Abstract
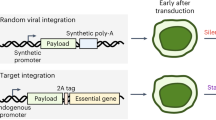
Confinement of transgene expression to target cells is highly desirable in gene therapy. Current strategies of transcriptional targeting to tumors usually rely on tissue-specific promoters to control gene expression. However, such promoters generally have much lower activity than the constitutive viral promoters. We have explored an alternative approach, using a strict-late viral promoter (UL38p) in the context of an oncolytic herpes simplex virus (HSV) for tumor-selective gene expression. As with many DNA viruses, the genomic transcription of HSV is a tightly regulated molecular cascade in which early and late phases of gene expression are separated by viral DNA replication. In particular, some of the late transcripts are categorized as strict-late, whose expression depends rigorously on the initiation of viral DNA replication. Our in vitro and in vivo characterization showed that in normal nondividing cells, where the oncolytic HSV has limited ability to replicate, the UL38p has minimal activity. However, in tumor or cycling cells where the virus can fully replicate, transgene expression from UL38p was almost as high as from the cytomegalovirus immediate-early promoter. These results suggest that delivery of therapeutic genes driven by UL38p through an oncolytic HSV may be an effective approach to gene therapy for malignant diseases.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Huber BE, Richards CA, Krenitsky TA . Retroviral-mediated gene therapy for the treatment of hepatocellular carcinoma: an innovative approach for cancer therapy. Proc Natl Acad Sci USA 1991; 88: 8039–8043.
Vile RG, Hart IR . Use of tissue-specific expression of the herpes simplex virus thymidine kinase gene to inhibit growth of established murine melanomas following direct intratumoral injection of DNA. Cancer Res 1993; 53: 3860–3864.
Latham JP, Searle PF, Mautner V, James ND . Prostate-specific antigen promoter/enhancer driven gene therapy for prostate cancer: construction and testing of a tissue-specific adenovirus vector. Cancer Res 2000; 60: 334–341.
Tanaka S et al. Targeted killing of carcinoembryonic antigen (CEA)-producing cholangiocarcinoma cells by polyamidoamine dendrimer-mediated transfer of an Epstein–Barr virus (EBV)-based plasmid vector carrying the CEA promoter. Cancer Gene Ther 2000; 7: 1241–1250.
Schuur ER et al. Prostate-specific antigen expression is regulated by an upstream enhancer. J Biol Chem 1996; 271: 7043–7051.
Koga S et al. A novel telomerase-specific gene therapy: gene transfer of caspase-8 utilizing the human telomerase catalytic subunit gene promoter. Hum Gene Ther 2000; 11: 1397–1406.
Babiss LE, Friedman JM, Darnell JE . Cellular promoters incorporated into the adenovirus genome. Effect of viral DNA replication on endogenous and exogenous gene transcription. J Mol Biol 1987; 193: 643–650.
Bischoff JR et al. An adenovirus mutant that replicates selectively in p53-deficient human tumor cells [see comments]. Science 1996; 274: 373–376.
Martuza RL et al. Experimental therapy of human glioma by means of a genetically engineered virus mutant. Science 1991; 252: 854–856.
Mineta T et al. Attenuated multi-mutated herpes simplex virus-1 for the treatment of malignant gliomas. Nat Med 1995; 1: 938–943.
Wagner EK, Guzowski JF, Singh J . Transcription of the herpes simplex virus genome during productive and latent infection. Prog Nucleic Acid Res Mol Biol 1995; 51: 123–165.
Holland LE, Anderson KP, Shipman Jr C, Wagner EK . Viral DNA synthesis is required for the efficient expression of specific herpes simplex virus type 1 mRNA species. Virology 1980; 101: 10–24.
Flanagan WM et al. Analysis of the herpes simplex virus type 1 promoter controlling the expression of UL38, a true late gene involved in capsid assembly. J Virol 1991; 65: 769–786.
Johnson PA, Everett RD . DNA replication is required for abundant expression of a plasmid-borne late US11 gene of herpes simplex virus type 1. Nucleic Acids Res 1986; 14: 3609–3625.
Guzowski JF, Wagner EK . Mutational analysis of the herpes simplex virus type 1 strict late UL38 promoter/leader reveals two regions critical in transcriptional regulation. J Virol 1993; 67: 5098–5108.
Guzowski JF, Singh J, Wagner EK . Transcriptional activation of the herpes simplex virus type 1 UL38 promoter con-ferred by the cis-acting downstream activation sequence is mediated by a cellular transcription factor. J Virol 1994; 68: 7774–7789.
