Abstract
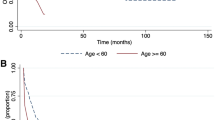
We studied the impact of cytogenetics and kind of induction/consolidation therapy on 848 adult acute myeloid leukemia (AML) patients (age 15–83). The patients received three types of induction/consolidation regimen: standard (daunorubicin and cytosine arabinoside (3/7); two cycles); intensive (idarubicin, cytosine arabinoside and etoposide (ICE), plus mitoxantrone and intermediate-dose Ara-C (NOVIA)); and low-dose (low-dose cytosine arabinoside). CR patients under 60 years of age, if an HLA-identical donor was available received allogeneic stem cell transplantation (allo-SCT); otherwise, as part of the program, they underwent autologous (auto)-SCT. CR rates significantly associated with ‘favorable’ (inv(16), t(8;21)), ‘intermediate’ (‘no abnormality’, abn(11q23), +8, del(7q)) and ‘unfavorable’ (del (5q), −7, abn(3)(q21q26), t(6;9), ‘complex’ (more than three unrelated cytogenetic abnormalities)) karyotypes (88% vs65% vs 36%, respectively; P = 0.0001). these trends were confirmed in all age groups. on therapeutic grounds, intensive induction did not determine significant increases of cr rates in any of the considered groups, with respect to standard induction. low-dose induction was associated with significantly lower cr rates. considering disease-free survival (dfs), multivariate analysis of the factors examined (including karyotype grouping) showed that only age >60 years significantly affected outcome. However, in cases where intensive induction was adopted, ‘favorable’ karyotype was significantly related to longer DFS (P = 0.04). This was mainly due to the favorable outcome of t(8;21) patients treated with intensive induction. Patients receiving allo-SCT had significantly longer DFS (P = 0.005); in particular, allo-SCT significantly improved DFS in the ‘favorable’ and ‘intermediate’ groups (P = 0.04 and P = 0.048, respectively). In conclusion our study could provide some guidelines for AML therapy: (1) patients in the ‘favorable’ karyotype group seem to have a longer DFS when treated with an intensive induction/consolidation regimen, adopted before auto-SCT instead of standard induction; this underlines the importance of reinforcement of chemotherapy, not necessarily based on repeated high-dose AraC cycles. Allo-SCT, independently of induction/consolidation therapy, should be considered an alternative treatment; (2) patients in the ‘intermediate’ karyotype group should receive allo-SCT; (3) patients in the ‘unfavorable’ karyotype group should be treated using investigational chemotherapy, considering that even allo-SCT cannot provide a significantly longer DFS, but only a trend to a better prognosis.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout








Similar content being viewed by others
References
Bloomfield CD, Baer MR, Herzig GP . Acute myeloid leukemia in adults: an update Educational Sessions of the Second EHA 1996 1–7
Bloomfield CD, Shuma C, Regal L, Philip PP, Hossfeld DK, Hagemejier AM, Garson OM, Peterson BA, Sakurai M, Alimena G, Berger R, Rowley JD, Ruutu T, Mitelman F, Dewald GW, Swansbury J . Long-term survival of patients with acute myeloid leukemia Cancer 1997 80: 2191–2198
Berman E . Recent advances in the treatment of acute leukemia Curr Opin Hematol 1997 4: 256–260
Rowe JM, Tallman MS . Intensifying induction therapy in acute myeloid leukemia: has a new standard of care emerged? Blood 1997 90: 2121–2126
Mandelli F, Petti MC, Lo Coco F . Therapy of acute myeloid leukemia: towards a patient-oriented, risk-adapted approach Haematologica 1998 83: 1015–1023
Bassan R, Barbui T . Remission induction therapy for adults with acute myelogenous leukemia: towards the ICE age? Haematologica 1995 80: 82–90
