Abstract
Data sources
PubMed, Web of Science, ScienceDirect, Chinese Biological Medical Literature Database, Chinese Wanfang Database, Chinese National Knowledge Infrastructure and reference lists of key publications. Language restrictions were placed with inclusion of English and Chinese texts only. No date restrictions were applied.
Study selection
Original population-based studies that described the diagnostic criteria of MIH and provided prevalence data or sufficient information that could be used to calculate MIH prevalence.
Data extraction and synthesis
Two reviewers independently extracted the data. Meta-regression was done using a random effects model for parameters of age, gender and region. Heterogeneity was assessed using I2 statistic.
Results
Seventy studies were included that encompassed a total of 89,520 people and 10,823 cases of MIH. The pooled global prevalence of MIH was 14.2% (95% CI 12.6-15.8), with South America having the highest prevalence (18%; 95% CI 13.8-22.2) and Africa the lowest (10.9%; 95% CI 4.2-17.6). There was no significant difference between male and female participants. Prevalence of MIH amongst children ten years of age or younger (15.1%, 95% CI 12.1-18.2) was higher than older children (12.1%, 95% CI 8.0-16.3).
Conclusions
This meta-analysis showed the average global prevalence of MIH as 14.2%. Some geographic regions had higher than average prevalence, which could inform oral health policy in those areas.
Similar content being viewed by others
Commentary
Molar incisor hypomineralisation (MIH) is defined as an acquired qualitative defect of systemic origin, affecting one to four first permanent molars and frequently incisors.1 Clinically, MIH affected teeth exhibit demarcated opacities varying in colour and size. The hypomineralised enamel substructure can predispose patients to plaque stagnation, rapid progression of dental caries with cavitation and thermal sensitivity causing pain and discomfort. Enamel changes in affected teeth make them brittle and prone to post-eruptive breakdown, most commonly seen in molars due to their increased occlusal load.2,3 The aetiology of MIH has been linked to early childhood or prenatal conditions such as otitis media, chicken pox, respiratory diseases, medications (antibiotics, asthma medications) and environmental exposures (dioxins and bisphenol A).4 In addition, twin studies indicate a genetic predisposition may occur, however further epigenetic analysis is needed.5 Treatment of MIH can be complex and challenging in the young patient with prognosis of affected teeth variable.6,7 The authors of this study aimed to perform a meta-analysis to estimate the global prevalence of MIH.
Electronic search of databases (PubMed, Web of Science, ScienceDirect, Chinese Biological Medical Literature Database, Chinese Wanfang Database and Chinese National Knowledge Infrastructure) was carried out. In addition, reference lists of key publications were manually searched, although these publications were not explicitly identified. It may have been beneficial to search the reference lists of included studies. In addition, the authors could have expanded their search to include grey literature from the OpenGrey database.
Inclusion criteria included original population-based studies where prevalence was provided or sufficient raw data available to calculate MIH prevalence. Studies needed to specify the diagnostic criteria of MIH and only publications in English or Chinese were accepted. Given the aim of the study was to identify global population prevalence, the exclusion of publications in other languages may have been a limiting factor in their search strategy. Studies were excluded if they had published duplicate data previously or if the study was based on a specific population (for example, children born preterm). If there were multiple articles based on the same population, only the study with the most detailed data was included.
Two reviewers were trained and then independently screened studies and extracted the data. They crosschecked their information and any disagreements were resolved by an independent member of the research group who made the final decision.
The random effects model was used to summarise the prevalence of MIH with heterogeneity across studies assessed with I2 statistic. Meta-regression was conducted to explore potential sources of heterogeneity. The P-value was set at <0.05 and all statistical analysis was performed using Stata.
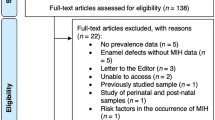
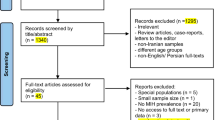
The authors communicated their selection process through a flow diagram showing 1401 citations initially selected from the database searches. Some1216 were excluded and after full-text analysis, a further 115 were excluded due to lack of prevalence figures for MIH, being case-control studies or containing a duplicate population. Their rationale for exclusions was well reasoned, ensuring pooled data was representative of global prevalence. In total, 70 articles remained for analysis that included a total of 89,520 people and 10,823 cases of MIH. The sample sizes of the chosen articles varied from 154 to 4989 participants.
