Abstract
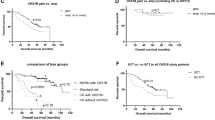
Ploidy appears as an important parameter in both the biology and the clinical evolution of multiple myeloma. However, its evaluation requires either a successful karyotyping (obtained in 30% of the patients) or a DNA index calculation by flow cytometry (not routinely performed in myeloma). We validated a novel method based on interphase fluorescence in situ hybridization that can be utilitized to analyze almost all the patients. The method was very specific and sensitive for the detection of hyperdiploidy. Extended studies showed that most recurrent 14q32 translocations occur in nonhyperdiploid clones, and that deletions of chromosome 13 were less frequently observed in hyperdiploid clones (48 vs 66%). Further large studies are ongoing to evaluate the prognostic value of ploidy in myeloma.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Dewald GW, Kyle RA, Hicks GA, Greipp PR . The clinical significance of cytogenetic studies in 100 patients with multiple myeloma, plasma cell leukemia, or amyloidosis. Blood 1985; 66: 380–390.
Gould J, Alexanian R, Goodacre A, Pathak S, Hecht B, Barlogie B . Plasma cell karyotype in multiple myeloma. Blood 1988; 71: 453–456.
Tricot G, Barlogie B, Jagannath S, Bracy D, Mattox S, Vesole DH et al. Poor prognosis in multiple myeloma is associated only with partial or complete deletion of chromosome 13 or abnormalities involving 11q and not with other karyotype abnormalities. Blood 1995; 86: 4250–4256.
Laï JL, Zandecki M, Mary JY, Bernardi F, Izydorczyk V, Flactif M et al. Improved cytogenetics in multiple myeloma: a study of 151 patients including 117 patients at diagnosis. Blood 1995; 85: 2490–2497.
Sawyer JR, Waldron JA, Jagannath S, Barlogie B . Cytogenetic finding in 200 patients with multiple myeloma. Cancer Genet Cytogenet 1995; 82: 41–49.
Fonseca R, Coignet LJA, Dewald GW . Cytogenetic abnormalities in multiple myeloma. Hematol/Oncol Clin N Am 1999; 13: 1169–1180.
Smadja NV, Bastard C, Brigaudeau C, Leroux D, Fruchart C . Hypodiploidy is a major prognostic factor in multiple myeloma. Blood 2001; 98: 2229–2238.
Calasanz MJ, Cigudosa JC, Odero MD, Garcia-Foncillas J, Marin J, Ardanaz MT et al. Hypodiploidy and 22q11 rearrangements at diagnosis are associated with poor prognosis in patients with multiple myeloma. Br J Haematol 1997; 98: 418–425.
Fassas ABT, Spencer T, Sawyer J, Zangari M, Lee CL, Anaissie E et al. Both hypodiploidy and deletion of chromosome 13 independently confer poor prognosis in multiple myeloma. Br J Haematol 2002; 118: 1041–1047.
Debes-Marun CS, Dewald GW, Bryant S, Picken E, Santana-Davila R, Gonzalez-Paz N et al. Chromosome abnormalities clustering and its implications for pathogenesis and prognosis in myeloma. Leukemia 2003; 17: 427–436.
Latreille J, Barlogie B, Dosik G, Johnston DA, Drewinko B, Alexanian R . Cellular DNA content as a marker of human multiple myeloma. Blood 1980; 55: 403–408.
Barlogie B, Alexanian R, Dixon D, Smith L, Smallwood L, Delasalle K . Prognostic implications of tumor cell DNA and RNA content in multiple myeloma. Blood 1985; 66: 338–341.
Tienhaara A, Pelliniemi TT . Flow cytometric DNA analysis and clinical correlations in multiple myeloma. Am J Clin Pathol 1992; 97: 322–330.
Smadja NV, Louvet C, Isnard F, Dutel JL, Grange MJ, Varette C et al. Cytogenetic study in multiple myeloma at diagnosis: comparison of two techniques. Br J Haematol 1995; 90: 619–624.