Bishop JF . Does it matter how remission is achieved in acute leukemia? Leukemia 1996 10 (Suppl. 1): S7–S9
Bishop JF . Approaches to induction therapy with adult acute myeloid leukemia Acta Haematol 1998 99: 133–137
Towards an increasingly molecularly-based . Patient-oriented treatment of acute myeloid leukemia. Editorial Haematologica 1996 81: 1–2
Warrel RP Jr, de The H, Wang ZY, Degos L . Acute promyelocytic leukemia N Engl J Med 1993 329: 177–189
Mandelli F, Diverio D, Avvisati G, Luciano A, Barbui T, Bernasconi C, Broccia G, Cerri R, Falda M, Fioritoni G, Leoni F, Liso V, Petti MC, Rodeghiero F, Saglio G, Vegna ML, Visani G, Jehn U, Willemze R, Muus P, Pelicci PG, Biondi A, Lo Coco F . Molecular remission in PML/RAR alpha-positive acute promyelocytic leukemia by combined all-trans retinoic acid and idarubicin (AIDA) therapy Blood 1997 90: 1014–1024
Venditti A, Del Poeta G, Buccisano F, Tamburini A, Cox MC, Stasi R, Bruno A, Aronica G, Maffei L, Suppo G, Simone MD, Forte L, Cordero V, Postorino M, Tufilli G, Isacchi G, Masi M, Papa G, Amadori S . Minimally differentiated acute myeloid leukemia (AML-M0): a distinct clinico–biologic entity with poor prognosis Ann Hematol 1996 72: 208–215
Tallman MS, Neuberg D, Bennet JM, Francois CJ, Paietta E, Wiernik P, Dewald G, Cassileth PA, Oken MM, Rowe JM . Acute megakaryocytic leukemia: the Eastern Cooperative Oncology Group experience Blood 2000 96: 2405–2411
Dassoneville L, Bailly C . Chromosome translocation and leukemias induced by inhibitors of topoisomerase II anticarcinogenetic drugs Bull Cancer 1998 85: 254–261
Van Putten WLJ on behalf of the AML Collaborative Group . Prognostic factors in AML Blood 1997 90 (Suppl. 1): 283-1(Abstr.)
Buchner T, Hiddemann W, Wormann B, Loffler H, Gassmann W, Haferlach T, Fontasch C, Hossfeld D, Maschmeyer G, Lengfelder E, Aul C, Heyll A, Ludwig W-D, Sauerland M-C, Heinecke A . Therapeutic outcome in AML is mainly determined by cytogenetics, LDH in serum, early response and, in poor risk subgroup, by intensified induction treatment Blood 1997 90 (Suppl. 1): 307-IX (Abstr.)
Dastigue N, Payen C, Lafage-Pochitaloff M, Bernard P, Leroux D, Huguet-Rigal F, Stoppa AM, Marit G, Molina L, Michallet M, Maraninchi D, Attal M, Reiffers J . Prognostic significance of karyotype in de novo adult acute leukemia Leukemia 1995 9: 1491–1498
Keating MJ, Smith TL, Kantarjian H, Cork A, Walters R, Trujillo JM, McCredie KB, Gehan EA, Freireich EJ . Cytogenetic pattern in acute myelogenous leukemia: a major reproducible determinant of outcome Leukemia 1988 2: 403–412
Grimwade D, Walker H, Oliver F, Wheatley K, Harrison C, Harrison G, Rees J, Hann I, Stevens R, Burnett A, Goldstone A on behalf of the Medical Research Council Adult and Children's Leukaemia Working Parties . The importance of diagnostic cytogenetics on outcome in AML: analysis of 1612 patients entered into the MRC AML10 Trial Blood 1998 92: 2322–2333
Leith PC, Kopecky KJ, Godwin J, McConnel T, Slovak ML, Chen I M, Head DR, Appelbaum F, Willman CL . Acute myeloid leukemia in the elderly: assessment of multidrug resistance (MDR1) and cytogenetics distinguishes biologic subgroups with remarkably distinct responses to standard chemotherapy. A Southwest Oncology Group Study Blood 1997 89: 3323–3329
Dohner H, Fisher K, Del Valle F, Hartmann F, Pralle H, Fisher JT, Gunzer U, Pezzuto A, Weber W, Grimminger W, Preiss J, Haas R, Schlenk R . Stratification of postremission therapy in adult acute myeloid leukemia according to the karyotype. First result of the AML HD93 multicenter treatment trial Blood 1997 90 (Suppl. 1): 2598 (Abstr.)
