Abstract
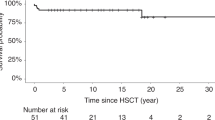
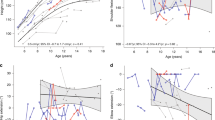
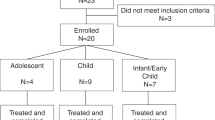
Infantile ceramidase deficiency (Farber disease) is an uncommon, progressive lysosomal storage disease characterized by multiple ceramide-containing nodules (lipogranulomata) in the subcutaneous tissue and upper aerodigestive tract, painful periarticular swelling, psychomotor retardation, and varying degrees of ocular, pulmonary or hepatic involvement. Management of Farber disease has been limited to symptomatic supportive care, and few affected infants survive beyond 5 years of age. We performed an allogeneic bone marrow transplant (BMT) from an HLA-identical heterozygous sister in a 9.5-month-old female with minimally symptomatic Farber disease who received a pre-transplant regimen of busulfan and cyclophosphamide. Ceramidase activity in peripheral blood leukocytes increased from 6% before transplant to 44% (donor heterozygote level) by 6 weeks after BMT. By 2 months after transplant, the patient's subcutaneous lipogranulomata, pain on joint motion, and hoarseness had resolved. Despite modest gains in cognitive and language development, hypotonia and delayed motor skills persisted. Gradual loss of circulating donor cells with autologous hematopoietic recovery occurred; VNTR analyses showed 50% donor DNA in peripheral blood cells at 8.5 months after BMT and only 1% at 21 months after transplant. Interestingly, leukocyte ceramidase activity consistently remained in the heterozygous range despite attrition of donor cells in peripheral blood. This novel observation indicates ongoing hydrolase production by non-circulating donor cells, possibly in the mononuclear phagocytic system, and uptake by recipient leukocytes. Although lipogranulomata and hoarseness did not recur, the patient's neurological and neurocognitive status progressively declined. She died 28 months after BMT (age 37.5 months) with pulmonary insufficiency caused by recurrent aspiration pneumonias. Allogeneic BMT improves the peripheral manifestations of infantile ceramidase deficiency, but may not prevent the progressive neurological deterioration, even when carried out in minimally symptomatic patients. Bone Marrow Transplantation (2000) 26, 357–363.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Sugita M, Dulaney J, Moser HW . Ceramidase deficiency in Farber's disease (lipogranulomatosis) Science 1972 178: 1100–1102
Moser HW . Farber disease (lipogranulomatosis). In: Moser HW (ed) Handbook of Clinical Neurology, vol 22 (66): Neurodystrophies and Neurolipidoses Elsevier Science: Amsterdam 1996 pp211–223
Bernardo K, Hurwitz R, Zenk T et al. Purification, characterization, and biosynthesis of human acid ceramidase J Biol Chem 1995 270: 11098–11102
Koch J, Gartner S, Li CM et al. Molecular cloning and characterization of a full-length complementary DNA encoding human acid ceramidase. Identification of the first molecular lesion causing Farber disease J Biol Chem 1996 271: 33110–33115
Li CM, Park JH, He X et al. The human acid ceramidase gene (ASAH): structure, chromosomal location, mutation analysis, and expression Genomics 1999 62: 223–231
Farber S . A lipid metabolic disorder – disseminated ‘lipogranulomatosis’. A syndrome with similarity to and important differences from Niemann–Pick and Hand–Schüller-Christian disease Am J Dis Child 1952 84: 499–500 (Abstr.)
Farber S, Cohen J, Uzman LL . Lipogranulomatosis. A new lipoglycoprotein storage disease J Mt Sinai Hosp 1957 24: 816–837
Yeager AM . Hematopoietic cell transplantation in storage diseases. In: Blume K, Forman SJ, Thomas ED (eds) Hematopoietic Cell Transplantation, edn2 Blackwell Science: Malden, MA 1999 pp1182–1191
Souillet G, Guiband P, Fensom AH et al. Outcome of displacement bone marrow transplantation in Farber's disease: a report of a case. In: Hobbs JR (ed) Correction of Certain Genetic Diseases by Transplantation COGENT: London 1989 pp137–141
Yeager AM, Wagner JE Jr, Graham ML et al. Optimization of busulfan dosage in children undergoing bone marrow transplantation: a pharmacokinetic study of dose escalation Blood 1992 80: 2425–2428
Scharf SJ, Smith AG, Hansen JA et al. Quantitative determination of bone marrow transplant engraftment using fluorescent polymerase chain reaction primers for human identity markers Blood 1995 85: 1954–1963
Chen TL, Grochow LB, Hurowitz LA, Brundrett RB . Determination of busulfan in human plasma by gas chromatography with electron-capture detection J Chromatogr Biomed Appl 1988 425: 303–309
Grochow LB, Krivit W, Whitley CB, Blazar B . Busulfan disposition in children Blood 1990 75: 1723–1727
Momoi T, Ben-Yoseph Y, Nadler HL . Substrate-specificities of acid and alkaline ceramidases in fibroblasts from patients with Farber disease and controls Biochem J 1982 205: 419–425
Bayley N . Bayley Scales of Infant Development, edn1 Psychological Corporation: New York 1969
Bayley N . Bayley Scales of Infant Development, edn2 Psychological Corporation Harcourt Brace and Company: San Antonio, TX 1993
