Key Points
In brief
-
Acupuncture is not a miracle cure and is not going to replace the drill. However, the technique can be a supplement to conventional treatments in TMDs, facial pain, pain management Sjøegrens syndrome, and in phobias and anxiety.
-
Acupuncture does have a scientific background and the efficacy has been tested in a number of clinical trials including pain management, facial pain, TMD and increasing of the pain threshold.
-
Acupuncture is not without adverse effect and therefore proper training is essential.
-
The technique can be achieved by any dentist after a short training programme
Abstract
An introduction to the practical application of acupuncture in dentistry is presented in the light of current research. It is concluded that acupuncture could supplement conventional treatment modalities. Its value in the treatment of temporomandibular dysfunction syndrome and facial pain has been well documented and supported by randomised controlled trials. Although it may be useful in the control of post-operative pain, its use as sole analgesia for operative care is questionable. The mode of action of acupuncture can be explained with reference to modern neurophysiology. A short training course can allow the technique to be an effective tool in every dentist's hands.
Similar content being viewed by others
Main
Acupuncture originated in China more than 3,000 years ago and involves insertion of needles into various parts of the body with the intention of curing disease. Two recent papers have reviewed the use of acupuncture in dentistry.1,2 Both authors have concluded that it is effective in a number of conditions encountered in dental practice such as temporomandibular dysfunction syndrome (TMD) and pain management. In addition Blom et al. have demonstrated its value in Sjøgrens disease.3Despite its long history there still exists a great deal of scepticism in the professional community as to its efficacy. This is understandable as the scientific study of acupuncture has occurred only relatively recently. A commonly held view of acupuncture is that it is a complicated technique involving a substantial knowledge of ancient Chinese philosophy whose action is largely a placebo effect and in any case of limited application to dentistry. However, Richardson has shown it to be effective in a wide range of musculo-skeletal conditions,4 Lundeberg has demonstrated that it may improve the immune response,5 and Tao recommends its use in stress management,6 a topic that interfaces with dental practice. The aim of this paper is to give a broad introduction to acupuncture to the general dental practitioner and to emphasise the scientific background for acupuncture. Before doing so it is necessary to briefly review some of the scientific evidence in support of acupuncture.
The author would like to thank Dr James Clague-Moore (UK) for constructive comments to the paper.
Research on acupuncture
A recent systematic review2 of published literature was able to identify 74 publications concerning the use of acupuncture in dentistry of which 17 reported randomised controlled trials (RCT).8,9,10,11,12,13,14,15,16,17,18,19,20,21,22 As three of these covered the same study14,15,16 they were regarded for the purpose of analysis as one trial resulting in a total of 15 RCTs. These were scored according to predefined and accepted criteria7 to assess the methodological quality. A score of methodological quality 60%+ (ie trial design incorporating some defects, but these unlikely to seriously influence outcome) was used as an acceptable criterion. Nine of the trials achieved this level: of these, four investigated TMD and four the use of acupuncture in post-operative pain management. All four trials covering TMD9,12,13,14,15,16 showed some benefit comparable to occlusal splint therapy. Three of the trials on post-operative pain management found acupuncture effective.10,11,17
The other recent review analysed 16 trials of the analgesic effect of acupuncture and found that the majority of the studies showed some positive effect,1 although the experimental nature of some of the studies made the evaluation of practical use difficult. However, in summary it may be stated that where trials are competently constructed and executed there is a body of scientific evidence supporting the efficacy of acupuncture within dental practice.
How does it work?