Goodart SA, Guzowski JF, Rice MK, Wagner EK . Effect of genomic location on expression of beta-galactosidase mRNA controlled by the herpes simplex virus type 1 UL38 promoter. J Virol 1992; 66: 2973–2981.
Saeki Y et al. Herpes simplex virus type 1 DNA amplified as bacterial artificial chromosome in Escherichia coli: rescue of replication-competent virus progeny and packaging of amplicon vectors. Hum Gene Ther 1998; 9: 2787–2794.
Herrlinger U et al. HSV-1 infected cell proteins influence tetracycline-regulated transgene expression. J Gene Med 2000; 2: 379–389.
Schang LM, Phillips J, Schaffer PA . Requirement for cellular cyclin-dependent kinases in herpes simplex virus replication and transcription. J Virol 1998; 72: 5626–5637.
Rampling R et al. Toxicity evaluation of replication-competent herpes simplex virus (ICP 34.5 null mutant 1716) in patients with recurrent malignant glioma. Gene Therapy 2000; 7: 859–866.
Markert JM et al. Conditionally replicating herpes simplex virus mutant, G207 for the treatment of malignant glioma: results of a phase I trial. Gene Therapy 2000; 7: 867–874.
MacKie RM, Stewart B, Brown SM . Intralesional injection of herpes simplex virus 1716 in metastatic melanoma. Lancet 2001; 357: 525–526.
Fu X, Zhang X . Potent systemic antitumor activity from an oncolytic herpes simplex virus of syncytial phenotype. Cancer Res 2002; 62: 2306–2312.
Todryk S et al. Disabled infectious single-cycle herpes simplex virus as an oncolytic vector for immunotherapy of colorectal cancer. Hum Gene Ther 1999; 10: 2757–2768.
Bennett JJ et al. Antitumor efficacy of regional oncolytic viral therapy for peritoneally disseminated cancer. J Mol Med 2000; 78: 166–174.
Schellingerhout D et al. Mapping the in vivo distribution of herpes simplex virions. Hum Gene Ther 1998; 9: 1543–1549.
Wood M et al. Biodistribution of an adenoviral vector carrying the luciferase reporter gene following intravesical or intravenous administration to a mouse. Cancer Gene Ther 1999; 6: 367–372.
Huard J, Goins WF, Glorioso JC . Herpes simplex virus type 1 vector mediated gene transfer to muscle. Gene Therapy 1995; 2: 385–392.
Huard J et al. The basal lamina is a physical barrier to herpes simplex virus-mediated gene delivery to mature muscle fibers. J Virol 1996; 70: 8117–8123.
Shenk T . Adenoviridae: the viruses and their replication. In: Fields BN, Knipe DM, Howley PM (eds). Fields Virology. Lippincott Williams & Wilkins: Philadelphia, 1996, pp. 2111–2148.
Hawkins LK, Hermiston T . Gene delivery from the E3 region of replicating human adenovirus: evaluation of the E3B region. Gene Therapy 2001; 8: 1142–1148.
Acknowledgements
We thank Yoshinaga Saeki (Massachusetts General Hospital) for the generous gift of fHSV-delta-pac and Malcolm K Brenner for support and careful reading of the manuscript.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Fu, X., Meng, F., Tao, L. et al. A strict-late viral promoter is a strong tumor-specific promoter in the context of an oncolytic herpes simplex virus. Gene Ther 10, 1458–1464 (2003). https://doi.org/10.1038/sj.gt.3302029
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.gt.3302029
Keywords
This article is cited by
-
Virotherapy targeting cyclin E overexpression in tumors with adenovirus-enhanced cancer-selective promoter
Journal of Molecular Medicine (2015)
-
Packaging, Amplification, and Appraisal of the Recombinant Tumor-Selective Type I Herpes Simplex Virus Carrying GALV.fus Gene
Cell Biochemistry and Biophysics (2014)
-
Anti-tumor Effects of Gene Therapy with GALV Membrane Fusion Glycoprotein in Lung Adenocarcinoma
Cell Biochemistry and Biophysics (2014)
-
Combination of autophagy inducer rapamycin and oncolytic adenovirus improves antitumor effect in cancer cells
Virology Journal (2013)
-
Incorporation of the B18R Gene of Vaccinia Virus Into an Oncolytic Herpes Simplex Virus Improves Antitumor Activity
Molecular Therapy (2012)