Abstract
The current focus of nutritional science has shifted from meeting needs to determining the biological effects that nutrition has on immediate and lifetime health. Of particular interest is the concept of programming, the idea that “a stimulus or insult during a critical or sensitive period of development can have long-term or lifetime effects on an organism.” Evidence that early nutrition has such “programming” effects in animals is overwhelming. In humans, retrospective observations show a relationship between adult disease and size in early life, though it is difficult to prove nutritional cause from observational associations and therefore difficult to use such data to underpin health policy. However, the results of randomized intervention trials of early nutrition with long-term follow-up are emerging. These experimental studies show that nutrition in early life has a major impact on health into early adulthood, notably on cardiovascular disease risk, bone health and cognitive function. These new findings have major biological, social and medical implications and should increasingly underpin health practices.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Lucas A, Cole TJ . Breast milk and neonatal necrotising enterocolitis. Lancet 1990;336:1519–1523.
Lucas A . Programming by early nutrition in man In: Bock GR, Whelan J, editors. The Childhood Environment and Adult Disease. CIBA Foundation Symposium 156. Chichester: Wiley; 1991; 38–55.
Angelbeck JH, DuBrul EF . The effect of neonatal testosterone on specific male and female patterns of phosphorylated cytosolic proteins in the rat preoptic-hypothalamus, cortex and amygdala. Brain Res 1983;264:277–283.
McCance RA . Food growth and time. Lancet 1962;2:271–272.
Smart J . Undernutrition, learning and memory: review of experimental studies In: Taylor TG, Jenkins NK, editors Proceedings of XII International Congress of Nutrition 1986. London, UK: John Libbey; p. 74–78.
Hahn P . Effect of litter size on plasma cholesterol and insulin and some liver and adipose tissue enzymes in adult rodents. J Nutr 1984;114:1231–1234.
Lewis DS, Bartrand HA, McMahan CA, McGill Jr HC, Carey KD, Masoro EJ . Preweaning food intake influences the adiposity of young adult baboons. J Clin Invest 1986;78:899–905.
Ozanne SE, Hales CN . Catch-up growth and obesity in male mice. Nature 2004;427:411–412.
Barker DJP . Fetal nutrition and cardiovascular disease in adult life. Lancet 1993;341:938–941.
Singhal A, Lucas A . Early origins of cardiovascular disease. Is there a unifying hypothesis? Lancet 2004;363:1642–1645.
Lucas A, Morley R, Cole TJ . Randomised trial of early diet in preterm babies and later intelligence quotient. Br Med J 1998;317:1481–1487.
Florey C, du V, Leech AM, Blackhall A . Infant feeding and mental and motor development at 18 months of age in first born singletons. Int J Epidemiol 1995;24:S21–S26.
Lucas A, Morley R . Breast milk and subsequent intelligence quotient in children born preterm. Lancet 1991;339:261–264.
Grantham-McGregor S . Field studies in early nutrition and later achievement In: Dobbing J, editor Early Nutrition and Later Achievement. London: Academic Press; 1987; 128–174.
Freeman HE, Klein RE, Townsend JW, Lechtig A . Nutrition and cognitive development among rural Guatemalan children. Am J Public Health 1980;70:1277–1285.
Lucas A, Morley R, Cole TJ, et al Early diet in preterm babies and developmental status at 18 months. Lancet 1990;335:1477-1481.
Fewtrell MS, Prentice A, Jones SC, Lunt M, Cole TJ, Lucas A . Bone mineralization and turnover in preterm infants at 8–12 years of age; the effects of early diet. J Bone Miner Res 1999;14:810–820.
Fall CHD, Barker DJP, Osmond C, Winter PD, Clark PMS, Hales CN . Relation of infant feeding to adult serum cholesterol concentration and death from ischaemic heart disease. BMJ 1992;304:801–805.
Owen CG, Whincup PH, Odoki K, Gilg JA, Cook DG . Infant feeding and blood cholesterol: a study in adolescents and a systematic review. Pediatrics 2002;110:597–608.
Von Kries R, Koletzko B, Sauerwald T, et al. Breast-feeding and obesity; cross sectional study. BMJ 1999;319:147–150.