The pooled global prevalence of MIH was 14.2% (95% CI: 12.6-15.8) however, there was significant heterogeneity between the studies. Meta-regression determined the sample size to have a statistically significant effect (P = 0.001) on the heterogeneity. South America was found to have the highest prevalence of MIH (18%, 95% CI: 13.8-22.2), followed by Oceania (16.3%, 95% CI: 12.6-20.0), Europe (14.3%, 95% CI: 12.2-16.3), Asia (13.0%, 95% CI: 10.5-15.5) and Africa (10.9%, 95% CI: 4.2-17.6). The authors stratified data based on continents allowing prevalence rates to be representative of the global burden of MIH for each region. Mean MIH prevalence, as a proxy of burden in each region, is unlikely to be representative of the entire continent however; this is the best the authors could achieve given the limited, good quality studies available.
The prevalence of MIH amongst children ten years of age or younger were higher (15.1%, 95% CI: 12.1-18.2) than children older than this age (12.1%, 95% CI: 8.0-16.3). This is likely due to several reasons such as MIH being clinically detected when the first permanent molars and incisors first erupt or affected teeth being extracted or restored prior to assessment. Furthermore, access to dental care in certain countries should be taken into consideration when interpreting the findings. There was no sex significance, which was to be expected, given the systemic aetiology of this condition.
Each study was evaluated using Egger's test and Begg's funnel plot to identify any publication bias. Then the trim and fill method was applied to assess bias by filling the funnel plot with the random effects model. The authors estimated nine studies to be missing from the selection, which (in addition to publication bias) may have implications in determining the overall prevalence of MIH. Identifying the potential aetiological factors of each study may further help us understand the complex nature of MIH. This study has informed the burden of MIH across each region; data which can be utilised by policymakers to assist in healthcare strategy.
Practice point
-
Children aged ten years or younger had a higher prevalence of MIH than those older. Additionally, there were no sex differences with prevalence.
-
The importance of active surveillance and appropriate management is emphasised through recognition of MIH as a global disease affecting young people in multiple countries, especially with a global prevalence of 14.2%.
References
Weerheijm KL . Molar incisor hypomineralisation (MIH). Eur J Paediatr Dent 2003; 4:114–120.
Mahoney E, Ismail FS, Kilpatrick N, Swain M . Mechanical properties across hypomineralized/hypoplastic enamel of first permanent molar teeth. Eur J Oral Sci 2004; 112:497–502.
Garg N, Jain AK, Saha S, Singh J . Essentiality of early diagnosis of molar incisor hypomineralization in children and review of its clinical presentation, Etiology and Management. Int J Clin Pediatr Dent 2012; 5:190–196.
Silva MJ, Scurrah KJ, Craig JM, Manton DJ, Kilpatrick N . Etiology of molar incisor hypomineralization - A systematic review. Community Dent Oral Epidemiol 2016; 44:342–353.
Teixeira RJPB, Andrade NS, Queiroz LCC, et al. Exploring the association between genetic and environmental factors and molar incisor hypomineralization: evidence from a twin study. Int J Paediatr Dent 2018; 28:198–206.
Lygidakis NA . Treatment modalities in children with teeth affected by molar-incisor enamel hypomineralisation (MIH): A systematic review. Eur Arch Paediatr Dent 2010; 11:65–74.
Schwendicke F, Elhennawy K, Reda S, Bekes K, Manton DJ, Krois J . Global burden of molar incisor hypomineralization. J Dent 2018; 68:10–18.
Author information
Authors and Affiliations
Additional information
Address for correspondence: Dr Ye-Huan Sun, Department of Epidemiology and Statistics, School of Public Health, Anhui Medical University, No. 81 Meishan Road, Hefei, Anuhui 230032, China. E-mail: yhsun_ahmu_edu@yeah.net
Zhao D, Dong B, Yu D, Ren Q, Sun Y. The prevalence of molar incisor hypomineralization: evidence from 70 studies. Int J Paediatr Dent 2018; 28: 170–179.
Rights and permissions
About this article
Cite this article
Dave, M., Taylor, G. Global prevalence of molar incisor hypomineralisation. Evid Based Dent 19, 78–79 (2018). https://doi.org/10.1038/sj.ebd.6401324
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ebd.6401324
This article is cited by
-
Prenatal exposure to environmental toxins and comprehensive dental findings in a population cohort of children
BMC Oral Health (2024)
-
Parental satisfaction and acceptance of silver diamine fluoride treatment for molar incisor hypomineralisation in pediatric dentistry: a cross-sectional study
Scientific Reports (2024)
-
Prevalence and clinical characteristics of molar-incisor hypomineralization in Syrian children: a cross-sectional study
Scientific Reports (2023)
-
Prevalence and severity of molar-incisor hypomineralization, is there an association with socioeconomic status? A cross-sectional study in Chilean schoolchildren
European Archives of Paediatric Dentistry (2023)
-
Er:YAG laser therapy in combination with GLUMA desensitizer reduces dentin hypersensitivity in children with molar-incisor hypomineralization: a randomized clinical trial
Lasers in Medical Science (2023)