Preisler H, Davis RB, Kirshner J, Dupre E, Richards F, Hoagland HC, Kopel S, Levy RN, Carey R, Schulman P, Gottlieb AJ, McIntre OR and the Cancer and Leukemia Group B . Comparison of three remission induction regimens and two postinduction strategies for the treatment of acute nonlymphocytic leukemia: a Cancer and Leukemia Group B study Blood 1987 69: 1441–1449
Berman E . Chemotherapy in acute myeloid leukemia: high dose, higher expectations? J Clin Oncol 1995 13: 1–4
Weick JW, Kopecky KJ, Appelbaum FR, Head DR, Kingsbury LL, Balcerzak SP, Bickers JN, Hynes HE, Welborn JL, Simon SR, Grever M . A randomized investigation of high-dose versus standard-dose cytosine arabinoside with daunorubicin in patients with previously untreated acute myeloid leukemia: a Southwest Oncology Group study Blood 1996 88: 2841–2851
Bennet JM, Catovsky DM, Daniel MT . Proposals for the classification of acute leukaemias Br J Haematol 1977 33: 451–458
Mitelman F . ISCN. An international system for human cytogenetic nomenclature Karger: Basel 1995
Testoni N, Borsaru G, Martinelli G, Carboni C, Ottaviani E, Pelliconi S, Ricci P, Pastano R, Visani G, Zaccari A, Tura S . 3q21 and 3q26 cytogenetic abnormalities in acute myeloblastic leukemia: biological and clinical features Haematologica 1999 84: 690–694
Kaplan EL, Meier P . Non-parametric estimation from incomplete observation J Am Stat Assoc 1958 53: 457–481
Peto R, Pike MC, Armitage ME Breslow NE, Cox DR, Howard SW, Mantel N, McPherson K, Peto J, Smith PG . Design and analysis of randomized clinical trials requiring prolonged observation of each patient. Part II. Analysis and examples Br J Cancer 1977 35: 1–39
Ferrant A, Doyen C, Delannoy A, Straetmans N, Martiat P, Mineur P, Bosly A, Van Den Berghe H, Michaux JL . Karyotype in acute myeloblastic leukemia: prognostic significance in a prospective study assessing bone marrow transplantation in first remission Bone Marrow Transplant 1995 15: 685–690
Ferrant A, Labopin M, Frassoni F, Prentice HG, Cahn JY, Blaise D, Reiffers J, Visani G, Sanz MA, Boogaerts MA, Lowenberg B, Gorin NC . Karyotype in acute myeloblastic leukemia: prognostic significance for bone marrow transplantation in first remission: a European Group for Blood and Marrow Transplantation Study Blood 1997 90: 2931–2938
Wheatley K, Burnett AK, Goldstone AH, Gray RG, Hann IM, Harrison IM, Harrison CJ, Rees JK, Stevens RF, Walker H . A simple, robust, validated and higly predictive index for the determination of risk-directed therapy in acute myeloid leukaemia derived from the MRC AML 10 trial Br J Haematol 1999 107: 69–79
Vogler WR, Velez-Garcia E, Weiner RS, Flaum MA, Bartolucci A A, Omura GA, Gerber MC, Banks PLC . A phase III trial comparing idarubicin and daunorubicin with cytarabine in acute myelogenous leukemia: a Southeastern Cancer Group Study J Clin Oncol 1992 10: 1103–1111
Rowe JM, Andersen JW, Mazza JJ, Bennet JM, Paietta E, Hayes FA, Oette D, Cassileth PA, Stadtmauer EA, Wiernick PH . A randomized placebo-controlled phase III study of granulocyte–macrophage colony stimulating-factor in adult patients (>55 years of age) with acute myelogenous leukemia: a study of the Eastern Oncology Cooperative Group (E1490) Blood 1995 86: 457–462
