on all 35 exons using primers designed to amplify the coding region and exon-intron junctions. The primers used for SSCP of exon 34 were: forward primer, 5′ (4348–42) GGTATTTATGGTTTTTTTTGTC (4348–21) 3′; reverse primer, 5′ (4481 + 38) ACACTAGTTATGGAAATTACA (4481 + 18) 3′. DNA was labeled by addition of 0.1 µl of 32P-dCTP (3),000 Ci/mmol, 10 Ci/1) in a 10-µl PCR. Cycling conditions were: 94°C for 1 min, 55°C for 1 min and 72°C for 1 min for 30 cycles, then 72°C for 5 min. Two microliters of each amplified sample were added to 8 µl of stop solution (95% formamide, 10 mM EDTA, 0.25% bromophenol blue, 0.25% xylene cyanol). The sample was denatured in a 95°C block and loaded directly onto a 0.75 × MDE gel (FMC, Rockland, Me., USA) and electrophoresed in 0.6 × TBE at 8 W at room temperature for 16 h. The gel was dried on 3MM Whatman paper and exposed to Kodak Biomax AR film overnight.
DNA Sequencing
PCR-amplified genomic DNA fragments were purified using the QIAquick purification kit (Quiagen, Hilden, Germany) and sub-cloned into pGEM-T (Promega, Madison, Wisc., USA). Six subclones of each control and patient DNA were sequenced using Sequenase kit II (USB, Cleveland, Ohio, USA) and the −40 primer of the Sequenase kit.
Restriction Analysis
Genomic DNA was amplified using the primers for exon 34 (above). The amplified fragments were digested with MboII (Fermentas AB, Lithuania) and separated on a 6% Nusieve (FMC) gel in TBE buffer.
Results
Mutation analysis of 1 Jewish North African patient was performed using 35 pairs of PCR primers designed to amplify all AGL exons, the coding region and the exonintron junctions. SSCP analysis on MDE gels was carried out to detect mobility shifts in the patient. The PCR product of exon 34 of the patient and his mother revealed different patterns than that of the normal control (fig. 1). GSD III patients from different ethnic backgrounds (8 Caucasians, 3 African Americans, 5 Arabs, 1 Ashkenazi Jewish and 1 oriental patient) had migration patterns of exon 34 similar to those of the control (data not shown). Genomic DNA of the Jewish North African GSD III patient and a healthy North African Jew were used to amplify exon 34 of the AGL; the PCR products were sub-cloned into the pGEM-T vector, and 6 subclones of each patient and control were sequenced. All clones of the patient revealed a deletion of T at position 4,455 (4),455delT; the assignment of the nucleotide position number was according to the GenBank accession number: BankIt 88587 U84007) (fig. 2). This deletion causes a frameshift starting at amino acid codon 1,486, eliminating the last relevant 47 amino acids at the carboxy terminus of the normal AGL of 1,532 amino acids (changing 17 amino acids following the deletion, then introducing a stop codon which causes premature termination).
The 4,455delT creates a new MboII site in exon 34. The PCR product of this exon is a fragment of 214 bp, and its restriction with MboII results in two fragments of 60 and 154 bp in the normal DNA. The 154-bp fragment is further divided into two fragments of 79 and 75 bp in DNA with the 4,455delT mutation. A family study showed that the patient was homozygous for the mutation, and both parents were heterozygous (fig. 3). The analysis of 12 GSD IIIa patients from 10 families revealed that all of them carried this mutation in the homozygous form. A Jewish patient whose mother is of North African extraction and the father of Yemenite origin was heterozygous for the mutation, as was his mother. Further analysis of 28 healthy Jews of North African extraction did not show the mutation.
