Abstract
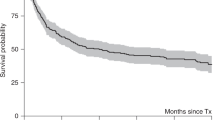
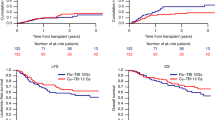
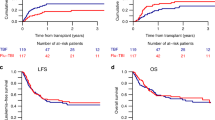
This study was designed to determine the complete response (CR) rate, event-free survival (EFS) and overall survival (OS) in patients with metastatic breast cancer treated with an adriamycin-based induction regimen, high-dose chemotherapy consisting of cyclophosphamide and thiotepa with autologous bone marrow or stem cell reinfusion, followed by post-transplant 5-fluorouracil and cisplatin. Forty-eight consecutive patients were enrolled and 35 received two to four cycles of a cytoreductive chemotherapy regimen followed by high-dose chemotherapy which included cyclophosphamide and thiotepa. Thirty-three patients with non-progressive disease received at least one cycle of post-transplant 5-fluorouracil and cisplatin. Fifty percent of patients with evaluable disease responded to induction chemotherapy. Three of the 34 patients (9%) evaluable for response to high-dose chemotherapy achieved CR, eight (24%) achieved partial response (PR), 12 (35%) had stable disease (SD) and 11 (32%) had progressive disease (PD). The median time to neutrophil recovery was 11.5 days (range, 8 to 40 days) post- reinfusion. The median time to platelet independence was 14.5 days (range, 8 to 44 days). The median follow-up is 24.5 months (range, 1 to 96 months). The actuarial probability of EFS for all patients is 17% at 4 years. The EFS for patients receiving all four cycles of post-transplant chemotherapy is 27% at 4 years, compared to 36% at 1 year for patients not receiving any post-transplant chemotherapy. Ten of the 48 patients (21%) are alive, and seven of these (15%) have no evidence of disease. High-dose chemotherapy with autologous bone marrow or peripheral blood-derived stem cell transplantation followed by post-transplant consolidation chemotherapy in patients with metastatic breast cancer results in a proportion of patients without evidence of disease at 4 years.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Tallman, M., Rademaker, A., Jahnke, L. et al. High-dose chemotherapy, autologous bone marrow or stem cell transplantation and post-transplant consolidation chemotherapy in patients with advanced breast cancer. Bone Marrow Transplant 20, 721–729 (1997). https://doi.org/10.1038/sj.bmt.1700962
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1038/sj.bmt.1700962
Keywords
This article is cited by
-
High-dose chemotherapy and autologous stem cell transplantation as treatment for high-risk breast cancer
Cancer Chemotherapy and Pharmacology (1998)