Abstract
OBJECTIVE: To examine maternal and neonatal outcomes in expectant management of spontaneous preterm premature rupture of membranes (PPROM) before 24 weeks.
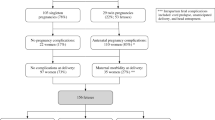
STUDY DESIGN: Patients presenting with spontaneous PPROM from 14 to 23 completed weeks' gestation between January 1, 1995 and December 31, 1999 were reviewed. A total of 108 pregnancies were evaluated; 57 patients elected expectant management.
RESULTS: Median latency from rupture of membranes (ROM) to delivery was 6 days; the overall survival rate was 26.3%. In ROM <20 weeks, a twin and a triplet pregnancy with loss of the presenting fetuses yielded the only survivors. In patients with ROM from 20 to 21 and 22 to 23 weeks, survival rates were 2/16 (12.5%) and 11/20 (55.0%), respectively. In all, 18/57 (31.6%) of patients developed chorioamnionitis. There was no maternal sepsis or death. There were three cases of pulmonary hypoplasia, all in patients with ROM <20 weeks.
CONCLUSIONS: Neonatal survival in spontaneous PPROM before 20 weeks is rare, irrespective of latency from ROM to delivery. When PPROM occurs from 20 to 24 weeks, survival improves with increasing gestational age at ROM and at delivery.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Nimrod C, Varela-Gittings F, Machin G, Campbell D, Wesenberg R . The effect of very prolonged membrane rupture on fetal development. Am J Obstet Gynecol 1984;148:540–543.
Thomas IT, Smith DW . Oligohydramnios, cause of the nonrenal features of Potter's syndrome, including pulmonary hypoplasia. J Pediatrics 1974;84:811.
Beydoun SN, Yasin SY . Premature rupture of the membranes before 28 weeks: conservative management. Am J Obstet Gynecol 1986;155:471–479.
Taylor J, Garite TJ . Premature rupture of membranes before fetal viability. Obstet Gynecol 1984;64:615–620.
Blott M, Greenough A . Neonatal outcome after prolonged rupture of the membranes starting in the second trimester. Arch Dis Child 1988;63:1146–1150.
Moretti M, Sibai BM . Maternal and perinatal outcome of expectant management of premature rupture of membranes in the midtrimester. Am J Obstet Gynecol 1988;159:390–396.
Bengston JM, VanMarter LJ, Barss VA, Greene MF, Tuomala RE, Epstein MF . Pregnancy outcome after premature rupture of the membranes at or before 26 weeks' gestation. Obstet Gynecol 1989;73:921–926.
Morales WJ, Talley T . Premature rupture of membranes at <25 weeks: a management dilemma. Am J Obstet Gynecol 1993;168:503–507.
Rotschild A, Ling EW, Puterman ML, Farquharson D . Neonatal outcome after prolonged preterm rupture of the membranes. Am J Obstet Gynecol 1990;162:46–52.
Rib DM, Sherer DM, Woods JR . Maternal and neonatal outcome associated with prolonged premature rupture of membranes below 26 weeks' gestation. Am J Perinatol 1993;10:369–373.
Major CA, Kitzmiller JL . Perinatal survival with expectant management of midtrimester rupture of membranes. Am J Obstet Gynecol 1990;163:838–844.
Hibbard JU, Hibbard MC, Isamail M, Arendt E . Pregnancy outcone after expectant management of premature rupture of the membranes in the second trimester. J Reprod Med 1993;38:951.
Fortunato SJ, Welt SI, Eggleston MK, Bryant EC . Active expectant management in very early gestations complicated by premature rupture of the fetal membranes. J Reprod Med 1994;39:13–16.
Hadi HA, Hodson CA, Strickland D . Premature rupture of the membranes between 20 and 25 weeks' gestation: role of amniotic fluid volume in perinatal outcome. Am J Obstet Gynecol 1994;170:1139–1144.
Farooqi A, Holmgren PA, Engberg S, Serenius F . Survival and 2-year outcome with expectant management of second-trimester rupture of membranes. Obstet Gynecol 1998;92:895–901.
Kurkinen-Raty M, Koivisto M, Jouppila P . Perinatal and neonatal outcome and late pulmonary sequelae in infants born after preterm premature rupture of membranes. Obstet Gynecol 1998;92:408–415.
Shumway JB, Al-Malt A, Amon E, et al. Impact of oligohydramnios on maternal and perinatal outcomes of spontaneous premature rupture of membranes at 18–28 weeks. J Matern Fetal Med 1999;8:20–23.
Grisaru-Granovsky S, Eitan R, Kaplan M, Samueloff A . Expectant management of midtrimester premature rupture of membranes: a plea for limits. J Perinatol 2003;23:235–239.
Doubilet PM, Benson CB . Gestational age In: Meire HB, Cosgrove D, Dwbury K, editors. Clinical Ultrasound: Ultrasound in Obstetrics and Gynecology. 2nd ed, Vol. 3. London: Churchill Livingstone; 2001 p. 213–222.
Borgida AF, Mills AA, Feldman DM, Rodis JF, Egan JFX . Outcome of pregnancies complicated by ruptured membranes after genetic amniocentesis. Am J Obstet Gynecol 2000;183:937–939.
Porreco RP, Sabin ED, Heyborne KD, Lindsay LG . Delayed-interval delivery in multifetal pregnancy. Am J Obstet Gynecol 1998;178:20–23.
Nimrod C, Varela-Gittings F, Machin G, Campbell D, Wesenberg R . The effect of very prolonged membrane rupture on fetal development. Am J Obstet Gynecol 1984;148:540–543.
Mercer BM, Miodovnik M, Thurnau GR, et al. Antiobiotic therapy for reduction of infant morbidity after preterm premature rupture of membranes: a randomized controlled trial. JAMA 1997;278:989–995.
McElrath TF, Robinson JN, Ecker JL, Ringer SA, Norwitz ER . Neonatal outcome of infants born at 23 weeks' gestation. Obstet Gynecol 2001;91:49–52.
Mercer BM, Crocker RN, Peirce F, Sibai BM . Clinical characteristics and outcome of twin gestation complicated by preterm premature rupture of the membranes. Am J Obstet Gynecol 1993;168:1467–1473.
Fortunato SF, Welt SI, Eggleston MK, Bryant EC . Active expectant management in very early gestations complicated by premature rupture of the fetal membranes. J Reprod Med 1994;39:13–16.
Beydoun SN, Yasin SY . Premature rupture of the membranes before 28 weeks: conservative management. Am J Obstet Gynecol 1986;155:471–479.
Farooqi A, Holmgren PA, Engberg S, Serenius F . Survival and 2-year outcome with expectant management of second-trimester rupture of membranes. Obstet Gynecol 1998;92:895–901.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Falk, S., Campbell, L., Lee-Parritz, A. et al. Expectant Management in Spontaneous Preterm Premature Rupture of Membranes between 14 and 24 Weeks' Gestation. J Perinatol 24, 611–616 (2004). https://doi.org/10.1038/sj.jp.7211163
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jp.7211163
This article is cited by
-
Offering induction of labor for 22-week premature rupture of membranes: a survey of obstetricians
Journal of Perinatology (2015)
-
Rupture of membranes before the age of viability and birth after the age of viability: comparison of outcomes in a matched cohort study
Journal of Perinatology (2010)