Abstract
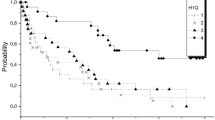
Immunophenotyping is a major tool to assign acute leukemia blast cells to the myeloid lineage. However, because of the large heterogeneity of myeloid-related lineages, no clinically relevant immunological classification of acute myeloblastic leukemia (AML) has been devised so far. To attempt at formulating such a classification, we analyzed the pattern of expression of selected antigens, on blast cells collected at AML diagnosis. Patients were eligible if they had a first diagnosis of de novo AML and a sufficient number of blast cells for proper immunophenotyping. The relative expression of CD7, CD13, CD14, CD15, CD33, CD34, CD35, CD36, CD65, CD117, and HLA-DR were analyzed by cytometry in a test series of 176 consecutive AML cases. Statistical tools of clusterization allowed to remove antigens with overlapping distribution, leading us to propose an AML classification that was validated in a second AML cohort of 733 patients. We identified five AML subsets (MA to ME) based on the expression of seven antigens within four groups (CD13/CD33/CD117, CD7, CD35/CD36, CD15).-MA and MB-AML have exclusively myeloid features with seldom extramedullary disease and rare expression of lymphoid antigens. No cases of acute promyelocytic leukemia (APL) were observed within MB AML. MC AML have either myeloid or erythroblastic features. MD AML have more frequently high WBC counts than other subsets, which were related to the expression of CD35/CD36 and CD14 and to monoblastic differentiation. ME AML lack CD13, CD33, and CD117 but display signs of terminal myeloid differentiation. Specific independent prognostic factors were related to poor overall survival in each immunological subset: CD34+ (P<3 × 10−4) in MA AML, CD7+ in MB AML, non-APL cases (P<0.03) in MC AML, CD34+ (P<0.002) and CD14+ (P<0.03) in MD AML, CD14+ in ME AML (P<0.01). The inclusion of seven key markers in the immunophenotyping of AML allows a stratification into clinically relevant subsets with individual prognostic factors, which should be considered to define high-risk AML populations.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout








Similar content being viewed by others
References
Bene MC, Castoldi G, Knapp W, Ludwig WD, Matutes E, Orfao A et al. Proposals for the immunological classification of acute leukemias. European Group for the Immunological Characterization of Leukemias (EGIL). Leukemia 1995; 9: 1783–1786.
Bene MC, Bernier M, Casasnovas RO, Castoldi G, Doekharan D, van der Holt B et al. Acute myeloid leukaemia M0: haematological, immunophenotypic and cytogenetic characteristics and their prognostic significance: an analysis in 241 patients. Br J Haematol 2001; 113: 737–745.
Matutes E, Morilla R, Farahat N, Carbonell F, Swansbury J, Dyer M et al. Definition of acute biphenotypic leukemia. Haematologica 1997; 82: 64–66.
Garand R, Vannier JP, Bene MC, Faure G, Favre M, Bernard A . Comparison of outcome, clinical, laboratory, and immunological features in 164 children and adults with T-ALL. The Groupe d'Etude Immunologique des Leucemies. Leukemia 1990; 4: 739–744.
Garand R, Voisin S, Papin S, Praloran V, Lenormand B, Favre M et al. Characteristics of pro-T ALL subgroups: comparison with late T-ALL. The Groupe d'Etude Immunologique des Leucémies. Leukemia 1993; 7: 161–167.
Casasnovas RO, Campos L, Mugneret F, Charrin C, Béné MC, Garand R et al. Immunophenotypic patterns and cytogenetic anomalies in acute non-lymphoblastic leukemia subtypes: a prospective study of 432 patients. Leukemia 1998; 12: 34–43.
Hartigan JA . Clustering algorithms. New York: Wiley, 1975.
Sneath PHA, Sokal RR . Numerical Taxonomy. San Francisco: WH Freeman & Co., 1973.
Bene MC, Bernier M, Casasnovas RO, Castoldi G, Knapp W, Lanza F et al. The reliability and specificity of c-kit for the diagnosis of acute myeloid leukemias and undifferentiated leukemias. The European Group for the Immunological Classification of Leukemias (EGIL). Blood 1998; 92: 596–599.