Discussion
GSD III patients may occasionally have severe hypoglycemia and seizures. Although in most cases symptomatology improves with age, liver cirrhosis has been reported, myopathy may be incapacitating and cardiac involvement may lead to death [13–15]. In adults, progressive myopathy leading to severe muscular paralysis has been reported [16]. GSD III is generally considered as a mild form of inherited metabolic disease; however, some patients are severely affected. The possibility of a poor course of disease justifies prenatal diagnosis. Prenatal diagnosis is possible by measuring the enzyme activity using a qualitative assay [17] in chorionic villi or amniotic fluid cells [18, 19]. However, the relatively low activity of the enzyme in these tissues and the existence of nonspecific enzyme activities can make the distinction between a heterozygote and an affected fetus difficult in a few cases. Three previous reports of AGL gene mutation analyses in a total of 31 GSD IIIa patients [8–10] did not demonstrate any prevalent mutation. The use of DNA methodology became recently available with the identification of polymorphic markers in the AGL gene which enable linkage analysis in families with GSD III [20]. Our identification of a single prevalent mutation in the North African Jewish population will allow direct DNA prenatal diagnosis for families at risk of GSD IIIa and will provide an easy and reliable screening method for this population who has an unusual high prevalence of the disease (carrier prevalence 1:35) [11]. Thus, the DNA test can be used for premarital genetic counseling and prenatal diagnosis for heterozygote couples for their first born. In a preliminary study, we have identified three restriction fragment length polymorphisms in the AGL gene [21]. Seven North African Jewish GSD III patients of different families presented the same restriction fragment length polymorphism pattern, which was distinct from the normal population, indicating a linkage disequilibrium caused by a founder effect and suggesting a single mutation in this patient population. In the present study, we have identified a single mutation (4),455delT), in homozygous form, which was the only mutation found in 10 Jewish GSD III families of North African extraction. The 4,455delT mutation was not found in 56 normal alleles.
The mutation 4,455delT, resulting in protein truncation, is likely to have a profound deleterious effect on the AGL activity as the putative glycogen-binding domain is located in the carboxy terminus of the AGL [5], although expression studies have not yet been performed. Indeed, the 4,529insA mutation causing the elimination of the last 23 amino acids was associated with a severe phenotype in a GSD III patient [8]. Moreover, specific separate measurements of the oligo1,4-1,4 glucantransferase (EC 2.4.1.25) and amylo 1,6 glucosidase (EC 3.2.1.33) activities demonstrated that both activities were markedly decreased (more than 80%) [12]; thus, the last 47 amino acids are apparently necessary for both activities.
All 12 North African Jewish patients carried the same mutation, compromising their AGL activity in tissues; however, their clinical manifestations varied with respect to muscle involvement. While all had elevated serum creatinine Phosphokinase levels, the muscle symptoms ranged from no clinical evidence of myopathy to a severely incapacitating late-onset neuromyopathy. Our finding suggests that other factors (such as dietary environment or modifying genes) may play a role, accounting for the clinical variability in this population.
References
Gordon RB, Brown DH, Brown BI: Preparation and properties of the glycogen-debranching enzyme from rabbit liver. Biochim Biophys Acta 1972;289:97–107.
Chen Y-T, He JK, Ding JH, Brown BI: Glycogen debranching enzyme: Purification, antibody characterization and immunoblot analyses of type III glycogen storage disease. Am J Hum Genet 1987;41:1002–1015.
Moses SW: Muscle glycogenosis. J Inherit Metab Dis 1990;13:452–460.
Chen Y-T, Burchell A: Glycogen storage disease; in Scriver CR, Beaudet AL, Sly WS, Valle D (eds): The Metabolic and Molecular Bases of Inherited Disease. New York, MacGraw-Hill, 1995, pp 935–965.
Yang B-Z, Ding J-H, Enghild JJ, Bao Y, Chen Y-T: Molecular cloning and nucleotide sequence of a cDNA encoding human muscle glycogen debranching enzyme. J Biol Chem 1992;267:9294–9299.
Liu W, de Castro ML, Takaema J, Bilous PT, Vinayagamoorthy T, Masden NB, Bleackleey C: Molecular cloning, sequencing and analysis of the cDNA for rabbit muscle glycogen de-branching enzyme. Arch Biochem Biophys 1993;306:232–239.
