Abstract
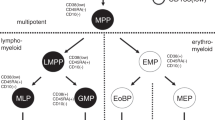
A pediatric patient with very early meningeal relapse of his CD34+ CD133− pre-B-ALL was transplanted with 2.5 × 106/kg CD133 selected autologous progenitor cells. Enrichment of CD133+ cells resulted in a purity of 92.3 ± 3.5% CD133+. Hematopoietic engraftment with >1.0 × 109/l neutrophils and >50 × 109/l platelets was reached within 13 and 24 days, respectively. At a follow-up of 11½ months after autologous transplantation, the patient is in complete remission. To our knowledge, the successful transplantation with a CD133 selected graft is the first one to be reported worldwide. CD133 selected cells may serve as an alternative in the case of CD34+ malignancy.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Messina C, Valsecchi MG, Arico M et al. Autologous bone marrow transplantation for treatment of isolated central nervous system relapse of childhood acute lymphoblastic leukemia Bone Marrow Transplant 1998 21: 9 14
Brenner MK, Rill DR, Moen RC et al. Gene-marking to trace origin of relapse after autologous bone marrow transplantation Lancet 1993 341: 85 86
Handgretinger R, Lang P, Schumm P et al. Isolation and transplantation of autologous peripheral CD34+ progenitor cells highly purified by magnetic-activated cell sorting Bone Marrow Transplant 1998 21: 987 993
Koehl U, Esser R, Zimmermann S et al. Large scale purification of progenitor cells by AC133+ selection Bone Marrow Transplant 2001 27: 296 (Abstr. P736)
Yin AH, Miraglia S, Zanjani ED et al. AC133, a novel marker for human hematopoietic stem and progenitor cells Blood 1997 12: 5002 5012
Koehl U, Gunkel M, Gruettner HP et al. Positive selection of hematopoietic progenitor cells for autologous and allogeneic transplantation in pediatric patients with solid tumors and leukemia Transplant Hematol Oncol 1999 1: 159 168
Schumm M, Lang P, Taylor G et al. Isolation of highly purified autologous and allogeneic peripheral CD34+ cells using the CliniMACS device J Hematother 1999 6: 5 11
Barsch G, Baumann M, Ritter J et al. Expression of AC133 and CD117 on candidate normal stem cell populations in childhood B-cell precursor acute lymphoblastic leukemia Br J Haematol 1999 107: 572 580
Bühring HJ, Seiffert M, Marxer A et al. AC133 antigen is not restricted to acute myeloid leukemic blasts but is also found on acute lymphoid leukemia blasts and on subset of CD34+ B-cell precursors Blood 1999 2: 832 833
Kobari L, Giarratana MC, Pflumic F et al. CD133 cell selection is an alternative to CD34+ cell selection for ex vivo expansion of hematopoietic stem cells J Hematother Stem Cell Res 2001 10: 273 281
Matsumoto K, Kazuta Y, Yamashita N et al. In vitro proliferation potential of AC133 positive cells in peripheral blood Stem Cells 2000 18: 196 203
Gallacher L, Murdoch B, Wu DM et al. Isolation and characterization of human CD34−Lin− and CD34+Lin− hematopoietic stem cells using cell surface markers AC133 and CD7 Blood 2000 9: 2813 2820
Acknowledgements
This project was supported by ‘Hilfe für Krebskranke Kinder Frankfurt eV’, by ‘Frankfurter Stiftung für Krebskranke Kinder’ and by ‘Paul und Ursula Klein-Stiftung’. We acknowledge the excellent technical support of Andrea Brinkmann, Ilse Bühler and Stephanie Grohal.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Koehl, U., Zimmermann, S., Esser, R. et al. Autologous transplantation of CD133 selected hematopoietic progenitor cells in a pediatric patient with relapsed leukemia. Bone Marrow Transplant 29, 927–930 (2002). https://doi.org/10.1038/sj.bmt.1703558
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bmt.1703558
Keywords
This article is cited by
-
CD133+CD34+ stem cells are mobilized after musculoskeletal surgery and target endothelium activated by surgical wound fluid
Langenbeck's Archives of Surgery (2011)
-
Proliferation and differentiation potential of CD133+ and CD34+ populations from the bone marrow and mobilized peripheral blood
Annals of Hematology (2011)
-
ISHAGE-based single-platform flowcytometric analysis for measurement of absolute viable T cells in fresh or cryopreserved products: CD34/CD133 selected or CD3/CD19 depleted stem cells, DLI and purified CD56+CD3− NK cells
International Journal of Hematology (2008)