Abstract
Objective:
Most research on constipation has focused on dietary fiber intake. Here, we examined the intake of water and magnesium, nutrients possibly associated with constipation, as well as that of dietary fiber in relation to constipation.
Design:
Cross-sectional study.
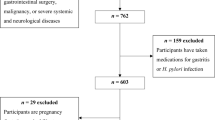
Subjects:
A total of 3835 female Japanese dietetic students aged 18–20 years from 53 institutions in Japan.
Methods:
Dietary intake was estimated with a validated, self-administered diet history questionnaire. Functional constipation was defined using the Rome I criteria.
Results:
The prevalence of functional constipation was 26.2%. Neither dietary fiber intake (mean=6.4 g/4186 kJ) nor intakes of total water and water from fluids were associated with constipation. Conversely, low intake of water from foods was associated with an increasing prevalence of constipation. In comparison with women in the first (lowest) quintile, the multivariate adjusted odds ratio (OR) (95% confidence interval (CI)) for women in the second, third, fourth, and fifth quintiles were 0.72 (0.57, 0.90), 0.78 (0.62, 0.98), 0.71 (0.56, 0.89), and 0.77 (0.61, 0.97), respectively (P for trend=0.04). Additionally, low magnesium intake was associated with increasing prevalence of constipation. Compared with women in the first quintile, the multivariate adjusted OR (95% CI) for women in the second, third, fourth and fifth quintiles were 0.70 (0.56, 0.88), 0.75 (0.60, 0.95), 0.73 (0.58, 0.92) and 0.79 (0.63, 0.996), respectively (P for trend=0.09).
Conclusions:
Low intakes of water from foods and magnesium are independently associated with an increasing prevalence of functional constipation among a population whose dietary fiber intake is relatively low.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Ainsworth BE, Haskell WL, Leon AS, Jacobs Jr DR, Montoye HJ, Sallis JF et al. (1993). Compendium of physical activities: classification of energy costs of human physical activities. Med Sci Sports Exerc 25, 71–80.
Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ et al. (2000). Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc 32 (Suppl 9), S498–S504.
Anti M, Pignataro G, Armuzzi A, Valenti A, Iascone E, Marmo R et al. (1998). Water supplementation enhances the effect of high-fiber diet on stool frequency and laxative consumption in adult patients with functional constipation. Hepatogastroenterology 45, 727–732.
Arnaud MJ (2003). Mild dehydration: a risk factor of constipation? Eur J Clin Nutr 57 (Suppl 2), S88–S95.
Black AE, Coward WA, Cole TJ, Prentice AM (1996). Human energy expenditure in affluent societies: an analysis of 574 doubly-labelled water measurements. Eur J Clin Nutr 50, 72–92.
Campbell AJ, Busby WJ, Horwath CC (1993). Factors associated with constipation in a community based sample of people aged 70 years and over. J Epidemiol Community Health 47, 23–26.
Chung BD, Parekh U, Sellin JH (1999). Effect of increased fluid intake on stool output in normal healthy volunteers. J Clin Gastroenterol 28, 29–32.
Dukas L, Willett WC, Giovannucci EL (2003). Association between physical activity, fiber intake, and other lifestyle variables and constipation in a study of women. Am J Gastroenterol 98, 1790–1796.
Garrigues V, Galvez C, Ortiz V, Ponce M, Nos P, Ponce J (2004). Prevalence of constipation: agreement among several criteria and evaluation of the diagnostic accuracy of qualifying symptoms and self-reported definition in a population-based survey in Spain. Am J Epidemiol 159, 520–526.
Higgins PD, Johanson JF (2004). Epidemiology of constipation in North America: a systematic review. Am J Gastroenterol 99, 750–759.
Klauser AG, Beck A, Schindlbeck NE, Muller-Lissner SA (1990). Low fluid intake lowers stool output in healthy male volunteers. Z Gastroenterol 28, 606–609.
Livingstone MBE, Black AE (2003). Markers of the validity of reported energy intake. J Nutr 133 (Suppl 3), 895S–920S.
Locke III GR, Pemberton JH, Phillips SF (2000). AGA technical review on constipation. American Gastroenterological Association. Gastroenterology 119, 1766–1778.
