Abstract
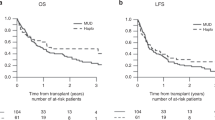
We compared the outcomes in patients receiving unrelated peripheral blood stem cell transplants (PBSCT) with those receiving bone marrow transplants (BMT) in a matched pair analysis. Seventy-four patients with hematological malignancies with HLA-matched (77%) and mismatched (23%) donors were analyzed in this study. Thirty-four patients (45%) were considered as high risk patients. Sixty-eight patients received standard conditioning regimens with Bu/Cy or TBI/Cy. Six patients received an intensified conditioning regimen with the addition of etoposide, thiotepa or melphalan. GVHD prophylaxis consisted of prednisolone, cyclosporine and methotrexate. Groups were matched for patient, donor, transplant characteristics and HLA compatibility. Peripheral blood stem cell collection led to the collection of a higher number of CD34+ and CD3+ cells in comparison to bone marrow collection. Leukocyte engraftment in the PBSCT group occurred in 14 days (median; range 6–26 days) and in the BMT group in 19 days (range 9–29 days; P < 0.02). The time of platelet engraftment did not differ significantly. The incidence of grades II–lV acute GVHD in the group of HLA-identical patients was 35% in the PBSCT group and 25% in the BMT group (P < 0.33, log-rank). However, there was a significant difference (P < 0.05, log-rank) in incidence and time to onset of acute GVHD II–IV comparing all patients, including the 17 mismatched transplants. Disease-free survival was 51% (19 patients) with a median of 352 days and 59% (21 patients) with a median of 760 days for PBSC and BMT transplants, respectively. In conclusion, our results indicate that allogeneic PBSCT led to significantly faster leukocyte engraftment but is associated with a higher incidence and more rapid onset of severe acute GVHD comparing all patients, including the 17 mismatched transplants. However, the incidence of severe acute GVHD in HLA-identical patients was not different between the PBSCT and BMT groups. Bone Marrow Transplantation (2001) 27, 27–33.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout








Similar content being viewed by others
References
Kessinger A, Smith DM, Strandjord SE et al. Allogeneic transplantation of blood-derived, T cell-depleted hematopoietic stem cells after myeloablative treatment in a patient with acute lymphoblastic leukemia Bone Marrow Transplant 1989 4: 643–646
Schmitz N, Bacigalupo A, Labopin M et al. Transplantation of allogeneic peripheral blood progenitor cells – the EBMT experience Bone Marrow Transplant 1996 17: (Suppl. 2) 40–46
Körbling M, Przepiorka D, Huh YO et al. Allogeneic blood stem cell transplantation: peripheralization and yield of donor-derived primitive hematopoietic progenitor cells (CD34+ Thy-1dim) and lymphoid subsets, and possible predictors of engraftment and graft-versus-host disease Blood 1995 86: 2842–2848
Russell JA, Brown C, Bowen T et al. Allogeneic blood cell transplants for haematological malignancy: preliminary comparison of outcomes with bone marrow transplantation Bone Marrow Transplant 1996 17: 703–708
Bensinger WI, Clift R, Martin P et al. Allogeneic peripheral blood progenitor cell transplantation in patients with advanced hematologic malignancies: a retrospective comparison with marrow transplantation Blood 1996 88: 2794–2800
Ottinger HD, Beelen DW, Scheulen B et al. Improved immune reconstitution after allotransplantation of peripheral blood stem cells instead of bone marrow Blood 1996 88: 2775–2779
Sierra J, Storer B, Hansen JA et al. Transplantation of marrow cells from unrelated donors for treatment of high-risk acute leukemia: the effect of leukemia burden, donor HLA-matching, and marrow cell dose Blood 1997 89: 4226–4235
Urbano-Ispizua A, Solano C, Brunet S et al. Allogeneic peripheral blood progenitor cell transplantation: analysis of short-term engraftment and acute GVHD incidence in 33 cases Bone Marrow Transplant 1996 18: 35–40
Storek J, Gooley T, Siadak M et al. Allogeneic peripheral blood stem cell transplantation may be associated with a high risk of chronic graft-versus-host disease Blood 1997 90: 4705–4709
Scott MA, Gandhi MK, Jestice HK et al. A trend towards an increased incidences of chronic graft-versus-host disease following allogeneic peripheral blood progenitor cell transplantation: a case controlled study Bone Marrow Transplant 1998 22: 273–276
Bensinger W, Martin P, Clift R et al. A prospective, randomized trail of peripheral blood stem cell (PBSC) transplants or marrow (BM) for patients undergoing allogeneic transplantation for hematologic malignancies Blood 1999 10: (Suppl. 1) 368a (Abstr. 1637)
