Abstract
Data sources
Electronic Databases searched in PubMed, Embase and Scopus. Unpublished literature was traced through OpenSIGLE, annals of IADR/AADR (International and American Associations for Dental Research) and ORCA (European Organisation for Caries Research) from 2003-2014. Studies were limited to English.
Study selection
Studies involving visual inspection for detection of primary coronal caries lesions in primary or permanent human teeth were considered. All papers needed to include a clearly defined reference standard and the reporting of absolute numbers of true positives, false positives, true negatives and false negatives or a presentation of sufficient data to calculate these figures. Reference methods considered appropriate were histologic evaluation, operative intervention, direct visual inspection after temporary tooth separation and radiography. For studies with the same data set only the most complete study was included. Articles that reported caries detection using artificial caries, root caries or recurrent decay adjacent to restorations were excluded.
Data extraction and synthesis
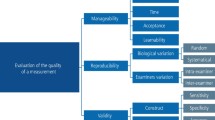
Study selection for inclusion was performed independently by two reviewers and disagreements were resolved by discussion with a third reviewer. Data were collected by two reviewers on structured tables. Discrepancies were resolved by consensus. A meta-analysis was performed. The following information was extracted; reference standard method, setting (clinical or laboratory), type of teeth (primary or permanent), surface evaluated (smooth, proximal or occlusal), sample size, examiner's experience. Also recorded were visual scoring systems. Studies that did not report any criteria were classified as 'with no criteria'. If authors used criteria with no reference to previously published studies they were classified as 'own criteria'. The PRISMA guideline was followed to report the review and the QUADAS-2 checklist (Quality assessment of studies of diagnostic performance included in systematic reviews) was used to assess the risk of bias of the included studies.
Results
Data were used to calculate the pooled sensitivity, specificity, diagnostic odds ratio and summary receiver operating characteristics curve. Heterogeneity of the studies was also assessed. A total of 102 manuscripts and one abstract were included. The analysis demonstrated that the visual method had good accuracy for detecting carious lesions. Clinically obtained specificity was higher. Also observed was moderate to high heterogeneity and evidence of publication bias. Studies employing well known visual scoring systems were significantly more accurate than those that used their own criteria. The results were grouped and differentiate the type of dentition (permanent or primary), type of lesion (initial or advanced), proximal or occlusal surface and clinical settings from laboratory settings.
The pooled specificity calculated was high in most of the groups and ranged from 0.573 to 0.992 mostly > 0.90; the lowest was in the occlusal initial caries lesions in primary teeth.
The sensitivity ranged from 0.274 to 0.77; the lowest from clinical studies in proximal surfaces in permanent teeth, the highest from three studies evaluating the occlusal initial caries lesions in permanent teeth. Most of the pooled sensitivities were around a low level.
Conclusions
Visual caries detection method has good overall performance. Although the studies together had high heterogeneity and risk of bias, the use of detailed and validated indices seems to improve the accuracy of the method.
Similar content being viewed by others
Commentary
In the implications for clinical practice the authors concluded (with all the caveats from the study) that visual inspection alone presented a good overall accuracy and high value for specificity and they recommend its utilisation in clinical practice. This recommendation is based on the calculated pooled specificity being high. As an example, the review for incipient carious lesions on permanent teeth calculates the pooled specificity as 0.990 (95% CI 0.995/0.994). In the case for incipient proximal carious lesions with a specificity of 99% the test will identify 99% of patients without the disease as test negative (true negatives) and 1% patients without the disease will incorrectly identified as test positive (false positive). Bear in mind that the information in this case is provided by three very heterogeneous clinical studies (I2 96.5%)
For initial carious lesions on the occlusal surface (results from seven studies with some heterogeneity I2: 67.8%) the pooled specificity is 0.573 (95% CI 0.519/0.626) and the pooled sensitivity 0.752 (95% CI 0.708-0.793). The difference here is a test with a 75% sensitivity will detect 75% of the patients with the disease (true positives) but 25% with the disease will go undetected (false negatives). In the case for incipient lesions as an example, with a specificity of 99% the test will identify 99% of patients without the disease as test negative (true negatives) and 1% of the patients without the disease will be incorrectly identified as test positive (false positive). A high sensitivity test is clearly important where the test is used to identify a serious but treatable disease. In the case of caries one would prefer false negatives rather than false positives. Surgical tooth intervention once begun is irrevocable. Tooth decay once initiated is slow to progress and can be visualised at a subsequent examination.
The pooled specificity for more advanced inter-proximal carious lesions in permanent teeth reported is 0.988 (95% CI 0.84-0.992) from four studies (with a test of heterogeneity I2 of 0%). Visual detection of more advanced carious lesions should be more facile and therefore have a high sensitivity.
Sensitivity and specificity are used to evaluate a clinical test. They are independent of the population of interest. For clinical practice, calculation of positive and negative predictive values are more useful, since they are dependent on the prevalence of the disease in the population of interest. For this reason the results should be interpreted with caution because the prevalence of the disease in the population and the specific patient should be taken in to account.
For the final recommendation about which visual index to use (most of them have DOR >1 good for a diagnostic tool) the authors recommended the utilisation of a well established scoring system since this has an impact in the overall accuracy of the method (one of the authors Ekstrand, has a visual scoring system ERK criteria). Other visual scoring systems reported were ICDAS, World Health Organization (WHO), Nyvad scoring system and Nytun.
These results should also be interpreted with prudence, for caries diagnosis the use of one tool alone for diagnosis of all mouths should not be encouraged; adjunct tools for caries detection should be included in clinical practice.
Caries detection is an essential skill for a dental practitioner. Daily, patient by patient, the dentist performs this search. A good clinician must possess this fundamental ability to be successful.
Dental practitioners when assessing each tooth for decay are using diagnostic skills where they are reviewing the entire mouth. Not one tooth in isolation is akin to these studies. A patient with a low incidence of decay and therefore limited restorations is viewed through a different lens from one with poor oral hygiene and multiple restorations.
A limitation of this review is the inclusion of proximal caries detection. Infrequently proximal decay can be visualised as a dark area seen through the tooth but radiographic confirmation is necessary for proper diagnosis. Visual detection alone does not rule out proximal decay.
In conclusion, a thorough review of all studies evaluating the accuracy of visual methods for detecting decay was performed but for what practical purpose? After this exhaustive systematic review and meta-analysis will dentists be certain that the next tooth they diagnose as positive for caries will have decay and need treatment? I think not. It may be statistically relevant from many combined studies that caries can be detected accurately by visual methods, however it is doubtful that this result is clinically relevant.
Author information
Authors and Affiliations
Additional information
Address for correspondence: FM Mendes, Faculdade de Odontologia da Universidade de São Paulo, Av Lineu Prestes, 2227, São Paulo, 05508-000, SP, Brazil. Email fmmendes@usp.br
Gimenez T, Piovesan C, Braga MM, Raggio DP, Deery C, Ricketts DN, Ekstrand DR, Mendes FM. Visual Inspection for Caries Detection: A Systematic Review and Meta-analysis. J Dent Res 2015; 94: 895–904.
Rights and permissions
About this article
Cite this article
Hoskin, E., Keenan, A. Can we trust visual methods alone for detecting caries in teeth?. Evid Based Dent 17, 41–42 (2016). https://doi.org/10.1038/sj.ebd.6401165
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ebd.6401165
This article is cited by
-
Comparing the outcomes of gold-standard dental examinations with photographic screening by mid-level dental providers
Clinical Oral Investigations (2019)