Acupuncture activates small myelinated nerve fibres in muscle, which send impulses to the spinal cord and then activate the midbrain and pituitary-hypothalamus. It has been shown that enkephalin, beta-endorphin, dynorphin, serotonin and noradrenalin are involved in this process.23 It is well known that a painful stimulation will activate two types of nerve fibres in the peripheral nervous system: A-δ-fibres and C-fibres which primarily will terminate at the second layer of the back horn. From the second layer of the back horn, the pain sensation is via interneurons transmitted to the cortex and we will experience a pain.24
Today it is generally accepted that insertion of a needle in an acupuncture point will create a small inflammatory process with release neurotransmitters such as bradykinin, histamine, etc. and subsequent stimulate A-δ-fibres located in the skin and muscle.25 The A-δ-fibres terminate in the second layer of the back horn and inhibits the incoming painful sensations by release of enkephaline.24 This segmental model is the most simple mode of action and accounts probably for the pain relieving effect of acupuncture in most cases.25
From the second layer of the back horn, the A-δ-fibre continues to the fifth layer of the back horn, cross over to the opposite side and ascend via the spinothalamic tract to the mid brain where the raphe magnus nucleus is stimulated.26 Raphe magnus nucleus is the main producer of serotonin on the brain and is believed to play a key role in acupuncture's mode of action.27 Thus, it has been demonstrated that serotonin is a pro-drug for endorphin which probably accounts for the central (extrasegmental) effect of acupuncture. Moreover, it has been shown that serotonin is a pro-drug for ACTH, which probably via the pituitary gland accounts for the increase of cortisol which has been shown after acupuncture23 and thus improves the immune system. Finally, Serotonin has a direct effect on the cortex and it is likely that the beneficial effect of acupuncture on stress and anxiety is because of this direct effect.27
It has been suggested that the pituitary gland takes part in the production of endorphin but our knowledge at this level is very scanty.23
The implementation of acupuncture in dentistry
Acupuncture came to Western Europe as a part of an alternative system of medicine. Traditional Chinese medicine (TCM), over the past 25 years, through neurophysiological research and well conducted clinical trials, has gained acceptance as a valuable tool in the general management of pain. However, it should be stated that acupuncture should be considered as an extra tool in the toolbox only. Its introduction into general dental practice has potentially three paths:
-
As a variant of the old medical acronym TEETH (tried everything else, try homeopathy). That is when clinicians have exhausted all available therapeutic avenues, acupuncture is tried as a last resort. This is unfair both to the patient, in whom it may engender false hopes of a 'miracle', and the practitioner for whom repeated failure may lead to abandonment of further study.
-
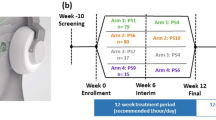
As a supplement to orthodox treatment where treatment modalities may be limited or ineffective. Clear examples are to suppress the gagging reflex during maxillary impression taking, the reduction in postoperative analgesic requirement in patients sensitive to them, reduction of time in the onset of local anaesthesia and control of pre-operative anxiety (Fig. 1). These involve simple acupuncture treatments with the insertion of few needles at recognised acupuncture points, which can be taught to any dentist as a short postgraduate course.
-
As an adjunct to, or replacement of normal treatment modalities, for more complex conditions such as TMD or facial pain (Fig. 2). Suitable example are when the use of non steroid anti-inflammatory drugs (NSAID's) is contra-indicated because of concomitant systemic medication or gastric ulceration. These therapies require careful evaluation and a high level of expertise on the part of the practitioner, but postgraduate pathways do exist for this training within the UK.
In Table 1 a brief summary of a number of studies and their outcome is presented, which hopefully will give the reader confidence of the techniques efficacy.
The practicalities of acupuncture
Does acupuncture always work?
No, and neither does anything else! It is not a miracle cure and in general if a significant improvement has not occurred after three sessions it is not worth continuing. There are two reasons for this: (i) some patients fail to respond to acupuncture per se,28 (ii) the original diagnosis could be wrong. A lack of response should always result in re-examination and refinement of the diagnosis.
How many treatments are needed?
One large-scale study found that the average number of treatments required to control the disorders of a mixed group of 350 patients was five,29 although clearly it is unrealistic to expect to gain control of chronic conditions with only a couple of treatments; indeed control of orofacial conditions such as trigeminal neuralgia may require several cycles of treatments.23
How soon can one expect a result?
It is not uncommon for patients to report some benefit immediately, especially in acute headache and torticollis. This will probably only last for a day or so, the period of relief extending with each successive treatment until control is achieved.
Can there be adverse effects associated with acupuncture?
Contrary to the popular belief that conventional medicine is beset by untoward sequelae and that 'alternative' techniques are totally safe; there have been numerous reports of adverse effects after acupuncture. These are (to mention a few) pneumothorax, endocarditis and hepatitis some resulting in fatalities.30 However, it must be appreciated that most of these result from ignorance of basic anatomy or because of non applying aseptic procedures by non medical/dental qualified practitioners. When these are factored out of analysis, acupuncture proves to be a very safe technique in the hands of a properly trained practitioner.