Sparrow SS, Balla DA, Cicchetti DV . Vineland Adaptive Behavior Scales, Interview Edition (A Revision of the Vineland Social Maturity Scale by Edgar A. Doll) American Guidance Service: Circle Pines, MN 1984
Hamill PVV, Drizd TA, Johnson CL et al. Physical growth: National Center for Health Statistics percentiles Am J Clin Nutr 1979 32: 607–629
Blazar BR, Ramsay NK, Kersey JH et al. Pretransplant conditioning with busulfan (Myleran) and cyclophosphamide for nonmalignant diseases. Assessment of engraftment following histocompatible allogeneic bone marrow transplantation Transplantation 1985 39: 597–603
Hobbs JR, Hugh-Jones K, Shaw PJ et al. Engraftment rates related to busulfan and cyclophosphamide dosages for displacement bone marrow transplants in fifty children Bone Marrow Transplant 1986 1: 201–208
Martin PJ . Overview of marrow transplantation immunology. In: Thomas ED, Blume KG, Forman SJ (eds) Hematopoietic Cell Transplantation, 2nd edn Blackwell Science: Malden, MA 1999 pp19–27
Gale RP, Sparkes RS, Golde DW . Bone marrow origin of hepatic macrophages (Kupffer cells) in humans Science 1978 201: 937–938
Thomas ED, Ramberg RE, Sale GE et al. Direct evidence for a bone marrow origin of the alveolar macrophage in man Science 1976 192: 1016–1018
Bou-Gharios G, Abraham D, Olsen I . Lysosomal storage diseases: mechanisms of enzyme replacement therapy Histochem J 1993 25: 593–605
Perry VH, Gordon S . Macrophages and the nervous system Int Rev Cytol 1991 125: 203–244
Krivit W, Sung JH, Shapiro EG, Lockman LA . Microglia: the effector cell for reconstitution of the central nervous system following bone marrow transplantation for lysosomal and peroxisomal storage diseases Cell Transplant 1995 4: 385–392
Hickey WF, Kimura H . Perivascular microglial cells of the CNS are bone marrow-derived and present antigen in vivo Science 1988 239: 290–292
Kennedy DW, Abkowitz JL . Kinetics of central nervous system microglial and macrophage engraftment: analysis using a transgenic bone marrow transplantation model Blood 1997 90: 986–993
Krall WJ, Challita PM, Perlmutter LS et al. Cells expressing human glucocerebrosidase from a retroviral vector repopulate macrophages and central nervous system microglia after murine bone marrow transplantation Blood 1994 83: 2737–2748
Yeager AM, Shinn C, Hart C, Pardoll DM . Repopulation by donor-derived macrophages in the murine central nervous system (CNS) after congenic bone marrow transplantation (BMT): a quantitative study Blood 1992 80: (Suppl.1) 269a (Abstr.)
Walkley SU, Thrall MA, Dobrenis K et al. Bone marrow transplantation corrects the enzyme defect in neurons of the central nervous system in a lysosomal storage disease Proc Natl Acad Sci USA 1994 91: 2970–2974
Krivit W, Shapiro EG, Lockman LA et al. Bone marrow transplantation treatment for globoid cell leukodystrophy, metachromatic leukodystrophy, adrenoleukodystrophy, and Hurler's syndrome. In: Moser HW (ed) Handbook of Clinical Neurology, Vol22 (66): Neurodystrophies and Neurolipidoses Elsevier Science: Amsterdam 1996 pp87–106
Krivit W, Shapiro EG, Peters C et al. Hematopoietic stem-cell transplantation in globoid-cell leukodystrophy New Engl J Med 1998 338: 1119–1126
Pridjian G, Humbert J, Willis J, Shapira E . Presymptomatic late-infantile metachromatic leukodystrophy treated with bone marrow transplantation J Pediatr 1994 125: 755–758
Zetterström R . Disseminated lipogranulomatosis (Farber's disease) Acta Paediatrica (Scand) 1958 47: 501–510
Samuelsson K, Zetterström R . Ceramides in a patient with lipogranulomatosis (Farber's disease) with chronic course Scand J Clin Lab Invest 1971 27: 393–400
Fiumara A, Nigro F, Pavone L, Moser HW . Farber disease with prolonged survival J Inher Metab Dis 1993 16: 915–916
Acknowledgements
We thank Donald Hutcherson for assistance with determination of busulfan pharmacokinetics, and the nurses at the AFLAC Cancer Center of Children's Healthcare of Atlanta at Egleston and at Scottish Rite for their expert and compassionate care of the patient. This work was supported in part by grant Nos R01 NS24097 and U10 CA20549 from the National Institutes of Health, Bethesda, Maryland, and by the Phil Niekro Beat Leukemia Celebrity Classic/Jill Andrews Leukemia Research Fund, the Andrew McLeroy Memorial Research Fund, the Stott Research Fund, and the Emory-Egleston Children's Research Center.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Yeager, A., Armfield Uhas, K., Coles, C. et al. Bone marrow transplantation for infantile ceramidase deficiency (Farber disease). Bone Marrow Transplant 26, 357–363 (2000). https://doi.org/10.1038/sj.bmt.1702489
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bmt.1702489
Keywords
This article is cited by
-
Sphingolipid lysosomal storage diseases: from bench to bedside
Lipids in Health and Disease (2021)
-
Acid ceramidase, an emerging target for anti-cancer and anti-angiogenesis
Archives of Pharmacal Research (2019)
-
Acid ceramidase deficiency: Farber disease and SMA-PME
Orphanet Journal of Rare Diseases (2018)
-
Deletion of MCP-1 Impedes Pathogenesis of Acid Ceramidase Deficiency
Scientific Reports (2018)
-
Allogeneic hematopoietic cell transplantation in Farber disease
Journal of Inherited Metabolic Disease (2018)