Abstract
Objective: To study the prevalence of vitamin D deficiency and to identify possible predictors of vitamin D deficiency in five main immigrant groups in Oslo.
Design: Cross-sectional, population-based.
Setting: City of Oslo.
Subjects: In total, 491 men and 509 women with native countries Turkey, Sri Lanka, Iran, Pakistan and Vietnam living in the county of Oslo.
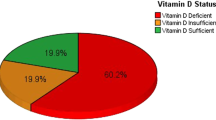
Results: Median serum 25(OH)D level (s-25(OH)D) was 28 nmol/l, ranging from 21 nmol/l in women born in Pakistan to 40 nmol/l in men born in Vietnam. Overall prevalence of vitamin D deficiency defined as s-25(OH)D<25 nmol/l was 37.2%, ranging from 8.5% in men born in Vietnam to 64.9% in women born in Pakistan. s-25(OH)D did not vary significantly with age. s-25(OH)D was higher in blood samples drawn in June compared to samples obtained in April, but not significantly for women. Reported use of fatty fish and cod liver oil supplements showed a strong positive association with s-25(OH)D in all groups. Education length was positively associated with s-25(OH)D in women, whereas body mass index (BMI) was inversely associated with s-25(OH)D in women. These two variables were not related to vitamin D deficiency in men.
Conclusions: There is widespread vitamin D deficiency in both men and women born in Turkey, Sri Lanka, Iran, Pakistan and Vietnam residing in Oslo. The prevalence of vitamin D deficiency is higher in women than in men, and it is higher in those born in Pakistan and lower in those born in Vietnam compared to the other ethnic groups. Fatty fish intake and cod liver oil supplements are important determinant factors of vitamin D status in the groups studied. BMI and education length are also important predictors in women.
Sponsorship: Supported by the Directorate for Health and Social Affairs, Oslo, and Research Forum, Aker University Hospital, Oslo.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Bell NH, Epstein S, Greene A, Shary J, Oexmann MJ & Shaw S (1985): Evidence for alteration of the vitamin D–endocrine system in obese subjects. J. Clin. Invest. 76, 370–373.
Brunvand L & Brunvatne R (2001): Helseproblemer blant innvandrerbarn i Norge. Tidsskr. Nor. Lægeforen. 121, 715–718.
Brunvand L & Haug E (1993): Vitamin D deficiency amongst Pakistani women in Oslo. Acta Obstet. Gynecol. Scand. 72, 264–268.
Brunvand L, Henriksen C & Haug E (1996): Vitamin D mangel blant gravide fra Pakistan. Hvordan best forebygge? Tidsskr. Nor. Lægeforen. 116, 1585–1587.
Brunvand L & Nordshus T (1996): Alimentær rakitt. En gammel sykdom med ny aktualitet. Nord. Med. 111, 219–221.
Brustad M, Sandanger T, Wilsgaard T, Aksnes L & Lund E (2003): Change in plasma levels of vitamin D after consumption of cod-liver and fresh cod-liver oil as part of the traditional north Norwegian fish dish ‘Mølje’. Int. J. Circumpolar Health 62, 40–53.
Datta S, Alfaham M, Davies DP, Dunstan F, Woodhead S, Evans J & Richards B (2002): Vitamin D deficiency in pregnant women from a non-European ethnic minority population—an interventional study. Br. J. Obstet. Gynaecol. 109, 905–908.
Davies PS, Bates CJ, Cole TJ, Prentice A & Clarke PC (1999): Vitamin D: seasonal and regional differences in preschool children in Great Britain. Eur. J. Clin. Nutr. 53, 195–198.
Dawodu A, Absood G, Patel M, Agarwal M, Ezimokhai M, Abdulrazzaq Y & Khalayli G (1998): Biosocial factors affecting vitamin D status of women of childbearing age in the United Arab Emirates. J. Biosoc. Sci. 30, 431–437.
DeLucia MC, Mitnick ME & Carpenter TO (2003): Nutritional rickets with normal circulating 25-hydroxyvitamin D: a call for reexamining the role of dietary calcium intake in North American infants. J. Clin. Endocrinol. Metab. 88, 3539–3545.
Falch JA & Steihaug S (2000): Vitamin D deficiency in Pakistani premenopausal women living in Norway is not associated with evidence of reduced skeletal strength. Scand. J. Clin. Lab. Invest. 60, 103–109.
Glerup H, Mikkelsen K, Poulsen L, Hass E, Overbeck S, Thomsen J, Charles P & Eriksen EF (2000): Commonly recommended daily intake of vitamin D is not sufficient if sunlight exposure is limited. J. Intern. Med. 247, 260–268.
Hamson C, Goh L, Sheldon P & Samanta A (2003): Comparative study of bone mineral density, calcium, and vitamin D status in the Gujarati and white populations of Leicester. Postgrad. Med. J. 79, 279–283.
