Abstract
OBJECTIVE: To determine if preterm infants of higher-order multiple (HOM) gestations have a significantly worse outcome during hospital stay when compared with preterm twins.
STUDY DESIGN: Retrospective cohort analysis.
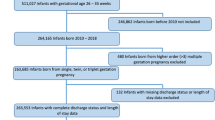
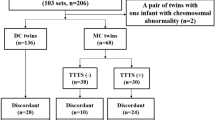
METHODS: Perinatal outcome variables including gestational age (GA), birthweight, prenatal steroid use, cesarean section delivery rate, Apgar scores, and growth retardation were analyzed for 106 preterm HOM births (triplets and quadruplets) versus 328 preterm twins admitted to a single tertiary level neonatal intensive care unit. A comparison of the mortality and major neonatal morbidities such as respiratory distress syndrome, patent ductus arteriosus, intraventricular hemorrhage, necrotizing enterocolitis, bronchopulmonary dysplasia, and retinopathy of prematurity was made for these two groups. In addition, the duration of respiratory support including surfactant therapy, nasal continuous positive airway pressure, and mechanical ventilation, as well as the length of hospitalization, was analyzed.
RESULTS: There were no significant differences in major morbidities between the infants of HOM and twin births of similar GA. There was no statistically significant difference in mortality, but the data showed a trend for lesser mortality in HOM. There was a highly significant increase in antenatal steroid use as well as the use of cesarean section for delivery in the HOM when compared with twin gestations. The infants of HOM gestations were of significantly lower birthweight than the twins and had a longer hospitalization.
CONCLUSION: Although premature infants of HOM had lower birthweight and needed a longer hospital stay, their mortality and morbidity at hospital discharge were not worse than that for preterm twins.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Loucopoulos A, Jewelewicz R Management of multifetal pregnancies: sixteen years' experience at the Sloan Hospital for Women Am J Obstet Gynecol 1982 143 902–5
Ron-El R, Caspi E, Schreyer P, Weinraub Z, Arieli S, Goldberg MD Triplet and quadruplet pregnancies and management Obstet Gynecol 1981 57 458–63
Martin JA, MacDorman MF, Mathews TJ Triplet births: trends and outcomes 1971–94 Vital Health Stat 1997 21 1–20
Luke B, Keith LG The contribution of singletons, twins and triplets to low birth weight, infant mortality and handicap in the United States J Reprod Med 1992 37 661–6
Holcberg G, Biale Y, Lewenthal H, Insler V Outcome of pregnancy in 31 triplet gestations Obstet Gynecol 1982 59 472–6
Olofsson P Triplet and quadruplet pregnancies — a forthcoming challenge also for the “general” obstetrician Eur J Obstet Gynecol Reprod Biol 1990 35 159–71
Melgar CA, Rosenfeld DL, Rawlinson K, Greenberg M Perinatal outcome after multifetal reduction to twins compared with nonreduced multiple gestations Obstet Gynecol 1991 78 763–7
Boulot P, Hedon B, Pelliccia G, et al Obstetrical results after embryonic reductions performed on 34 multiple pregnancies Hum Reprod 1990 5 1009–13
Angel JL, Kalter CS, Morales WJ, Rasmussen C, Caron L Aggressive perinatal care for high-order multiple gestations: does good perinatal outcome justify aggressive assisted reproductive techniques? Am J Obstet Gynecol 1999 181 253–9
Skrablin S, Kuvacic I, Pavicic D, Kalafatic D, Goluza T Maternal neonatal outcome in quadruplet and quintuplet versus triplet gestations Eur J Obstet Gynecol Reprod Biol 2000 88 147–52
Wolf EJ, Vintzileos AM, Rosenkrantz TS, Rodis JF, Lettieri L, Mallozzi A A comparison of pre-discharge survival and morbidity in singleton and twin very-low-birth-weight infants Obstet Gynecol 1992 80 436–9
Sassoon DA, Castro L, Davis J, Hobel CJ Perinatal outcome in triplet versus twin gestations Obstet Gynecol 1990 75 817–20
Ballard JL, Novak KK, Driver M A simplified score for assessment of fetal maturation of newly born infants J Pediatr 1979 95 769–74
Kattner E, Metze B, Waiss E, Obladen M Accelerated lung maturation following maternal steroid treatment in infants born before 30 weeks gestation J Perinat Med 1992 20 449–57