Durant S . Morton AJ. A randomized trial of filgrastim (G-CSF) stimulated donor marrow (BM) versus peripheral blood (PBSC) for allogeneic transplantation: increased extensive chronic GVHD following PBSC transplantation Blood 1999 10: (Suppl. 1) 608a (Abstr. 2706)
Anderlini P, Przepiorka D, Körbling M, Champlin R . Blood stem cell procurement: donor safety issues Bone Marrow Transplant 1998 21: (Suppl. 3) 35–39
Bensinger WI, Price TH, Dale DC et al. The effects of daily recombinant human granulocyte colony stimulating factor administration on normal granulocyte donors undergoing leukapheresis Blood 1998 81: 1883–1888
Becker PS, Wagle M, Matous S et al. Spontaneous splenic rupture following administration of granulocyte colony stimulating factor (G-CSF): occurence in an allogeneic donor of peripheral blood stem cells Blood Marrow Transplant 1997 3: 45–49
Basara N, Blau IW, Kiehl MG et al. Mycophenolate mofetil for the prophylaxis of acute GVHD in HLA-mismatched bone marrow transplant patients Clin Transplant 2000 14: 121–126
Hägglund H, Ringden O, Remberger M et al. Faster neutrophil and platelet engraftment, but no differences in acute GVHD or survival using peripheral blood stem cells from related and unrelated donors, compared to bone marrow Bone Marrow Transplant 1998 22: 131–136
Thomas ED, Storb R, Clift RA et al. Bone marrow transplantation. Parts I, II New Engl J Med 1975 293: 832–840, 895–902
Przepiorka D, Weisdorf D, Martin P et al. Meeting report: concensus conference on acute GVHD grading Bone Marrow Transplant 1995 15: 825–828
Shulman HM, Sullivan KM, Weiden PI et al. Chronic graft-versus-host syndrome in man. A long term clinicopathologic study of 20 Seattle patients Am J Med 1980 69: 204–217
Peto R, Pike MC, Armitage P et al. Design and analysis of randomized clinical trails requiring prolonged observation of each patient. II. Analysis and examples Br J Cancer 1977 35: 1–39
Armitage P, Berry G . Statistical Methods in Medical Research Blackwell Science: Oxford 1987
Ringden O, Lönnqvist B, Hägglind H et al. Transplantation with peripheral blood stem cells from unrelated donors without serious graft-versus-host disease Bone Marrow Transplant 1995 16: 856–857
Blaise D, Kuentz M, Fortanier C et al. Randomized trial of bone marrow versus lenograstim-primed blood cell allogeneic transplantation in patients with early-stage leukemia: a report from the Societe Française de Greffe de Moelle J Clin Oncol 2000 18: 537–546
Schmitz N, Bacigalupo A, Hasenclever D et al. Allogeneic bone marrow transplantation vs filgrastim-mobilized peripheral blood progenitor cell transplantation in patients with early leukaemia: first results of a randomized multicenter trial of the European group for Blood and Marrow Transplantation Bone Marrow Transplant 1998 21: 995–1003
Ringden O, Remberger M, Runde V et al. Peripheral blood stem cell transplantation from unrelated donors: a comparison with marrow transplantation Blood 1999 94: 455–464
Stockschläder M, Löliger C, Krüger W et al. Transplantation of allogeneic rhG-CSF mobilized peripheral CD34+ cells from an HLA-identical unrelated donor Bone Marrow Transplant 1995 16: 719–722
Pan L, Delmonte J Jr, Jalonen C et al. Pretreatment of donor mice with granulocyte colony stimulating factor polarizes donor T-lymphocytes toward type-2 cytokine production and reduces severity of experimental graft-versus-host-disease Blood 1995 86: 4422–4429
Tayebi H, Tiberghien P, Kuentz M et al. Comparison of HLA-identical allogeneic bone marrow (BM) versus peripheral blood stem cells (PBSC) transplantation: phenotypical and functional study of donor T cells in the graft and after hematopoietic reconstitution Blood 1998 92: 140 (Abstr. 562)
Anderlini P, Körbling M, Dale D et al. Allogeneic blood stem cell transplantation: considerations for donors Blood 1997 90: 903–908
Storek J, Dawson M, Maloney DG . Normal T,B, and NK cell counts in healthy donors at 1 year after blood stem cell harvesting (letter) Blood 2000 95: 2993–2994
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Blau, I., Basara, N., Lentini, G. et al. Feasibility and safety of peripheral blood stem cell transplantation from unrelated donors: results of a single-center study. Bone Marrow Transplant 27, 27–33 (2001). https://doi.org/10.1038/sj.bmt.1702734
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bmt.1702734
Keywords
This article is cited by
-
Transplantation of highly purified peripheral-blood CD34+ progenitor cells from related and unrelated donors in children with nonmalignant diseases
Bone Marrow Transplantation (2004)
-
Patients with acute lymphoblastic leukaemia allografted with a matched unrelated donor may have a lower survival with a peripheral blood stem cell graft compared to bone marrow
Bone Marrow Transplantation (2003)