Abstract
OBJECTIVE:
In critically ill neonates, peripheral perfusion and oxygenation assessment may provide indirect information on the circulatory failure of vital organs during circulatory shock. The development of pulse oximetry has recently made it possible to calculate the perfusion index (PI), obtained from the ratio between the pulsatile and nonpulsatile signals of absorbed light. The main goals of this study were: (1) to study foot PI; and (2) to evaluate the relationship between foot PI, obtained continuously by pulse oximetry, and a number of variables, i.e. blood flow (BF), oxygen delivery (DO2), oxygen consumption (VO2), and fractional oxygen extraction (FOE), measured indirectly by near-infrared spectroscopy (NIRS) on the calf in 43 healthy term neonates (weight 3474.6±466.9 g; gestational age 39.1±1.4 weeks).
STUDY DESIGN:
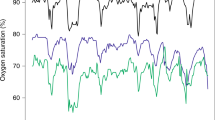
Calf BF, DO2 and VO2 were assessed by NIRS on short-lived venous and arterial occlusion maneuvers. PI was measured on the contralateral foot.
RESULTS:
Foot PI was 1.26±0.39. There was a positive correlation between foot PI and both calf BF (r=0.32, p=0.03) and DO2 (r=0.32, p=0.03), but no correlation was found between foot PI and calf FOE and between foot PI and VO2.
CONCLUSIONS:
In the neonatal intensive care unit, continuously measuring foot PI by pulse oximetry seems clinically more feasible for peripheral perfusion monitoring than spot measurements of the calf BF and/or VO2 by indirect NIRS.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Genzel-Boroviczeny O, Strotgen J, Harris AG, Messmer K, Christ F . Orthogonal polarization spectral imaging (OPS): a novel method to measure the microcirculation in term and preterm infants transcutaneously. Pediatr Res 2002;51:386–391.
Goldman JM, Petterson MT, Kopotic RJ, Barker SJ . Masimo signal extraction pulse oximetry. J Clin Monit Comput 2000;16:475–483.
De Felice C, Latini G, Vacca P, Kopotic RJ . The pulse oximeter perfusion index as a predictor for high illness severity in neonates. Eur J Pediatr 2002;161:561–562.
Hales JR, Stephens FR, Fawcett AA, et al. Observations on a new non-invasive monitor of skin blood flow. Clin Exp Pharmacol Physiol 1989;16:403–415.
Partridge BL . Use of pulse oximetry as a noninvasive indicator of intravascular volume status. J Clin Monit 1987;3:263–268.
Lima AP, Beelen P, Bakker J . Use of a peripheral perfusion index derived from the pulse oximetry signal as a noninvasive indicator of perfusion. Crit Care Med 2002;30:1210–1213.
Nicklin SE, Hassan IA, Wickramasinghe YA, Spencer SA . The light still shines, but not that brightly? The current status of perinatal near infrared spectroscopy. Arch Dis Child Fetal Neonatal Ed 2003;88:F263–F268.
Wardle SP, Weindling AM . Peripheral oxygenation in preterm infants. Clin Perinatol 1999;26:947–966.
Yoxall CW, Weindling AM . The measurement of peripheral venous oxyhemoglobin saturation in newborn infants by near infrared spectroscopy with venous occlusion. Pediatr Res 1996;39:1103–1106.
Hassan IA, Spencer SA, Wickramasinghe YA, Palmer KS . Measurement of peripheral oxygen utilisation in neonates using near infrared spectroscopy: comparison between arterial and venous occlusion methods. Early Hum Dev 2000;57:211–224.
Hassan IA, Wickramasinghe YA, Spencer SA . Effect of limb cooling on peripheral and global oxygen consumption in neonates. Arch Dis Child Fetal Neonatal Ed 2003;88:F139–F142.
Hassan IA, Wickramasinghe YA, Spencer SA . Effect of a change in global metabolic rate on peripheral oxygen consumption in neonates. Arch Dis Child Fetal Neonatal Ed 2003;88:F143–F146.