How can one get the necessary education in acupuncture?
The education in acupuncture is arranged by the British Medical Acupuncture Society (BMAS) and the British Dental Acupuncture Society (BDAS) leading to a diploma of basic competence. To qualify for this diploma the participants should attend a basic course, a post-basic course and a practical course of a total of 40 hours duration. The basic course teaches the basic principles such as point location, practical needling, the neurophysiological background, planning treatment etc. The post-basic course puts the acquired skills into dental-related diseases such as TMD, Sjøegrens disease, pain management, facial pains, etc. Finally, the participants take part in a 1-day practical course where the technique and the practical application is demonstrated on patients. Participants will, after the basic course, be able to start using the technique on a selected number of conditions but to use the technique on a wider range of diseases an education equivalent to the diploma of basic competence is required. For those who want to go further, intermediate and advanced courses are available as well as a yearly scientific meeting.
Conclusion
In general acupuncture should be regarded as a supplement to conventional treatment. As a sole analgesic for operative intervention its value is questionable; however, in control of post-operative pain and in the management of TMD and facial pain it may be a valuable addition to the therapeutic armamentarium of the general dental practitioner. These skills may be acquired with a short postgraduate training programme.
References
Ernst E, Pittler M H. The effectiveness of acupuncture in treating acute dental pain: a systemic review. Br Dent J 1998; 184: 443–472.
Rosted P. The use of acupuncture in dentistry: a review of the scientific validity of published papers. Oral Dis 1998; 4: 100–104.
Blom M, Dawidson I, Angmar-Månsson B. The effect of acupuncture on salivary flow rates in patients with xerostomia. Oral Surg, Oral Med, Oral Pathol 1992; 73: 293–298.
Richardson P H, Vincent C A. Acupuncture for the treatment of pain: a review of evaluative research. Pain 1986; 24: 15–40.
Lundeberg T. Peripheral effects of sensory nerve stimulation (acupuncture) in inflammation and ischemia. Scand J Rehab Med Suppl. 1993; 29: 61–86.
Tao D J. Research on the reduction of anxiety and depression with acupuncture. Am J Acup 1993; 21: 327–329.
Vickers A. Ensuring scientific rigor in literature review. Acup Med 1995; 13: 93–96.
Ekblom A, Hansson P, Thomsson M, Thomas M. Increased postoperative pain and consumption of analgesics following acupuncture. Pain 1991; 44: 241–247.
Johanssson A, Wenneberg B, Wagersten C, Haraldson T. Acupuncture in treatment of facial muscular pain. Acta Odontol Scand 1991; 49: 153–158.
Lao L, Bergman S, Anderson R, Langenberg P, Wong R H, Berman B. The effect of acupuncture on post-operative oral surgery pain; A pilot study. Acup Med 1994; 12: 13–17.
Lao L, Bergman S, Lamgenberg P, Wong R H, Berman B. Efficacy of Chinese acupuncture on ostoperative oral surgery pain. Oral Surg, Oral Med, Oral Pathol 1995; 79: 423–428.
List T, Helkimo M, Andersson S, Carlsson G E. Acupuncture and occlusal splint therapy in the treatment of craniomandibular disorders. Swed Dent J 1992; 16: 125–41.
List T, Helkimo M. Acupuncture and occlusal splint therapy in the treatment of cranio-mandibular disorders. A 1 year follow-up study. Acta Odontol Scand 1992; 50: 375–385.
Raustia A M, Pohjola R T, Virtanen K K. Acupuncture compared with stomatognathic treatment for TMJ dysfunction. Part I: A randomized study. J Prosthet Dent 1985; 54: 581–585.
Raustia A M, Pohjola R T, Virtanen K K. Acupuncture compared with stomatognathic treatment for TMJ dysfunction. Part II: Components of the dysfunction index. J Prosthet Dent 1986; 55: 372–376.
Raustia A M, Pohjola R T. Acupuncture compared with stomatognathic treatment for TMJ dysfunction. Part III: Effect of treatment on mobility. J Prosthet Dent 1986; 56: 616–623.