Brigaudeau C, Trimoreau F, Gachard N, Rouzier E, Jaccard A, Bordessoule D et al. Cytogenetic study of 30 patients with multiple myeloma: comparison of 3 and 6 day bone marrow cultures stimulated or not with cytokines by using a miniaturized karyotypic method. Br J Haematol 1997; 96: 594–600.
Hernandez JM, Gutierrez NC, Almeida J, Garcia JL, Sanchez MA, Mateo G et al. IL-4 improves the detection of cytogenetic abnormalities in multiple myeloma and increases the proportion of clonally abnormal metaphases. Br J Haematol 1998; 103: 163–167.
Seong C, Delasalle K, Hayes K, Weber D, Dimopoulos D, Swantkowski J et al. Prognostic value of cytogenetics in multiple myeloma. Br J Haematol 1998; 101: 189–194.
Smadja NV, Fruchart C, Isnard F, Louvet C, Dutel JL, Cheron N et al. Chromosomal analysis in multiple myeloma: cytogenetic evidence of two different diseases. Leukemia 1998; 12: 960–969.
Rajkumar SV, Fonseca R, Dewald GW, Therneau TM, Lacy MQ, Kyle RA et al. Cytogenetic abnormalities correlate with the plasma cell labelling index and extent of bone marrow involvement in myeloma. Cancer Genet Cytogenet 1999; 113: 73–77.
Shankey TV, Rabinovitch PS, Bagwell B, Bauer KD, Duque RE, Hedley DW et al. Guidelines for implementation of clinical DNA cytometry. Cytometry 1993; 14: 472–477.
Avet-Loiseau H, Li JY, Facon T, Brigaudeau C, Morineau N, Maloisel F et al. High incidence of translocations t(11;14)(q13;q32) and t(4;14)(p16;q32) in patients with plasma cell malignancies. Cancer Res 1998; 58: 5640–5645.
Avet-Loiseau H, Facon T, Grosbois B, Magrangeas F, Rapp MJ, Harousseau JL, for the Intergroupe Francophone du Myelome et al. Oncogenesis of multiple myeloma: 14q32 and 13q chromosomal abnormalities are not randomly distributed, but correlate with natural history, immunological features and clinical presentation. Blood 2002; 99: 2185–2191.
Fonseca R, Blood EA, Oken MM, Kyle RA, Dewald GW, Bailey RJ et al. Myeloma and the t(11;14)(q13;q32); evidence for a biologically defined unique subset of patients. Blood 2002; 99: 3735–3741.
Fonseca R, Debes-Marun CS, Picken EB, Dewald GW, Bryant SC, Winkler JM et al. The recurrent IgH translocations are highly associated with nonhyperdiploid variant multiple myeloma. Blood 2003; 102: 2562–2567.
Acknowledgements
This study has been supported by a grant from the Ligue contre le Cancer, and by a Programme Hospitalier de Recherche Clinique.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Wuilleme, S., Robillard, N., Lodé, L. et al. Ploidy, as detected by fluorescence in situ hybridization, defines different subgroups in multiple myeloma. Leukemia 19, 275–278 (2005). https://doi.org/10.1038/sj.leu.2403586
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.leu.2403586
Keywords
This article is cited by
-
Differences in the cytogenetic underpinnings of AL amyloidosis among African Americans and Caucasian Americans
Blood Cancer Journal (2022)
-
Genetic pathogenesis of immunoglobulin light chain amyloidosis: basic characteristics and clinical applications
Experimental Hematology & Oncology (2021)
-
European recommendations and quality assurance for cytogenomic analysis of haematological neoplasms
Leukemia (2019)
-
Cereblon-binding proteins expression levels correlate with hyperdiploidy in newly diagnosed multiple myeloma patients
Blood Cancer Journal (2019)
-
Cytogenetic abnormalities in monoclonal gammopathy of undetermined significance
Leukemia (2018)