Abstract
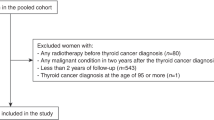
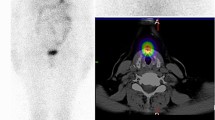
The aim of this study was to evaluate the incidence and risk factors related to secondary thyroid carcinoma (STC) in patients who have undergone allogeneic BMT during childhood. Data related to the primary hematological disorder and BMT procedure were obtained from the records of 113 patients (42 F; 71 M) who underwent BMT before the age of 18 (median 10.0 years; range 1.7–18.0) and survived more than 3 years after transplant with a median follow-up of 10.1 years (range 3.0–19.0). Sixteen received cranial radiation (CRT) during first-line treatment. Pre-transplant conditioning included TBI in 85 patients, TAI in two, while 26 children did not receive irradiation. The standardized incidence ratio of STC after BMT was significantly higher (P < 0.001) than that of the general population. STC was found in eight patients, 3.1 to 15.7 years after transplant. All received TBI and three also CRT. The Cox's regression analysis, although not statistically significant due to the small study population, showed an increased risk in those who had received a cumulative radiation dose higher than 10 Gy and in those who developed chronic GVHD. Careful follow-up of thyroid status including annual ultrasound examination is recommended for early detection of tumor.
Bone Marrow Transplantation (2001) 28, 1125–1128.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Deeg HJ, Socié G . Malignancies after hematopoietic stem cell transplantation: many questions, some answers Blood 1998 91: 1833–1844
Witherspoon RP, Fisher LD, Schoch G et al. Secondary cancer after bone marrow transplantation for leukemia or aplastic anemia New Engl J Med 1989 321: 784–789
Socié G, Henry-Amar M, Cosset JM et al. Increased incidence of solid malignant tumors after bone marrow transplantation for severe aplastic anemia Blood 1991 78: 277–279
Bhatia S, Ramsay NK, Steinbuch M et al. Malignant neoplasms following bone marrow transplantation Blood 1996 87: 3633–3639
Lowsky R, Lipton J, Fyles G et al. Secondary malignancies after bone marrow transplantation in adults J Clin Oncol 1994 12: 2187–2192
Deeg HJ, Socié G, Henry-Amar M et al. Malignancies after marrow transplantation for aplastic anemia and Fanconi anemia: a joint Seattle and Paris analysis of results in 700 patients Blood 1996 87: 386–392
Curtis ER, Rowlings PA, Deeg HJ et al. Solid cancers after bone marrow transplantation New Engl J Med 1997 336: 897–904
Kolb HJ, Socié G, Duell T et al. Malignant neoplasms in long-term survivors of bone marrow transplantation Ann Intern Med 1999 131: 738–744
Sociè G, Curtis RE, Sobocinski KA et al. New malignant diseases after allogeneic marrow transplantation for childhood acute leukemia J Clin Oncol 2000 18: 348–357
Uderzo C, van Lint MT, Rovelli A et al. Papillary thyroid carcinoma after total body irradiation Arch Dis Child 1994 71: 256–258
Rovelli A, Cohen A, Uderzo C et al. Follicular cell carcinoma of the thyroid in a child after bone marrow transplantation for acute lymphoblastic leukemia Acta Haematol 1997 97: 225–227
Epilog Plus Statistics Package for Epidemiology and Clinical Trials Pasadena, CA: Epicenter Software 1988
Parkin DM, Whelan SL, Ferlag J et al. Cancer Incidence in Five Continents Vol. VII: IARC Scientific Publications: Lyon 1997 p 143
SPSS 9 Statistical Package SPSS Inc: Chicago, IL 1999
Viswanathan K, Gierlowski TC, Schneider AB . Childhood thyroid cancer Arch Pediatr Adolesc Med 1994 148: 260–265
Ron E, Lubin JH, Shore RE et al. Thyroid cancer after exposure to external radiation: a pooled analysis of seven studies Radiat Res 1995 141: 259–277
Bessho F, Ohta K, Akanuma A, Sakata KI . Dosimetry of radiation scattered to thyroid gland from prophylactic cranial irradiation for childhood leukemia Pediatr Haematol Oncol 1994 11: 47–53
Beatty O III, Hudson MM, Greenwald C et al. Subsequent malignancies in children and adolescents after treatment for Hodgkin's disease J Clin Oncol 1995 13: 603–609
Sankila R, Garwicz S, Olsen JH et al. Risk of subsequent malignant neoplasms among 1641 Hodgkin's disease patients diagnosed in childhood and adolescence: a population-based cohort study in the five Nordic countries J Clin Oncol 1997 14: 1442–1446
Neglia JP, Meadows AT, Robison LL et al. Second neoplasms after acute lymphoblastic leukemia in childhood New Engl J Med 1991 325: 1330–1336
Black P, Straaten A, Gutjahr P . Secondary thyroid carcinoma after treatment for childhood cancer Med Pediatr Oncol 1998 31: 91–95
Katsanis E, Shapiro RS, Robison LL et al. Thyroid dysfunction following bone marrow transplantation: long-term follow-up of 80 pediatric patients Bone Marrow Transplant 1990 5: 335–340
Borgstrom B, Bolme P . Thyroid function in children after allogeneic bone marrow transplantation Bone Marrow Transplant 1994 13: 59–64
Acknowledgements
We thank the nonprofit ‘Associazione CRESCI’ and ‘Comitato ML Verga’ for their help in the accomplishment of this study and Miss J Upton for linguistic consultancy and secretarial assistance.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Cohen, A., Rovelli, A., van Lint, M. et al. Secondary thyroid carcinoma after allogeneic bone marrow transplantation during childhood. Bone Marrow Transplant 28, 1125–1128 (2001). https://doi.org/10.1038/sj.bmt.1703290
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bmt.1703290
Keywords
This article is cited by
-
Radiotherapy for childhood cancer and subsequent thyroid cancer risk: a systematic review
European Journal of Epidemiology (2018)
-
Thyroid carcinoma in children, adolescents and adults, both spontaneous and after childhood radiation exposure
European Journal of Pediatrics (2016)
-
Second cancers and late mortality in Australian children treated by allogeneic HSCT for haematological malignancy
Leukemia (2015)
-
Secondary solid tumors after allogeneic hematopoietic SCT in Japan
Bone Marrow Transplantation (2012)
-
Endocrine late effects after total body irradiation in patients who received hematopoietic cell transplantation during childhood: a retrospective study from a single institution
Journal of Cancer Research and Clinical Oncology (2011)