Abstract
Objective:
To determine the effect on blood pressure of dietary advice to consume a combination of plant-based cholesterol-lowering foods (dietary portfolio).
Methods:
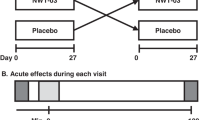
For 1 year, 66 hyperlipidemic subjects were prescribed diets high in plant sterols (1.0 g/1000 kcal), soy protein (22.5 g/1000 kcal), viscous fibers (10 g/1000 kcal) and almonds (22.5 g/1000 kcal). There was no control group. Seven-day diet record, blood pressure and body weight were monitored initially monthly and later at 2-monthly intervals throughout the study.
Results:
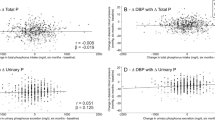
Fifty subjects completed the 1-year study. When the last observation was carried forward for non-completers (n=9) or those who changed their blood pressure medications (n=7), a small mean reduction was seen in body weight 0.7±0.3 kg (P=0.036). The corresponding reductions from baseline in systolic and diastolic blood pressure at 1 year (n=66 subjects) were −4.2±1.3 mm Hg (P=0.002) and −2.3±0.7 mm Hg (P=0.001), respectively. Blood pressure reductions occurred within the first 2 weeks, with stable blood pressures 6 weeks before and 4 weeks after starting the diet. Diastolic blood pressure reduction was significantly related to weight change (r=0.30, n=50, P=0.036). Only compliance with almond intake advice related to blood pressure reduction (systolic: r=−0.34, n=50, P=0.017; diastolic: r=−0.29, n=50, P=0.041).
Conclusions:
A dietary portfolio of plant-based cholesterol-lowering foods reduced blood pressure significantly, related to almond intake. The dietary portfolio approach of combining a range of cholesterol-lowering plant foods may benefit cardiovascular disease risk both by reducing serum lipids and also blood pressure.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Anderson KM, Wilson PW, Odell PM, Kannel WB (1991). An updated coronary risk profile. A statement for health professionals. Circulation 83, 356–362.
Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM et al. (1997). A clinical trial of the effects of dietary patterns on blood pressure. DASH collaborative research group. N Engl J Med 336, 1117–1124.
Appel LJ, Champagne CM, Harsha DW, Cooper LS, Obarzanek E, Elmer PJ, et al., Writing Group of the PREMIER Collaborative Research Group (2003). Effects of comprehensive lifestyle modification on blood pressure control: main results of the PREMIER clinical trial. JAMA 289, 2083–2093.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo Jr JL, et al., National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee (2003). The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA 289, 2560–2572.
Dodson PM (1980). Dietary fibre, sodium, and blood pressure. Br Med J 280, 564.
Dwyer JH, Dwyer KM, Scribner RA, Sun P, Li L, Nicholson LM et al. (1998). Dietary calcium, calcium supplementation, and blood pressure in African American adolescents. Am J Clin Nutr 68, 648–655.
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (2001). Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). JAMA 285, 2486–2497.
Food and Drug Administration Dockets Management 00Q-158 (2000). Health claim notification for potassium containing foods. October 31.
Griffith LE, Guyatt GH, Cook RJ, Bucher HC, Cook DJ (1999). The influence of dietary and nondietary calcium supplementation on blood pressure: an updated metaanalysis of randomized controlled trials. Am J Hypertens 12, 84–92.
Grundy SM, Hansen B, Smith Jr SC, Cleeman JI, Kahn RA, American Heart Association; National Heart, Lung, and Blood Institute; American Diabetes Association (2004). Clinical management of metabolic syndrome: report of the American Heart Association/National Heart, Lung, and Blood Institute/American Diabetes Association conference on scientific issues related to management. Circulation 109, 551–556.
Intersalt: an international study of electrolyte excretion and blood pressure (1988). Results for 24 h urinary sodium and potassium excretion. Intersalt Cooperative Research Group. BMJ 297, 319–328.
Jee SH, Miller III ER, Guallar E, Singh VK, Appel LJ, Klag MJ (2002). The effect of magnesium supplementation on blood pressure: a meta-analysis of randomized clinical trials. Am J Hypertens 15, 691–696.
Jenkins DJ, Kendall CW, Faulkner DA, Kemp T, Marchie A, Wong JM et al. (2006). Assessment of the longer-term effects of a dietary portfolio of cholesterol lowering foods in hypercholesterolemia. Am J Clin Nutr 83, 582–591.
Jenkins DJ, Kendall CW, Jackson CJ, Connelly PW, Parker T, Faulkner D et al. (2002). Effects of high- and low-isoflavone soyfoods on blood lipids, oxidized LDL, homocysteine, and blood pressure in hyperlipidemic men and women. Am J Clin Nutr 76, 365–372.
Jenkins DJ, Kendall CW, Faulkner D, Vidgen E, Trautwein EA, Parker TL et al. (2002). A dietary portfolio approach to cholesterol reduction: Combined effects of plant sterols, vegetable proteins, and viscous fibers in hypercholesterolemia. Metabolism 51, 1596–1604.
Jenkins DJA, Kendall CWC, Marchie A, Faulkner DA, Wong JM, de Souza R et al. (2003). Effects of a dietary portfolio of cholesterol-lowering foods vs lovastatin on serum lipids and C-reactive protein. JAMA 290, 502–510.
