Abstract
Objective:
To test the psychometric soundness of a teamwork climate survey in labor and delivery, examine differences in perceptions of teamwork, and provide benchmarking data.
Design:
Cross-sectional survey of labor and delivery caregivers in 44 hospitals in diverse regions of the US, using the Safety Attitudes Questionnaire teamwork climate scale.
Results:
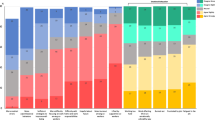
The response rate was 72% (3382 of 4700). The teamwork climate scale had good internal reliability (overall α=0.78). Teamwork climate scale factor structure was confirmed using multilevel confirmatory factor analyses (CFI=0.95, TLI=0.92, RMSEA=0.12, SRMRwithin=0.04, SRMRbetween=0.09). Aggregation of individual-level responses to the L&D unit-level was supported by ICC (1)=0.06 (P<0.001), ICC (2)=0.83 and mean rwg(j)=0.83. ANOVA demonstrated differences between caregivers F (7, 3013)=10.30, P<0.001 and labor and delivery units, F (43, 1022)=3.49, P<0.001. Convergent validity of the scale scores was measured by correlations with external teamwork-related items: collaborative decision making (r=0.780, P<0.001), use of briefings (r=0.496, P<0.001) and perceived adequacy of staffing levels (r=0.593, P<0.001).
Conclusion:
We demonstrate a psychometrically sound teamwork climate scale, correlate it to external teamwork-related items, and provide labor and delivery teamwork benchmarks. Further teamwork climate research should explore the links to clinical and operational outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Kohn L, Corrigan J, Donaldson M . To err is human: building a safer health system. editors. Institute of Medicine Report . National Academy Press: Washington, DC 1999.
ACOG CoQIaPS. ACOG committee opinion: Patient safety in obstetrics and gynecology. Int J Gynecol Obstet 2004; 86: 121–123.
Helmreich R . Managing human error in aviation. Sci Am 1997; 276(5): 62–67.
Helmreich R, Wilhelm J . Outcomes of crew resource management training. Int J Aviat Psychol 1991; 1: 287–300.
Thomas E, Sexton J, Helmreich R . Translating teamwork behaviors from aviation to healthcare: development of behavioral markers for neonatal resuscitation. Qual Saf Health Care 2004; 13(1): i57–i64.
Thomas E, Sherwood G, Mulhollem J, Sexton BJ, Helmreich RL . Working together in the Neonatal Intensive Care Unit: Provider Perspectives. J Perinatol 2004; 24: 552–559.
JCAHO. Preventing infant death and injury during delivery. Sentinel Event Alert 30. 7-21-2004. JCAHO.
JCAHO. Sentinel Event Alert #30: Preventing infant death and injury during deliver. JCAHO. 7-21-2004. http://www.jcaho.org/about+us/news+letters/sentinel+accessed 4-10-2005.
Geller S, Rosenberg B, Cox S . The continuum of maternal morbidity and mortality: factors associated with severity. Am J Obstet Gynecol 2004; 191: 939–944.
Simpson K . Failure to rescue. Implications for evaluating quality of care during labor and birth. J Perinat Neonat Nurs 2005; 19(1): 24–34.
Clarke S, Aiken L . Failure to rescue. Am J Nurs 2003; 103(1): 42–47.
Schein E . Organizational culture. Am Psychologist 1990; 45: 109–119.
Schneider B, Goldstein H, Smith D . The ASA framework: an update. Personnel Psychol 1995; 40: 747–773.
Helmreich R, Merritt A . Culture at Work in Aviation and Medicine: National, Organizational, and Professional Influences. Ashgate Publishing Limited: Aldershot, UK, 1998 p 176.
Helmreich R . Cockpit management attitudes. Human Factors 1984; 26: 583–589.
Helmreich R, Merrrit A, Sherman P, Gregorich S, Wiener E . The flight management attitudes questionnaire (FMAQ). NASA/UT/FAA Technical Report 93–4. Austin, TX: The University of Texas.
Gregorich S, Helmreich R, Wilhelm J . The structure of cockpit management attitudes. J Appl Psychol 1990; 75: 682–690.
Helmreich R, Foushee H, Benson R, Russini W . Cockpit resource management: exploring the attitude-performance linkage. Aviat Space Environ Med 1986; 57(12 Part 1): 1198–1200.
Foushee H . Dyads and triads at 25 000 feet: Factors affecting group process and aircrew performance. Am Psychologist 1984; 39: 885–993.
DeFontes J, Surbida S . Preoperative safety briefing project. Permanente J 2004; 8(2): 21–27.
