Abstract
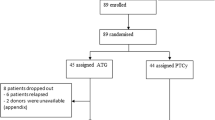
We compared the occurrence of severe infections following 71 reduced-intensity conditioning (RIC) allogeneic peripheral blood stem cell transplants (PBSCT) and 123 standard myeloablative PBSCT (MINI and STAND groups, respectively) from HLA-identical siblings. The probability of 1-year infection-related mortality (IRM) was 19% in the STAND group and 10% in the MINI group (log-rank, P = 0.3). On multivariate analysis the only significant variable associated with a higher risk of IRM was the development of moderate-to-severe GVHD (P = 0.005). The probability of developing CMV infection was 39% in the STAND group and 21% in the MINI group (P = 0.03) (43% and 21%, respectively, in seropositive donor/recipient pairs, P = 0.01), and the probability of developing CMV disease was 9.5% and 1%, respectively (P = 0.05) (11% and 1%, respectively, in seropositive donor/recipient pairs, P = 0.03). Multivariate analysis of CMV infection identified four variables associated with a higher risk: CMV positive serostatus (P = 0.05), STAND transplant group (P = 0.02), the development of moderate-to-severe GVHD (P < 0.001) and a dose of CD34+ cells infused below 6 × 106/kg (P = 0.01). Invasive fungal infections and pneumonias of unknown origin did not differ between groups, and neither did other severe non-CMV viral infections and bacterial infections. Our results suggest that RIC allogeneic PBSCT may decrease the risk of dying from an opportunistic infection and reduces the occurrence of CMV infection and disease. Overall, the development of GVHD (acute or chronic) is an important risk factor for these complications. Other infections continue to pose a significant threat to recipients of RIC allografts, stressing that prophylactic and supportive measures are an important aspect in their care. Bone Marrow Transplantation (2001) 28, 341–347.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Giralt S, Estey E, Albitar M et al. Engraftment of allogeneic hematopoietic progenitor cells with purine analog-containing chemotherapy: harnessing graft-versus-leukemia without myeloablative therapy Blood 1997 89: 4531–4536
Slavin S, Nagler A, Naparstek E et al. Nonmyeloablative stem cell transplantation and cell therapy as an alternative to conventional bone marrow transplantation with lethal cytoreduction for the treatment of malignant and nonmalignant hematologic diseases Blood 1998 91: 756–763
Khouri IF, Keating M, Körbling M et al. Transplant-lite. Induction of graft-versus-malignancy using fludarabine-based nonablative chemotherapy and allogeneic blood progenitor-cell transplantation as treatment for lymphoid malignancies J Clin Oncol 1998 16: 2817–2824
Carella AM, Lerma E, Dejana A et al. Engraftment of HLA-matched sibling hematopoietic stem cells after immunosuppressive conditioning regimen in patients with hematologic neoplasias Haematologica 1998 83: 904–909
McSweeney P, Niederwieser D, Shizuru J et al. Outpatient allografting with minimally myelosuppressive, immunosuppressive conditioning of low-dose TBI and postgrafting cyclosporine and mycophenolate mofetil Blood 1999 94: (Suppl. 1) 393a
Childs R, Clave E, Contentin N et al. Engraftment kinetics after nonmyeloablative allogeneic peripheral blood stem cell transplantation: full donor T-cell chimerism precedes alloimmune responses Blood 1999 94: 3234–3241
Carella AM, Champlin R, Slavin S et al. Mini-allografts: ongoing trials in humans Bone Marrow Transplant 2000 25: 345–350
Engels EA, Ellis CA, Supran SE et al. Early infections in bone marrow transplantation: Quantitative study of clinical factors that affect risk Clin Infect Dis 1999 28: 256–266
Blijlevens NMA, Donnelly JP, De Pauw BE . Mucosal barrier injury: biology, pathology, clinical counterparts and consequences of intensive treatment for haematological malignancy: an overview Bone Marrow Transplant 2000 25: 1269–1278
Parkman R, Weinberg KI . Immunological reconstitution following hematopoietic stem cell transplantation In: Thomas ED, Blume KG, Forman SJ (eds) Hematopoietic Cell Transplantation 2nd edn Blackwell Scientific Publications: Boston, MA 1999 pp 704–711
Przepiorka D, Weisdorf D, Martin P et al. 1994 Consensus conference on acute GVHD grading Bone Marrow Transplant 1995 15: 825–828