Jenkins DJ, Kendall CW, Marchie A, Faulkner DA, Wong JM, de Souza R et al. (2005). Direct comparison of a dietary portfolio of cholesterol-lowering foods with a statin in hypercholesterolemic participants. Am J Clin Nutr 81, 380–387.
Kreijkamp-Kaspers S, Kok L, Bots ML, Grobbee DE, Lampe JW, van der Schouw YT (2005). Randomized controlled trial of the effects of soy protein containing isoflavones on vascular function in postmenopausal women. Am J Clin Nutr 81, 189–195.
Lin PH, Aickin M, Champagne C, Craddick S, Sacks FM, McCarron P, et al., Dash-Sodium Collaborative Research Group (2003). Food group sources of nutrients in the dietary patterns of the DASH-sodium trial. J Am Diet Assoc 103, 488–496.
Resnick LM, Oparil S, Chait A, Haynes RB, Kris-Etherton P, Stern JS et al. (2000). Factors affecting blood pressure responses to diet: the Vanguard study. Am J Hypertens 13, 956–965.
Rivas M, Garay RP, Escanero JF, Cia Jr P, Cia P, Alda JO (2002). Soy milk lowers blood pressure in men and women with mild to moderate essential hypertension. J Nutr 132, 1900–1902.
Sacks FM, Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP et al. (1999). A dietary approach to prevent hypertension: a review of the dietary approaches to stop hypertension (DASH) study. Clin Cardiol 22, III6–III10.
SAS Institute (1997). SAS/STAT User's Guide (ed 6.12). SAS Institute:Cary, NC.
Searle SR (1971). Linear Models. John Wiley and Sons:Boston, MA, 95–96. ISBN 0471769509.
Streppel MT, Arends LR, van't Veer P, Grobbee DE, Geleijnse JM (2005). Dietary fiber and blood pressure: a meta-analysis of randomized placebo-controlled trials. Arch Int Med 165, 150–156.
Svetkey LP, Erlinger TP, Vollmer WM, Feldstein A, Cooper LS, Appel LJ et al. (2005). Effect of lifestyle modifications on blood pressure by race, sex, hypertension status, and age. J Hum Hypertens 19, 21–31.
The Agricultural Research Service (1992). Composition of Foods, Agriculture Handbook No 8. US Department of Agriculture: Washington, DC.
van Mierlo LA, Arends LR, Streppel MT, Zeegers MP, Kok FJ, Grobbee DE et al. (2006). Blood pressure response to calcium supplementation: a meta-analysis of randomized controlled trials. J Hum Hypertens 20, 571–580.
Weinberger MH, Fineberg NS (1991). Sodium and volume sensitivity of blood pressure. Age and pressure change over time. Hypertension 18, 67–71.
Whelton PK, for the TONE Collaborative Research Group (1998). Efficacy of sodium reduction and weight loss in the treatment of hypertension in older persons: main results of the randomized, controlled trial of nonpharmacologic interventions in the elderly (TONE). JAMA 279, 839–846.
Acknowledgements
This work is supported by the Canada Research Chair Endowment of the Federal Government of Canada; the Canadian Natural Sciences and Engineering Research Council of Canada; Loblaw Brands Limited; the Almond Board of California; Unilever Canada and Unilever Research & Development, Vlaardingen, The Netherlands.
We thank Ms Kathy Galbraith of Natural Temptations Bakery, Burlington, ON, Canada for her assistance on this project; and to the study participants for their attention to detail and enthusiasm.
Author information
Authors and Affiliations
Corresponding author
Additional information
Contributors: DJAJ, CWCK and DAF contributed to study concept and design; DJAJ, CWCK, DAF, TK, AM, THN, JMWW, RdS, AE and EV contributed to acquisition of data; DJAJ, CWCK, TK, RGJ, LAL and WS contributed to analysis and interpretation of data; DJAJ and CWCK contributed to drafting of the manuscript; DJAJ, CWCK, DAF, AM, THN, JMWW, RdS, AE, EV, EAT, KGL, RGJ, LAL and WS contributed to critical revision of the manuscript for important intellectual content; EV contributed to statistical expertise; DJAJ and CWCK contributed to obtaining funding; CWCK, DAF, AM, THN, JMWW, RdS, AE, EAT, KGL, RGJ, LAL and WS contributed to administrative, technical or material support; DJAJ, CWCK and DAF study supervision.
Rights and permissions
About this article
Cite this article
Jenkins, D., Kendall, C., Faulkner, D. et al. Long-term effects of a plant-based dietary portfolio of cholesterol-lowering foods on blood pressure. Eur J Clin Nutr 62, 781–788 (2008). https://doi.org/10.1038/sj.ejcn.1602768
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ejcn.1602768
Keywords
This article is cited by
-
Dietary phytosterols and phytostanols decrease cholesterol levels but increase blood pressure in WKY inbred rats in the absence of salt-loading
Nutrition & Metabolism (2010)
-
Macronutrients, Weight Control, and Cardiovascular Health: A Systematic Review
Current Cardiovascular Risk Reports (2010)
-
The portfolio diet for cardiovascular risk reduction
Current Atherosclerosis Reports (2007)