Buccheri V, Shetty V, Yoshida N, Morilla R, Matutes E, Catovsky D . The role of an anti-myeloperoxidase antibody in the diagnosis and classification of acute leukaemia: a comparison with light and electron microscopy cytochemistry. Br J Haematol 1992; 80: 62–68.
Bennett JM, Catovsky D, Daniel MT, Flandrin G, Galton DA, Gralnick HR et al. Proposals for the classification of the acute leukaemias. French-American-British (FAB) co-operative group. Br J Haematol 1976; 33: 451–458.
Huh HY, Pearce SF, Yesner LM, Schindler JL, Silverstein RL . Regulated expression of CD36 during monocyte-to-macrophage differentiation: potential role of CD36 in foam cell formation. Blood 1996; 87: 2020–2028.
van Schravendijk MR, Handunnetti SM, Barnwell JW, Howard RJ . Normal human erythrocytes express CD36, an adhesion molecule of monocytes, platelets, and endothelial cells. Blood 1992; 80: 2105–2114.
Lo SK, Golenbock DT, Sass PM, Maskati A, Xu H, Silverstein RL . Engagement of the Lewis X antigen (CD15) results in monocyte activation. Blood 1997; 89: 307–314.
Tien HF, Chou CC, Wang CH, Chang CH, Hsing CC . Putative normal counterparts of leukaemic cells from CD7-positive acute myeloid leukaemia can be demonstrated in human haemopoietic tissues. Br J Haematol 1996; 94: 501–506.
Chabannon C, Wood P, Torok-Storb B . Expression of CD7 on normal human myeloid progenitors. J Immunol 1992; 149: 2110–2113.
Barcena A, Muench MO, Galy AH, Cupp J, Roncarolo MG, Phillips JH et al. Phenotypic and functional analysis of T-cell precursors in the human fetal liver and thymus: CD7 expression in the early stages of T- and myeloid-cell development. Blood 1993; 82: 3401–3414.
Bonnet D, Dick JE . Human acute myeloid leukemia is organized as a hierarchy that originates from a primitive hematopoietic cell. Nat Med 1997; 3: 730–737.
Jensen AW, Hokland M, Jorgensen H, Justesen J, Ellegaard J, Hokland P . Solitary expression of CD7 among T-cell antigens in acute myeloid leukemia: identification of a group of patients with similar T-cell receptor beta and delta rearrangements and course of disease suggestive of poor prognosis. Blood 1991; 78: 1292–1300.
Venditti A, Del Poeta G, Buccisano F, Tamburini A, Cox-Froncillo MC, Aronica G et al. Prognostic relevance of the expression of Tdt and CD7 in 335 cases of acute myeloid leukemia. Leukemia 1998; 12: 1056–1063.
Solary E, Casasnovas RO, Campos L, Bene MC, Faure G, Maingon P et al. Surface markers in adult acute myeloblastic leukemia: correlation of CD19+, CD34+ and CD14+/DR--phenotypes with shorter survival. Groupe d'Etude Immunologique des Leucemies (GEIL). Leukemia 1992; 6: 393–399.
Fergedal M, Astrom M, Tidefelt U, Karlsson MG . Differences in CD14 and alpha-naphthyl acetate esterase positivity and relation to prognosis in AML. Leuk Res 1998; 22: 25–30.
Campos L, Guyotat D, Archimbaud E, Devaux Y, Treille D, Larese A et al. Surface marker expression in adult acute myeloid leukaemia: correlations with initial characteristics, morphology and response to therapy. Br J Haematol 1989; 72: 161–166.
Bradstock K, Matthews J, Benson E, Page F, Bishop J . Prognostic value of immunophenotyping in acute myeloid leukemia. Australian Leukaemia Study Group. Blood 1994; 84: 1220–1225.
Del Poeta G, Stasi R, Venditti A, Cox C, Aronica G, Masi M et al. CD7 expression in acute myeloid leukemia. Leuk Lymphoma 1995; 17: 111–119.
Del Poeta G, Stasi R, Venditti A, Suppo G, Aronica G, Bruno A et al. Prognostic value of cell marker analysis in de novo acute myeloid leukemia. Leukemia 1994; 8: 388–394.