Suzuki S, Takasaki S, Ozaki T, Kobayashi Y . A tissue oxygenation monitor using NIR spatially resolved spectroscopy. Proc SPIE 1999;3597:582–592.
Duncan A, Meek JH, Clemence M, et al. Optical pathlength measurements on adult head, calf and forearm and the head of the newborn infant using phase resolved optical spectroscopy. Phys Med Biol 1995;40:295–304.
De Blasi RA, Ferrari M, Natali A, Conti G, Mega A, Gasparetto A . Noninvasive measurement of forearm blood flow and oxygen consumption by near-infrared spectroscopy. J Appl Physiol 1994;76:1388–1393.
Bay-Hansen R, Elfving B, Greisen G . Use of near infrared spectroscopy for estimation of peripheral venous saturation in newborns: comparison with co-oximetry of central venous blood. Biol Neonate 2002;82:1–8.
De Blasi RA, Cope M, Elwell C, Safoue F, Ferrari M . Noninvasive measurement of human forearm oxygen consumption by near infrared spectroscopy. Eur J Appl Physiol Occup Physiol 1993;67:20–25.
Wardle SP, Yoxall W, Crawley E, Weindling AM . Peripheral oxygenation and anemia in preterm babies. Pediatr Res 1998;44:125–131.
Girardis M, Rinaldi L, Busani S, Flore I, Mauro S, Pasetto A . Muscle perfusion and oxygen consumption by near-infrared spectroscopy in septic-shock and non-septic-shock patients. Intensive Care Med 2003;29:1173–1176.
Winter DA . A new definition of mechanical work done in human movement. J Appl Physiol 1979;46:79–83.
Harbage B, Dean AG . Distribution of Epi Info software: an evaluation using the internet. Am J Prev Med 1999;16:314–317.
Wardle SP, Yoxall CW, Weindling M . Peripheral oxygenation in hypotensive preterm babies. Pediatr Res 1999;45:343–349.
De Felice C, Flori ML, Pellegrino M, et al. Predictive value of skin color for illness severity in the high-risk newborn. Pediatr Res 2002;51:100–105.
Beinder E, Trojan A, Bucher HU, Huch A, Huch R . Control of skin blood flow in pre- and full-term infants. Biol Neonate 1994;65:7–15.
Wardle SP, Weindling AM . Peripheral fractional oxygen extraction and other measures of tissue oxygenation to guide blood transfusions in preterm infants. Semin Perinatol 2001;25:60–64.
Slaaf DW, Oude Egbrink MG . Capillaries and flow redistribution play an important role in muscle blood flow reserve capacity. J Mal Vasc 2002;27:63–67.
Van Beekvelt MC, Colier WN, Wevers RA, Van Engelen BG . Performance of near-infrared spectroscopy in measuring local O2 consumption and blood flow in skeletal muscle. J Appl Physiol 2001;90:511–519.
Astiz ME, Rackow EC, Falk JL, Kaufman BS, Weil MH . Oxygen delivery and consumption in patients with hyperdynamic septic shock. Crit Care Med 1987;15:26–28.
Fink M . Cytopathic hypoxia in sepsis. Acta Anaesthesiol Scand Suppl 1997;110:87–95.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Zaramella, P., Freato, F., Quaresima, V. et al. Foot Pulse Oximeter Perfusion Index Correlates with Calf Muscle Perfusion Measured by Near-Infrared Spectroscopy in Healthy Neonates. J Perinatol 25, 417–422 (2005). https://doi.org/10.1038/sj.jp.7211328
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jp.7211328
This article is cited by
-
Relationship between perfusion index and patent ductus arteriosus in preterm infants
Pediatric Research (2017)
-
Oxymétrie pulsée : contribution au diagnostic et à l’approche hémodynamique en pédiatrie
Réanimation (2015)
-
Perfusion index as a possible predictor for postanesthetic shivering
Journal of Anesthesia (2014)
-
Reference values of perfusion indices in hemodynamically stable newborns during the early neonatal period
European Journal of Pediatrics (2014)
-
The perfusion index derived from a pulse oximeter for predicting low superior vena cava flow in very low birth weight infants
Journal of Perinatology (2010)