Henriksen C, Brunvand L, Stoltenberg C, Trygg K, Haug E & Pedersen JI (1995): Diet and vitamin D status among pregnant Pakistani women in Oslo. Eur. J. Clin. Nutr. 49, 211–218.
Holick MF (1995): Environmental factors that influence the cutaneous production of vitamin D. Am. J. Clin. Nutr. 61, 638S–645S.
Holick MF (2003): Vitamin D: a millenium perspective. J. Cell. Biochem. 88, 296–307.
Iqbal SJ, Featherstone S, Kaddam IM, Mortimer J & Manning D (2001): Family screening is effective in picking up undiagnosed Asian vitamin D deficient subjects. J. Hum. Nutr. Diet. 14, 371–376.
Isaia G, Giorgino R, Rini GB, Bevilacqua M, Maugeri D & Adami S (2003): Prevalence of hypovitaminosis D in elderly women in Italy: clinical consequences and risk factors. Osteoporos. Int. 14, 577–582.
Jacques PF, Felson DT, Tucker KL, Mahnken B, Wilson PW, Rosenberg IH & Rush D (1997): Plasma 25-hydroxyvitamin D and its determinants in an elderly population sample. Am. J. Clin. Nutr. 66, 929–936.
Lips P (2001): Vitamin D deficiency and secondary hyperparathyroidism in the elderly: consequences for bone loss and fractures and therapeutic implications. Endocr. Rev. 22, 477–501.
Meyer HE, Falch JA, Søgaard AJ & Haug E (2004): Vitamin D deficiency & secondary hyperparathyroidism and the association with bone mineral density in persons with Pakistani and Norwegian background living in Oslo, Norway. The Oslo Health Study. Bone 35, 412–417.
Pedersen P, Michaelsen KF & Molgaard C (2003): Children with nutritional rickets referred to hospitals in Copenhagen during a 10-year period. Acta Paediatr. 92, 87–90.
Semba RD, Garrett E, Johnson BA, Guralnik JM & Fried LP (2000): Vitamin D deficiency among older women with and without disability. Am. J. Clin. Nutr. 72, 1529–1534.
Serhan E, Newton P, Ali HA, Walford S & Singh BM (1999): Prevalence of hypovitaminosis D in Indo-Asian patients attending a rheumatology clinic. Bone 25, 609–611.
Shaw NJ & Pal BR (2002): Vitamin D deficiency in UK Asian families: activating a new concern. Arch. Dis. Child. 86, 147–149.
Statistics Norway (2003): Innvandring og innvandrere 2003. Statistics Norway website. www.ssb.no.
Søgaard AJ, Selmer R, Bjertness E & Thelle D (2004): The Oslo Health Study: The impact of self-selection in a large population-based survey. Int. J. Equity Health 3, 3.
Wilkinson RJ, Llewelyn M, Toossi Z, Patel P, Pasvol G, Lalvani A, Wright D, Latif M & Davidson RN (2000): Influence of vitamin D deficiency and vitamin D receptor polymorphisms on tuberculosis among Gujarati Asians in west London: a case–control study. Lancet 355, 618–621.
Wortsman J, Matsuoka LY, Chen TC, Lu Z & Holick MF (2000): Decreased bioavailability of vitamin D in obesity. Am. J. Clin. Nutr. 72, 690–693.
Acknowledgements
The data collection was conducted as part of the Oslo Immigrant Health Study carried out in 2002 as a collaboration between the Norwegian Institute of Public Health and the University of Oslo.
Author information
Authors and Affiliations
Corresponding author
Additional information
Guarantor: K Holvik.
Contributors: KH performed the data analysis and prepared the manuscript with HM, who was also a responsible organizer of the Oslo Immigrant Health Study. EH was responsible for the blood sample analyses. LB initiated the vitamin D substudy, and contributed to the design of the paper. All coauthors have critically revised and approved the manuscript.
Rights and permissions
About this article
Cite this article
Holvik, K., Meyer, H., Haug, E. et al. Prevalence and predictors of vitamin D deficiency in five immigrant groups living in Oslo, Norway: the Oslo Immigrant Health Study. Eur J Clin Nutr 59, 57–63 (2005). https://doi.org/10.1038/sj.ejcn.1602033
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ejcn.1602033
Keywords
This article is cited by
-
Serum vitamin D levels in Berliners of Turkish descent –a cross-sectional study
BMC Public Health (2019)
-
A Comparison Study of Vitamin D Deficiency among Older Adults in China and the United States
Scientific Reports (2019)
-
Vitamin D deficiency was common in all patients at a Swedish primary care centre, but more so in patients born outside of Europe
Journal of Public Health (2018)
-
Vitamin D deficiency and supplementation in pregnancy in a multiethnic population-based cohort
BMC Pregnancy and Childbirth (2016)
-
Risk factors for antenatal hypovitaminosis D in an urban district in Malaysia
BMC Pregnancy and Childbirth (2016)