Bao Y, Downson TL Jr, Chen Y-T: Human glycogen debranching enzyme (AGL): Complete structural organization and characterization of the 5′ flanking region. Genomics 1996;38:155–165.
Shen J-J, Bao Y, Chen Y-T: A nonsense mutation due to a single base insertion in the 3′-coding region of glycogen debranching enzyme gene is associated with a severe phenotype in a patient with glycogen storage disease type IIIa. Hum Mutat 1997;9:37–40.
Okubo M, Aoyama Y, Murase T: A novel donor splice site mutation in the glycogen de-branching enzyme gene is associated with glycogen storage disease type III. Biochem Biophys Res Commun 1996;224:493–499.
Shen J-J, Bao Y, Liu H-M, Lee P, Leonard JV, Chen Y-T: Mutations in the glycogen de-branching enzyme gene are associated with glycogen storage disease type III that is differentially expressed in liver and muscle. J Clin Invest 1996;98:352–357.
Moses SW, Bashan N, Skibin A, Biran H, Gutman A: Genetic traits and diseases in the North African Jewish community. Israel J Med Sci 1973;9:1407–1409.
Steinitz K: Laboratory diagnosis of glycogen disease; in Sobota H, Stewart CD (eds): Advances in Clinical Chemistry, vol 9. New York, Academic Press, 1967, pp 227–354.
Miller CG, Alleyne GA, Brooks SEH: Gross cardiac involvement in glycogen storage disease type III. Br Heart J 1972;34:862–864.
Moses SW, Gadoth N, Bashan N, Ben-David E, Slonim A, Wanderman L: Neuromuscular involvement in glycogen storage disease type III. Acta Pediatr Scand 1986; 75:169–185.
Olson LJ, Reeder GS, Noller KL, Edwards WD, Howell RR, Michels W: Cardiac involvement in glycogen storage disease III: Morphologic and biochemical characterization with endomyocardial biopsy. Am J Cardiol 1986;53:980–981.
Di Mauro S, Hartwig GB, Hays R, Eastwood AB, Frauco R, Olarte M, Chang M, Roses AD, Fettel M, Schoenfeldt RS, Stern LZ: Debrancher deficiency: Neuromuscular disorder in 5 adults. Ann Neurol 1978;5:422–436.
Yang B-Z, Ding J-H, Brown BI, Chen Y-T: Definitive prenatal diagnosis for type III glycogen storage disease. Am J Hum Genet 1990;47:735–739.
Shin YS, Reith M, Tausenfreund J, Andres W: First trimester prenatal diagnosis of glycogen storage disease type II and type III. J Inherit Metab Dis 1989;12:289–291.
Maire I, Mandom G, Mathien M: First trimester prenatal diagnosis of glycogen storage disease type III. J Inherit Metab Dis 1989;12:292–294.
Shen J-J, Liu H-M, Bao Y, Chen Y-T: Polymorphic markers of the glycogen debranching enzyme gene allowing linkage analysis in families with glycogen storage disease type III. J Med Genet 1997;34:34–38.
Mishori-Dery A, Bashan N, Moses S, Hershkovitz E, Bao Y, Chen Y-T, Parvari R: RFLPs for linkage analysis in families with glycogen storage disease type III. J Inherit Metab Dis 1995;18:207–210.
Acknowledgments
This work was in part supported by a grant from the Chief Scientist, Israel Ministry of Health (to R.P.), grants from the National Institute of Health DK9078 (to Y.-T.C.), the Muscular Dystrophy Association (to Y.-T.C.) and grant M01-RR30 (National Center of Research Sources, General Clinical Research Center Program). We thank Mrs. Magda Bartal for her excellent technical assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Parvari, R., Moses, S., Shen, J. et al. A Single-Base Deletion in the 3′-Coding Region of Glycogen-Debranching Enzyme Is Prevalent in Glycogen Storage Disease Type IIIA in a Population of North African Jewish Patients. Eur J Hum Genet 5, 266–270 (1997). https://doi.org/10.1007/BF03405928
Received:
Revised:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF03405928