Matsuzawa Y, Inoue S, Ikeda Y, Sakata T, Saito Y, Sato Y et al. (2000). The judgment criteria for new overweight, and the diagnostic standard for obesity. Obes Res 6, 18–28. (in Japanese).
Ministry of Health, Labour, and Welfare (2004). The National Nutrition Survey in Japan, 2002. Daiichi Shuppan Publishing Co., Ltd: Tokyo (in Japanese).
Ministry of Health, Labour, and Welfare (2005). Dietary Reference Intakes for Japanese, 2005. Daiichi Shuppan Publishing Co., Ltd: Tokyo (in Japanese).
Muller-Lissner SA, Kamm MA, Scarpignato C, Wald A (2005). Myths and misconceptions about chronic constipation. Am J Gastroenterol 100, 232–242.
Murakami K, Okubo H, Sasaki S (2006). Dietary intake in relation to self-reported constipation among Japanese women aged 18–20 years. Eur J Clin Nutr 60, 650–657.
Ohya Y, Yoneda Y (1995). Relationship between constipation and food intake and eating habits consciousness. Jpn J Nutr 53, 385–394 (in Japanese with English abstract).
Pare P, Ferrazzi S, Thompson WG, Irvine EJ, Rance L (2001). An epidemiological survey of constipation in Canada: definitions, rates, demographics, and predictors of health care seeking. Am J Gastroenterol 96, 3130–3137.
Saez LR (1991). Therapeutic proposals for the treatment of idiopathic constipation. Ital J Gastroent 23, 30–35.
Sanjoaquin MA, Appleby PN, Spencer EA, Key TJ (2004). Nutrition and lifestyle in relation to bowel movement frequency: a cross-sectional study of 20 630 men and women in EPIC-Oxford. Public Health Nutr 7, 77–83.
Sasaki S, Ushio F, Amano K, Morihara M, Todoriki T, Uehara Y et al. (2000). Serum biomarker-based validation of a self-administered diet history questionnaire for Japanese subjects. J Nutr Sci Vitaminol 46, 285–296.
Sasaki S, Yanagibori R, Amano K (1998a). Self-administered diet history questionnaire developed for health education: a relative validation of the test-version by comparison with 3-day diet record in women. J Epidemiol 8, 203–215.
Sasaki S, Yanagibori R, Amano K (1998b). Validity of a self-administered diet history questionnaire for assessment of sodium and potassium: comparison with single 24-h urinary excretion. Jpn Circ J 62, 431–435.
Science and Technology Agency (2000). Standard Tables of Food Composition in Japan,5th edn, Printing Bureau of the Ministry of Finance: Tokyo (in Japanese).
Talley NJ (2004). Definitions, epidemiology, and impact of chronic constipation. Rev Gastroenterol Disord 4 (Suppl 2), S3–S10.
Thompson WG, Longstreth GF, Drossman DA, Heaton KW, Irvine EJ, Muller-Lissner SA (1999). Functional bowel disorders and functional abdominal pain. Gut 4 (Suppl 2), II43–II47.
Towers AL, Burgio KL, Locher JL, Merkel IS, Safaeian M, Wald A (1994). Constipation in the elderly: influence of dietary, psychological, and physiological factors. J Am Geriatr Soc 42, 701–706.
Whitehead WE, Chaussade S, Corazziari E, Kumar D (1991). Report of an international workshop on management of constipation. Gastroenterol Int 4, 99–113.
Wong ML, Wee S, Pin CH, Gan GL, Ye HC (1999). Sociodemographic and lifestyle factors associated with constipation in an elderly Asian community. Am J Gastroenterol 94, 1283–1291.
Young RJ, Beerman LE, Vanderhoof JA (1998). Increasing oral fluids in chronic constipation in children. Gastroenterol Nurs 21, 156–161.