Sung Y F, Kuntner M H, Cerine F C . and Frederickson E L . Comparison of the effects of acupuncture and codeine on postoperative dental pain. Anesthesia and Analgesia 1977; 56: 473–478.
Taub H A, Mitchell J N, Stuber F E, Eisenberg L, Beard M C, McCormack R K. Analgesia for operative dentistry: A comparison of acupuncture and placebo. Oral Surg, Oral Med, Oral Pathol 1979; 48: 205–210.
Baraschkow G N, Stosch W I. Die Akupunktur als mittel der Schmarzbekämpfung bei Zahnextraktionen.(In German. Akupunkture. 1991; 19: 207–209.
Hansson P, Ekblom A, Thomsson M and Lundeberg T . Is acupuncture sufficient as the sole analgesic in oral surgery. Oral Surg, Oral Med, Oral Pathol 1987; 64: 283–286.
Lapeer G L, Biedermann H J, Hemsted J J. Acupuncture analgesia for postoperative dental pain. J Can Dent Assoc 1987; 6: 479–480.
Lee M H M, Teng P, Zaretsky H H, Rubin M. Acupuncture anesthesia in dentistry. State Dental J 1973; 39: New York 299–301.
Stux G, Pomeranz B . Acupuncture Textbook and Atlas. Berlin: Springer-Verlag, 1987: 1–34.
Bowsher D. Physiology and pathophysiology of pain. Acupunct Med 1990; VII: 17–20.
Macdonald A. Acupuncture analgesia and therapy – Part 2. Acupunct Med 1990; VIII: 44–49.
Bowsher D. The physiology of stimulation-produced analgesia. Acupunct Med 1991; 9: 58–61.
Veroux G . Percivalle V . Fundamentals and scientific research in acupuncture. Acupunct Med 1988; V: 12–14.
Mann F. Textbook of acupuncture. London: William Heinemann Medical Books, 1987.
Rosted P. Anvendelse af akupunktur i daglig klinik: en multicenterundersøgelse. Lægerne i Ribe Amt 1996; 16: 9–12.
Rosted P. Adverse reaction after acupuncture: A review. Critical Rev Phys Rehabil Med 1997; 9: 245–264.
Andersson S A, Ericson T, Holmgren E, Lindquist G. Electro-acupuncture. Effect on pain threshold measured with electrical stimulation of teeth. Brain Res 1973; 63: 393–396.
Andersson S A, Holmgren E, Roos A. Analgesic effects of peripheral conditioning stimulation-II. Importance of certain stimulation parameters. Acupunc Electrother Res 1977; 2: 237–246.
Bakke M. Effect of acupuncture on the pain perception thresholds of human teeth. Scand J Dent Res 1976; 84: 404–408.
Chapman C R, Gehrig J D, Wilson M E. Acupuncture compared with 33 per cent nitrous oxide for dental analgesia. Anesthesiol 1975; 42: 532–537.
Chapman C R, Wilson M E, Gehrig J D. Comparative effects of acupuncture and Transcutaneous Stimulation on the perception of painful dental stimuli. Pain 1976; 2: 265–283.
Chapman C R, Chen A C, Bonica J J. Effects of intrasegmental electrical acupuncture on dental pain: Evaluation by threshold estimation and sensory decision theory. Pain 1977; 3: 213–227.
List T, Helkimo M. Acupuncture in the treatment of patients with chronic facial pain and mandibular dysfunction. Swed Dent J 1987; 11: 83–92.
Sung Y F, Kuntner M H, Cerine F C, Frederiskson E L. Comparison of the effects of acupuncture and codeine on postoperative dental pain. Anesth Analgesic 1977; 56: 473–478.
Wong T. Use of electrostimulation of acupuncture points in general dental practice. Anesth Prog 1989; 36: 243–244.
Author information
Authors and Affiliations
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Rosted, P., Rosted, P. Introduction to acupuncture in dentistry. Br Dent J 189, 136–140 (2000). https://doi.org/10.1038/sj.bdj.4800704
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4800704
This article is cited by
-
Complementary treatments and dental indemnity
BDJ In Practice (2020)
-
A survey on the uses of acupuncture by a group of UK dentists
British Dental Journal (2005)
-
The role of acupuncture in controlling the gagging reflex using a review of ten cases
British Dental Journal (2001)