Abstract
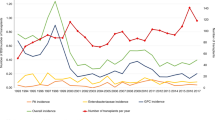
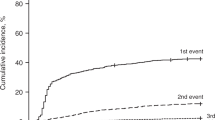
Meticillin-resistant Staphylococcus aureus (MRSA) is a major nosocomial pathogen, with an increased incidence in the UK since 1993, causing serious morbidity and mortality in immunosuppressed patients. We analysed the frequency and outcome of MRSA infection in a single-centre transplant population over a 5-year period. The total number of patients infected was 41/776 (5%). The frequency in autologous, sibling and unrelated donor transplants was 3, 6 and 9%, respectively. Prior to 2004, the incidence was <4%/year; however, an outbreak in the day unit resulted in 22 patients becoming newly infected. Over 90% of infections were clinically relevant, half (49%) being bacteraemia. Three patterns were seen: known MRSA positive at any time before transplant (n=15), MRSA first detected during the neutropenia phase (n=5) and MRSA only post discharge (n=21). MRSA was implicated in a number of deaths, at all time points, in those infected. An intensive eradication policy resulted in new infections dropping to <2%. In conclusion, MRSA is likely to remain endemic in our unit, but robust early screening protocols and aggressive eradication strategies have effectively limited the spread of and morbidity due to this pathogen.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Stefani S, Varaldo PE . Epidemiology of methicillin-resistant staphylococci in Europe. Clin Microbiol Infect 2003; 9: 1179–1186.
Fridkin SK, Hageman JC, Morrison M, Sanza LT, Como-Sabetti K, Jernigan JA et al. Methicillin-resistant Staphylococcus aureus disease in three communities. N Engl J Med 2005; 352: 1436–1444.
Bronzwaer SL, Buchholz U, Kool JL . International surveillance of antimicrobial resistance in Europe: now we also need to monitor antibiotic use. Euro Surveill 2001; 6: 1–2.
Kottaridis PD, Milligan DW, Chopra R, Chakraverty RK, Chakrabarti S, Robinson S et al. In vivo CAMPATH-1H prevents graft-versus-host disease following nonmyeloablative stem cell transplantation. Blood 2000; 96: 2419–2425.
Matsubara H, Makimoto A, Higa T, Kawamoto H, Kanda Y, Kami M et al. Successful treatment of meningoencephalitis caused by methicillin-resistant Staphylococcus aureus with intrathecal vancomycin in an allogeneic peripheral blood stem cell transplant recipient. Bone Marrow Transplant 2003; 31: 65–67.
Kato N, Tanaka J, Mori A, Tutumi Y, Yonezumi M, Chiba K et al. The risk of persistent carriage of methicillin-resistant Staphylococcus aureus in hematopoietic stem cell transplantation. Ann Hematol 2003; 82: 310–312.
Imataki O, Makimoto A, Kato S, Bannai T, Numa N, Nukui Y et al. Coincidental outbreak of methicillin-resistant Staphylococcus aureus in a hematopoietic stem cell transplantation unit. Am J Hematol 2006; 81: 664–669.
Guidelines for preventing opportunistic infections among hematopoietic stem cell transplant recipients. Biol Blood Marrow Transplant 2000; 6: 659–713; 715; 717–727; quiz 729–733.
Bertz H, Auner HW, Weissinger F, Salwender HJ, Einsele H, Egerer G et al. Antimicrobial therapy of febrile complications after high-dose chemo-/radiotherapy and autologous hematopoietic stem cell transplantation – guidelines of the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Oncology (DGHO). Ann Hematol 2003; 82 (Suppl 2): S167–S174.
Coia JE, Duckworth GJ, Edwards DI, Farrington M, Fry C, Humphreys H et al. Guidelines for the control and prevention of meticillin-resistant Staphylococcus aureus (MRSA) in healthcare facilities. J Hosp Infect 2006; 63 (Suppl 1): S1–S44.
Muller AA, Mauny F, Bertin M, Cornette C, Lopez-Lozano JM, Viel JF et al. Relationship between spread of methicillin-resistant Staphylococcus aureus and antimicrobial use in a French university hospital. Clin Infect Dis 2003; 36: 971–978.
Hori S, Sunley R, Tami A, Grundmann H . The Nottingham Staphylococcus aureus population study: prevalence of MRSA among the elderly in a university hospital. J Hosp Infect 2002; 50: 25–29.
Harbarth S, Liassine N, Dharan S, Herrault P, Auckenthaler R, Pittet D . Risk factors for persistent carriage of methicillin-resistant Staphylococcus aureus. Clin Infect Dis 2000; 31: 1380–1385.
Fujita S, Senda Y, Iwagami T, Hashimoto T . Rapid identification of staphylococcal strains from positive-testing blood culture bottles by internal transcribed spacer PCR followed by microchip gel electrophoresis. J Clin Microbiol 2005; 43: 1149–1157.
Lodise TP, McKinnon PS . Clinical and economic impact of methicillin resistance in patients with Staphylococcus aureus bacteremia. Diagn Microbiol Infect Dis 2005; 52: 113–122.
Cosgrove SE, Qi Y, Kaye KS, Harbarth S, Karchmer AW, Carmeli Y . The impact of methicillin resistance in Staphylococcus aureus bacteremia on patient outcomes: mortality, length of stay, and hospital charges. Infect Control Hosp Epidemiol 2005; 26: 166–174.
Cooper BS, Stone SP, Kibbler CC, Cookson BD, Roberts JA, Medley GF et al. Isolation measures in the hospital management of methicillin resistant Staphylococcus aureus (MRSA): systematic review of the literature. BMJ 2004; 329: 533.
Cepeda JA, Whitehouse T, Cooper B, Hails J, Jones K, Kwaku F et al. Isolation of patients in single rooms or cohorts to reduce spread of MRSA in intensive-care units: prospective two-centre study. Lancet 2005; 365: 295–304.
Barakate MS, Yang YX, Foo SH, Vickery AM, Sharp CA, Fowler LD et al. An epidemiological survey of methicillin-resistant Staphylococcus aureus in a tertiary referral hospital. J Hosp Infect 2000; 44: 19–26.
Anstead GM, Owens AD . Recent advances in the treatment of infections due to resistant Staphylococcus aureus. Curr Opin Infect Dis 2004; 17: 549–555.
Patti JM . A humanized monoclonal antibody targeting Staphylococcus aureus. Vaccine 2004; 22 (Suppl 1): S39–S43.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shaw, B., Boswell, T., Byrne, J. et al. Clinical impact of MRSA in a stem cell transplant unit: analysis before, during and after an MRSA outbreak. Bone Marrow Transplant 39, 623–629 (2007). https://doi.org/10.1038/sj.bmt.1705654
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bmt.1705654
Keywords
This article is cited by
-
Anforderungen an die Infektionsprävention bei der medizinischen Versorgung von immunsupprimierten Patienten
Bundesgesundheitsblatt - Gesundheitsforschung - Gesundheitsschutz (2021)
-
Bacterial bloodstream infections in the allogeneic hematopoietic cell transplant patient: new considerations for a persistent nemesis
Bone Marrow Transplantation (2017)
-
Infection Prevention in Transplantation
Current Infectious Disease Reports (2016)
-
Infection Probability Score, APACHE II and KARNOFSKY scoring systems as predictors of bloodstream infection onset in hematology-oncology patients
BMC Infectious Diseases (2010)
-
Typing of Staphylococcal Cassette Chromosome mec Encoding Methicillin Resistance in Staphylococcus aureus Strains Isolated at the Bone Marrow Transplant Centre of Tunisia
Current Microbiology (2009)