Martino R, Caballero MD, Canals C et al. Allogeneic peripheral blood stem cell transplantation with reduced-intensity conditioning: results of a prospective multicenter study Br J Haematol (in press)
Clift RA, Buckner CD, Appelbaum FR et al. Allogeneic marrow transplantation in patients with acute myeloid leukemia in first remission: a randomized trial of two irradiation regimens Blood 1990 76: 1876–1871
Clift RA, Buckner CD, Appelbaum FR et al. Allogeneic marrow transplantation in patients with chronic myeloid leukemia in the chronic phase: a randomized trial of two irradiation regimens Blood 1991 77: 1660–1665
Mohty M, Faucher C, Vey N et al. High rate of secondary viral and bacterial infections in patients undergoing allogeneic bone marrow mini-transplantation Bone Marrow Transplant 2000 26: 251–255
Hensel N, Almeida K, Bahceci E et al. Factors affecting incidence and timing of cytomegalovirus reactivation after allogeneic peripheral blood stem cell transplants Blood 1999 94: (Suppl. 1) 337a
Chakrabarti S, Kottaridis P, Ogormon P et al. High incidence of early and late CMV infection and delayed immune reconstitution after allogeneic transplants with nonmyeloablative conditioning using CAMPATH (anti-CD52 antibody) Blood 2000 96: (Suppl. 1) 586a
Reddy V, Pollock BH, Sharda S et al. GVHD and CMV antigenemia after allogeneic peripheral blood stem cell transplantation: comparison between myeloablative and non-myeloablative (mini) conditioning regimens Blood 2000 96: (Suppl. 1) 191a
Small TN, Avigan D, Dupont B et al. Immune reconstitution following T-cell depleted bone marrow transplantation: effect of age and posttransplant graft rejection prophylaxis Biol Blood Marrow Transplant 1997 3: 65–75
Junghanss C, Boeckh M, Carter R et al. Incidence of herpesvirus infections following nonmyeloablative allogeneic stem cell transplantation Blood 2000 96: (Suppl. 1) 188a
Ringdén O, Nilsson B . Death by graft-versus-host disease associated with HLA mismatch, high recipient age, low marrow cell dose and splenectomy Transplantation 1985 40: 39–44
Mavroudis D, Fox M, Read EJ et al. Effect of CD34+ cell dose on outcome following T-depleted marrow transplantation Blood 1996 88: 3223–3229
Sierra J, Storer B, Hansen JA et al. Transplantation of marrow cells from unrelated donors for treatment of high-risk acute leukemia: the effect of leukemia burden, donor HLA-matching and marrow cell dose Blood 1997 89: 4226–4235
Barrett AJ, Ringdén O, Zhang M-J et al. Effect of nucleated marrow cell dose on relapse and survival in identical twin bone marrow transplants for leukemia Blood 2000 95: 3323–3327
Bahçeci E, Read E, Leitman S et al. CD34+ cell dose predicts relapse and survival after T-cell-depleted HLA-identical haematopoietic stem cell transplantation (HSCT) for haematological malignancies Br J Haematol 2000 108: 408–414
Martino R, Rovira M, Carreras E et al. Severe infections after allogeneic peripheral blood stem cell transplantation: a comparison of unmanipulated and CD34+ cell-selected transplantation (submitted for publication)
Author information
Authors and Affiliations
Consortia
Rights and permissions
About this article
Cite this article
Martino, R., Caballero, M., Canals, C. et al. Reduced-intensity conditioning reduces the risk of severe infections after allogeneic peripheral blood stem cell transplantation. Bone Marrow Transplant 28, 341–347 (2001). https://doi.org/10.1038/sj.bmt.1703150
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bmt.1703150
Keywords
This article is cited by
-
Pushing the envelope—nonmyeloablative and reduced intensity preparative regimens for allogeneic hematopoietic transplantation
Bone Marrow Transplantation (2015)
-
Reduction of infection-related mortality after allogeneic PBSCT from HLA-identical siblings: longitudinal analysis from 1994 to 2008 at a single institution
Bone Marrow Transplantation (2011)
-
Surveillance of active human cytomegalovirus infection in hematopoietic stem cell transplantation (HLA sibling identical donor): search for optimal cutoff value by real-time PCR
BMC Infectious Diseases (2010)
-
Cytomegalovirus infection and disease after reduced intensity conditioning allogeneic stem cell transplantation: single-centre experience
Bone Marrow Transplantation (2010)
-
Lower respiratory tract respiratory virus infections increase the risk of invasive aspergillosis after a reduced-intensity allogeneic hematopoietic SCT
Bone Marrow Transplantation (2009)