Lubchenco LO, Hansman C, Boyd E Intrauterine growth in length and head circumference as estimated from live births at gestational ages from 26 to 42 weeks Pediatrics 1966 37 403–8
Boyle RJ, Oh W Respiratory distress syndrome Clin Perinatol 1978 5 283–97
Friedman WF, Fitzpatrick KM, Merritt TA, Feldman BH The patent ductus arteriosus Clin Perinatol 1978 5 411–36
Papile LA, Burstein J, Burstein R, Koffler H Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm J Pediatr 1978 92 529–34
Banker BQ, Larroche J-C Periventricular leukomalacia of infancy: a form of neonatal anoxic encephalopathy Arch Neurol 1962 7 386–410
Volpe JJ Hypoxic–ischemic encephalopathy: neuropathology and pathogenesis Neurology of the Newborn 3rd ed Philadelphia: W.B. Saunders 1987
Anonymous An international classification for retinopathy of prematurity. The Committee for the Classification of Retinopathy of Prematurity Arch Ophthal 1984 102 1130
Northway WH Jr, Rosan RC, Porter DY Pulmonary disease following respirator therapy of hyaline membrane disease. Bronchopulmonary dysplasia N Engl J Med 1967 276 357–68
Shennan AT, Dunn MS, Ohlsson A, Lennox K, Hoskins EM Abnormal pulmonary outcomes in premature infants: prediction from oxygen requirement in the neonatal period Pediatrics 1988 82 527–32
Luke B The changing pattern of multiple births in the United States: maternal and infant characteristics, 1973 and 1990 Obstet Gynecol 1994 84 101–6
Porreco RP, Burke MS, Hendrix ML Multifetal reduction of triplets and pregnancy outcome Obstet Gynecol 1991 78 335–9
Lipitz S, Reichman B, Paret G, et al The improving outcome of triplet pregnancies Am J Obstet Gynecol 1989 161 1279–84
Albrecht JL, Tomich PG The maternal and neonatal outcome of triplet gestations Am J Obstet Gynecol 1996 174 1551–6
Papiernik E, Grange G, Zeitlin J Should multifetal pregnancy reduction be used for prevention of preterm deliveries in triplet or higher-order multiple pregnancies? J Perinat Med 1998 26 365–70
Elster AD, Bleyl JL, Craven TE Birth weight standards for triplets under modern obstetric care in the United States, 1984–1989 Obstet Gynecol 1991 77 387–93
Boulot P, Hedon B, Pelliccia G, Peray P, Laffargue F, Viala JL Effects of selective reduction in triplet gestation: a comparative study of 80 cases managed with or without this procedure Fertil Steril 1993 60 497–503
Syrop CH, Varner MW Triplet gestation: maternal and neonatal implications Acta Genet Med Gemellol 1985 34 81–8
Collins MS, Bleyl JA Seventy-one quadruplet pregnancies: management and outcome Am J Obstet Gynecol 1990 162 1384–91 discussion 1391–2
Newman RB, Hamer C, Miller MC Outpatient triplet management: a contemporary review Am J Obstet Gynecol 1989 161 547–53 discussion 553–5
Gonen R, Heyman E, Asztalos EV, et al The outcome of triplet, quadruplet, and quintuplet pregnancies managed in a perinatal unit: obstetric, neonatal, and follow-up data [see comments] Am J Obstet Gynecol 1990 162 454–9
Acknowledgements
We thank Marlene Holman, RN, Paula Gendreau, RN, Marta Baker, RN, and Barbara Westman, Administrative Program Assistant, for their invaluable help with data collection and maintenance of our neonatal database.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Suri, K., Bhandari, V., Lerer, T. et al. Morbidity and Mortality of Preterm Twins and Higher-Order Multiple Births. J Perinatol 21, 293–299 (2001). https://doi.org/10.1038/sj.jp.7200492
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jp.7200492
This article is cited by
-
Outcomes of multiple gestation births compared to singleton: analysis of multicenter KID database
Maternal Health, Neonatology and Perinatology (2021)
-
Trends of infant mortality and its determinants in Ethiopia: mixed-effect binary logistic regression and multivariate decomposition analysis
BMC Pregnancy and Childbirth (2021)
-
Birth Characteristics Associated With Early Intervention Referral, Evaluation for Eligibility, and Program Eligibility in the First Year of Life
Maternal and Child Health Journal (2006)
-
Five cases of dizygotic triplet pregnancy following assisted reproductive techniques
Reproductive Medicine and Biology (2005)
-
Triplet Morbidity and Mortality in a Large Case Series
Journal of Perinatology (2003)