Pronovost P, Weast B, Rosenstein B, Sexton JB, Holzmueller C, Paine L et al. Implementing and validating a comprehensive unit-based safety program. J Patient Safety 2005; 1(1): 33–40.
Pronovost PJ, Sexton BJ . Assessing safety culture: guidelines and recommendations. Qual Saf Health Care 2005; 14: 231–233.
Sexton J, Makary M, Tersigni A, Pryor D, Helmreich A, Thomas E et al. Teamwork in the operating room: Frontline perspectives among hospitals and operating room personnel. Anesthesiology 2006 in press.
Mearns K, Flin R, Fleming M, Gordon R . Organization and Human Factors in Offshore Safety. HSE: London, 1997.
Trice HM, Beyer JM . The Cultures of Work Organizations. Prentice Hall: Englewood Cliffs, NJ, 1993.
Schein EH . Organizational Culture and Leadership: A Dynamic View. Jossey-Bass: San Francisco, 1992.
Schwartz SH . Universals in the content and structure of values: theoretical advances and empirical tests in 20 countries. In: Zanna MP (ed). Advances in Experimental Social Psychology. Academic Press: San Diego, CA, 1992, pp 1–65.
Schein EH . Organizational culture. Am Psychologist 1990; 45: 109–119.
Ostroff C, Kinicki AJ, Tamkins MM . Organizational culture and climate. In: Borman WC, Ilgen DR, Klimoski RJ (eds). Handbook of Psychology. Wiley & Sons: Hoboken, NJ, 2003, pp 565–594.
Thomas E, Sexton J, Neilands T, Frankel A, Helmreich R . The effect of executive walk rounds on nurse safety climate attitudes. A randomized trial of clinical units. BMC Health Serv Res 2005; 5: 28 doi: 10.1186/1473-6963-5-28 [published online first: 11 April 2005]
Sexton J, Helmreich R, Neilands T, Rowan K, Vella K, Boyden J et al. The Safety Attitudes Questionnaire: psychometric properties, benchmarking data, and emerging research. BMC Health Serv Res 2006; 6(44) doi:10.1186/1472-6963-6-44.
Thomas E, Sexton J, Helmreich R . Discrepant attitudes about teamwork among critical care nurses and physicians. Crit Care Med 2003; 31(3): 956–959.
Muthen B . Multilevel covariance structure analysis. Sociol Methods Res 1994; 22(Multilevel Modeling): 376–398.
Dyer N, Hanges P, Hall R . Applying multilevel confirmatory factor analysis techniques to the study of leadership. Leadership Quart 2005; 16(1): 149–167.
Klein KJ, Kozlowski SWJ . From micro to meso: Critical steps in conceptualizing and conducting multilevel research. Organ Res Meth 2000; 3: 211–236.
James L, Demaree R, Wolf G . Rwg: An assessment of within-group interrater agreement. J Appl Psychol 1984; 78: 306–309.
Bliese P . Within-group agreement, non-independence, and reliability: Implications for data aggregation and analysis. In: Klein K, Kozlowski S (eds). Multilevel Theory, Research, and Methods in Organizations: Foundations, Extensions, and New Directions. Jossey-Bass: San Francisco, 2000, pp 349–381.
Cronbach L . Coefficient alpha and the internal structure of tests. Psychometrika 1951; 16: 297–333.
Wiles R . Teamwork in primary care: the views and experiences of nurses, midwives and health visitors. J Advanced Nurs 1994; 20: 324–330.
Sexton J, Helmreich R, Thomas E . Error, stress and teamwork in medicine and aviation: Cross sectional surveys. Br Med J 2000; 320: 745–749.
Acknowledgements
This work was funded in part by Agency for Healthcare Research and Quality Grant # 1PO1HS1154401
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sexton, J., Holzmueller, C., Pronovost, P. et al. Variation in caregiver perceptions of teamwork climate in labor and delivery units. J Perinatol 26, 463–470 (2006). https://doi.org/10.1038/sj.jp.7211556
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jp.7211556
Keywords
This article is cited by
-
Acute care nurses’ perceptions of leadership, teamwork, turnover intention and patient safety – a mixed methods study
BMC Nursing (2021)
-
Turnover intention of hospital staff in Ontario, Canada: exploring the role of frontline supervisors, teamwork, and mindful organizing
Human Resources for Health (2019)
-
Trauma team leaders’ non-verbal communication: video registration during trauma team training
Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine (2016)
-
Understanding nurses’ and physicians’ fear of repercussions for reporting errors: clinician characteristics, organization demographics, or leadership factors?
BMC Health Services Research (2015)
-
Teamwork Assessment in Internal Medicine: A Systematic Review of Validity Evidence and Outcomes
Journal of General Internal Medicine (2014)