Pettitt DJ, Forman MR, Hanson RL, Knowler WC, Bennett PH . Breastfeeding and incidence of non-insulin-dependent diabetes mellitus in Pima Indians. Lancet 1997;350:166–168.
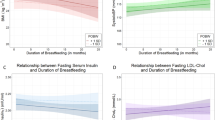
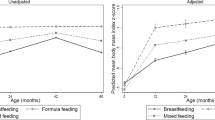
Singhal A, Cole TJ, Lucas A . Early nutrition in preterm infants and later blood pressure: two cohorts after randomised trials. Lancet 2001;357:413–419.
Singhal A, Cole TJ, Fewtrell M, Lucas A . Breast-milk feeding and the lipoprotein profile in adolescents born preterm. Lancet 2004;363:1571–1578.
Singhal A, Fewtrell M, Cole TJ, Lucas A . Low nutrient intake and early growth for later insulin resistance in adolescents born preterm. Lancet 2003;361:1089–1097.
Singhal A, Sadaf Farooqi I, O'Rahilly S, Cole TJ, Fewtrell MS, Lucas A . Early nutrition and leptin concentrations in later life. Am J Clin Nutr 2002;75:993–999.
Singhal A, Cole TJ, Fewtrell M, Deanfield J, Lucas A . Is slower early growth beneficial for long-term cardiovascular health? Circulation 2004;109:1108–1113.
Metcalfe NB, Monaghan P . Compensation for a bad start: grow now, pay later? Trends Ecol Evol 2001;16:254–260.
Forsen T, Eriksson J, Tuomilehto J, Reunanen A, Osmond C, Barker D . The fetal and childhood growth of persons who develop type 2 diabetes. Ann Intern Med 2000;133:176–182.
Wilson AC, Forsyth JS, Greene SA, Irvine L, Hau C, Howie PW . Relation of infant diet to childhood health: seven year follow up of cohort of children in Dundee infant feeding study. BMJ 1998;316:21–25.
Martin RM, McCarthy A, Smith Davey G, Davies DP, Ben-Schlomo Y . Infant nutrition and blood pressure in early adulthood: the Barry Caerphilly Growth Study. Am J Clin Nutr 2003;77:1489–1497.
Desai M, Crowther NJ, Ozanne SE, Lucas A, Hales CN . Adult glucose and lipid metabolism may be programmed during fetal life. Biochem Soc Trans 1995;23:331–335.
Snoek A, Remacle C, Reusens B, Hoet JJ . Effect of a low protein diet during pregnancy on the fetal rat endocrine pancreas. Biol Neonate 1990;57:107–118.
Morley R, Fewtrell MS, Abbott RA, Stephenson T, MacFadyen UM, Lucas A . Neurodevelopment in children born small for gestational age; a randomized trial of nutrient enriched versus standard formula, and comparison with a reference breast fed group. Pediatrics 2004;113:515–521.
Author information
Authors and Affiliations
Additional information
This research was supported by Farleys, Mead Johnson Nutritionals, Nutricia, Ross Labs, Wyeth Pharmaceuticals.
Rights and permissions
About this article
Cite this article
Lucas, A. Long-Term Programming Effects of Early Nutrition — Implications for the Preterm Infant. J Perinatol 25 (Suppl 2), S2–S6 (2005). https://doi.org/10.1038/sj.jp.7211308
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jp.7211308
This article is cited by
-
The effect of massage on feeding intolerance in preterm infants: a systematic review and meta-analysis study
Italian Journal of Pediatrics (2020)
-
The risk of small for gestational age in very low birth weight infants born to Asian or Pacific Islander mothers in California
Journal of Perinatology (2020)
-
Colonic Bacteroides are positively associated with trabecular bone structure and programmed by maternal vitamin D in male but not female offspring in an obesogenic environment
International Journal of Obesity (2018)
-
Association of maternal breast milk and serum levels of macronutrients, hormones, and maternal body composition with infant’s body weight
European Journal of Clinical Nutrition (2018)
-
Impact of body size, nutrition and socioeconomic position in early life on the epigenome: a systematic review protocol
Systematic Reviews (2017)