Acknowledgements
We thank the students for their generous participation in the study. The members of the Freshmen in Dietetic Courses Study II Group (in addition to the authors) are as follows (shown in alphabetical order of the affiliation): S Awata (Beppu University); T Watanabe and A Suzuki (Chiba College of Health Science); T Abe (Doshisha Women's College); H Hayabuchi (Fukuoka Women's University); R Ueda (Futaba Nutrition College); N Takeda and T Matsubara (Hiroshima Bunkyo Women's University); H Ohwada and K Hirayama (Ibaraki Christian University); C Maruyama (Japan Women's University); M Makino (Jin-ai Women's College); S Tanaka and N Nagasawa (Jumonji University); F Tonozuka and S Osada (Junior College of Kagawa Nutrition University); K Uenishi (Kagawa Nutrition University); T Sagara (Kanazawa Gakuin College); Y Enomoto, K Okayama and H Ooe (Kitasato Junior College of Health and Hygienic Sciences); K Nakayama and M Furuya (Kochi Gakuen College); N Yagi and K Soeda (Koshien University); J Ikeda (Kyoto Bunkyo Junior College); I Kitagawa (Kyoto Koka Women's University); K Yokoyama and R Nakayama (Kyoto Women's University); A Miura (Kwassui Women's College); K Baba (Mie Chukyo University Junior College); Y Sugiyama and M Furuki (Minami Kyushu University); T Oyama (Miyagi Gakuin Women's University); Y Naito and M Kato (Mukogawa Women's University); N Hirota (Nagano Prefectural College); T Tsuji and K Washino (Nagoya Bunri University); T Yawata and C Shimamura (Nara Saho College); N Murayama (Niigata University of Health and Welfare); R Watanabe (Niigata Women's College); M Yamasaki (Nishikyusyu University); M Kitamura (Osaka Aoyama College); T Iwamoto (Prefectural University of Hiroshima); I Suzuki and Y Sugishima (Prefectural University of Kumamoto); M Aoki (Sanyo Gakuen College); S Nishi (Seibo Jogakuin Junior College); K Toyama and R Amamoto (Seinan Jo Gakuin University); N Takahashi and R Sasaki (Sendai Shirayuri Women's College); N Kakibuchi (Setouchi Junior College); M Goto (Shokei Gakuin College); M Watanabe and M Yokotsuka (Showa Women's University); M Kimura (Takasaki University of Health and Welfare); M Hara and N Kiya (Tenshi College); J Hirose, T Fukui and K Shibata (The University of Shiga Prefecture); R Nishiyama (Toita Women's College); N Tomita (Tokiwa Junior College); J Oka and T Ide (Tokyo Kasei University); T Uemura and T Furusho (Tokyo University of Agriculture); A Notsu and Y Yokoyama (Tottori College); T Kuwamori (Toyama College); S Shirono (Ube Frontier College); T Goda (University of Shizuoka); K Suizu (Yamaguchi Prefectural University); H Okamoto (Yamanashi Gakuin Junior College).
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Guarantor: S Sasaki.
Contributors: KM was involved in the study designing, data collection and data management; created a constipation questionnaire, conducted the statistical analyses and wrote the manuscript. SS was responsible for the study designing, data collection, data management, and the overall management, and assisted in the manuscript preparation. HO was involved in the study designing. YT assisted in the manuscript preparation. YH was involved in the study designing, data collection and data management. MI was involved in data collection and data management. All the authors provided suggestions during the preparation of the manuscript and approved the final version submitted for publication.
Rights and permissions
About this article
Cite this article
Murakami, K., Sasaki, S., Okubo, H. et al. Association between dietary fiber, water and magnesium intake and functional constipation among young Japanese women. Eur J Clin Nutr 61, 616–622 (2007). https://doi.org/10.1038/sj.ejcn.1602573
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ejcn.1602573
Keywords
This article is cited by
-
Nutraceuticals and biotics in pediatric gastrointestinal disorders
European Journal of Clinical Nutrition (2024)
-
Evaluating the risk factors for the development of benign disorders of defaecation: a surgical perspective
Techniques in Coloproctology (2023)
-
Empirically derived dietary patterns and constipation among a middle-aged population from China, 2016–2018
Nutrition Journal (2019)
-
Dietary phosphorus intake estimated by 4-day dietary records and two 24-hour urine collections and their associated factors in Japanese adults
European Journal of Clinical Nutrition (2018)
-
Higher dietary acid load is associated with a higher prevalence of frailty, particularly slowness/weakness and low physical activity, in elderly Japanese women
European Journal of Nutrition (2018)