Lee EJ, Yang J, Leavitt RD, Testa JR, Civin CI, Forrest A et al. The significance of CD34 and TdT determinations in patients with untreated de novo acute myeloid leukemia. Leukemia 1992; 6: 1203–1209.
Geller RB, Zahurak M, Hurwitz CA, Burke PJ, Karp JE, Piantadosi S et al. Prognostic importance of immunophenotyping in adults with acute myelocytic leukaemia: the significance of the stem-cell glycoprotein CD34 (My10). Br J Haematol 1990; 76: 340–347.
Bassan R, Biondi A, Benvestito S, Tini ML, Abbate M, Viero P, Barbui T et al. Acute undifferentiated leukemia with CD7+ and CD13+ immunophenotype. Lack of molecular lineage commitment and association with poor prognostic features. Cancer 1992; 69: 396–404.
Merle-Beral H, Nguyen Cong Duc L, Leblond V, Boucheix C, Michel A et al. Diagnostic and prognostic significance of myelomonocytic cell surface antigens in acute myeloid leukaemia. Br J Haematol 1989; 73: 323–330.
Schwarzinger I, Valent P, Koller U, Marosi C, Schneider B, Haas O Prognostic significance of surface marker expression on blasts of patients with de novo acute myeloblastic leukemia. J Clin Oncol 1990; 8: 423–430.
Miwa H, Nakase K, Kita K . Biological characteristics of CD7(+) acute leukemia. Leuk Lymphoma 1996; 21: 239–244.
Saxena A, Sheridan DP, Card RT, McPeek AM, Mewdell CC, Skinnider LF . Biologic and clinical significance of CD7 expression in acute myeloid leukemia. Am J Hematol 1998; 58: 278–284.
Kornblau SM, Thall P, Huh YO, Estey E, Andreeff M . Analysis of CD7 expression in acute myelogenous leukemia: martingale residual plots combined with ‘optimal’ cutpoint analysis reveals absence of prognostic significance. Leukemia 1995; 9: 1735–1741.
Reuss Borst MA, Bühring HJ, Schmidt H, Müller CA . AML: immunophenotypic heterogeneity and prognostic significance of c-kit expression. Leukemia 1994; 8: 258–263.
Kanda Y, Hamaki T, Yamamoto R, Chizuka A, Suguro M, Matsuyama T et al. The clinical significance of CD34 expression in response to therapy of patients with acute myeloid leukemia: an overview of 2483 patients from 22 studies. Cancer 2000; 88: 2529–2533.
Kyoda K, Nakamura S, Hattori N, Takeshima M, Nakamura K, Kaya H et al. Lack of prognostic significance of CD34 expression in adult AML when FAB M0 and M3 are excluded. Am J Hematol 1998; 57: 265–266.
Lanza F, Rigolin GM, Moretti S, Latorraca A, Castoldi G . Prognostic value of immunophenotypic characteristics of blast cells in acute myeloid leukemia. Leuk Lymphoma 1994; 13(Suppl 1): 81–85.
Ciolli S, Leoni F, Caporale R, Pascarella A, Salti F, Rossi-Ferrini P . CD34 expression fails to predict the outcome in adult acute myeloid leukemia. Haematologica 1993; 78: 151–155.
Author information
Authors and Affiliations
Additional information
This work was supported by a grant from the CHU of Dijon and by the GOELAMS
Rights and permissions
About this article
Cite this article
Casasnovas, R., Slimane, F., Garand, R. et al. Immunological classification of acute myeloblastic leukemias: relevance to patient outcome. Leukemia 17, 515–527 (2003). https://doi.org/10.1038/sj.leu.2402821
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.leu.2402821
Keywords
This article is cited by
-
Evaluating the prognostic value of CD56 in pediatric acute myeloid leukemia
BMC Cancer (2022)
-
DNAM-1/CD226 is functionally expressed on acute myeloid leukemia (AML) cells and is associated with favorable prognosis
Scientific Reports (2021)
-
A recurrent immunophenotype at diagnosis independently identifies high-risk pediatric acute myeloid leukemia: a report from Children’s Oncology Group
Leukemia (2016)
-
CD34 expression and the outcome of nucleophosmin 1-mutated acute myeloid leukemia
Annals of Hematology (2016)
-
Single-cell sphingosine kinase activity measurements in primary leukemia
Analytical and Bioanalytical Chemistry (2014)