Lowenberg B, Suciu S, Archimbaud E, Haak H, Stryckmans P, de Cataldo R, Dekker AW, Bernema ZN, Thyss A, Van der Lelie J, Sonnevald P, Visani G, Fillet G, Hayat M, Hagemeijer A, Solbu G, Zittoun R . Mitoxantrone versus daunorubicin in induction-consolidation chemotherapy. The value of low-dose cytarabine for maintenance of remission, and an assessment of prognostic factors in acute myeloid leukemia in the elderly: a final report of the Leukemia Cooperative Group of the European Organization for the research and treatment of cancer and the Dutch–Belgian Hemato–Oncology Cooperative Hovon Group Randomized Phase III Study AML-9 J Clin Oncol 1998 16: 872–881
Willman CL . Immunophenotyping and cytogenetics in older adults with acute myeloid leukemia: significance of expression of multidrug resistance gene-1 (MDR1) Leukemia 1996 10 (Suppl. 1): S33–S35
Schiller G, Gajewski J, Territo M, Nimer S, Lee M, Belin T, Champlin R . Long-term outcome of high-dose cytarabine-based consolidation chemotherapy for adults with acute myelogenous leukemia Blood 1992 80: 2977–2982
Mayer RJ, Davis RB, Schiffer CA, Berg DT, Powell BL, Schulman P, Omura GA, Moore JO, McIntyre OR, Frei E . Intensive postremission chemotherapy in adults with acute myeloid leukemia. Cancer and Leukemia Group B N Engl J Med 1994 331: 896–903
Bloomfield CD, Lawrence D, Byrd JC, Carroll A, Pettenati MJ, Tantravahi R, Patil SR, Davey FR, Berg DT, Schiffer CA, Arthur DC, Mayer RJ . Frequency of prolonged remission duration after high-dose cytarabine intensification in acute myeloid leukemia varies by cytogenetic subtype Cancer Res 1998 58: 4173–4179
Byrd JC, Dodge RK, Carroll A, Baer MR, Edwards C, Stamberg J, Qumsiyeh M, Moore JO, Mayer RJ, Davey F, Schiffer CA, Bloomfield CD . Patients with t(8;21)(q22;q22) and acute myeloid leukemia have superior failure-free and overall survival when repetitive cycles of high-dose cytarabine are administered J Clin Oncol 1999 17: 3767–3775
Acknowledgements
This work was supported in part by MURST ex 40% (S Tura) and FONDI ex 60% (S Tura).
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Visani, G., Bernasconi, P., Boni, M. et al. The prognostic value of cytogenetics is reinforced by the kind of induction/consolidation therapy in influencing the outcome of acute myeloid leukemia – analysis of 848 patients. Leukemia 15, 903–909 (2001). https://doi.org/10.1038/sj.leu.2402142
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.leu.2402142
Keywords
This article is cited by
-
Sex-associated differences in frequencies and prognostic impact of recurrent genetic alterations in adult acute myeloid leukemia (Alliance, AMLCG)
Leukemia (2024)
-
Drugging the unfolded protein response in acute leukemias
Journal of Hematology & Oncology (2015)
-
Improved outcome in relapsed and refractory myeloid malignancies for unrelated vs related donor allogeneic peripheral blood-derived hematopoietic cell transplantation
Bone Marrow Transplantation (2010)
-
Outcome of acute myeloid leukemia patients with hyperleukocytosis in Brazil
Medical Oncology (2010)
-
Interactive diagnostics in the indication to allogeneic SCT in AML
Bone Marrow Transplantation (2009)