Abstract
Several expert committees recommend a high fluid intake in patients with chronic bronchitis and asthma. Is there a relationship between fluid intake or hydration status and broncho-pulmonary disorders like bronchitis and asthma?
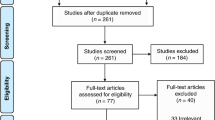
First, basic physiologic mechanisms like regulation of lung fluid balance and water transport at pulmonary surfaces were analyzed, in order to characterize the role of local hydration status in lung and airways. Second, making use of the computer-based literature searches (PubMed), evidence for a role of hydration status in complex physiological and pathophysiological conditions of lungs and airways like perinatal lung adaptation (PLA) (in prematures), mucociliary clearance(MC) and asthma was categorized.
The movement of fluid between the airspaces, interstitium, and vascular compartments in the lungs plays an important physiological role in the maintenance of hydration and protection of the lung epithelium and significantly contributes to a proper airway clearance.
PLA is characterized by a rapid change from fluid secretion to fluid absorption in the distal respiratory tract, with the literature data confirming a critical role of the epithelial sodium channel. Only few studies have investigated the effect of different fluid input regimens on PLA in prematures. MC relies on the interaction between epithelial water fluxes, mucus secretions, and ciliary activity. Whereas animal data show that drying of the airway epithelium decreases MC, few clinical studies investigating the effect of local or systemic hydration on MC have led to ambiguous results. Asthma (A) is characterized by chronic airway inflammation and episodic airway obstruction. Data in animals and humans indicate an association between exercise-induced-A and conditioning (humidity and heat exchange) of inspired air. However, epidemiological studies (children and adults), investigating the role of fluid (and salt) input in the etiology of the disease as well as studies analyzing different markers of hydration status during asthmatic attacks have so far led to conflicting results. Some expert groups recommend sufficient hydration as a complementary A-therapy.
Analysis of basic physiological mechanisms in lungs and airways clearly demonstrates a critical role for water transport and local hydration status. In broncho-pulmonary diseases, however, analysis of the complex pathophysiological mechanisms is difficult. Thus, we still need more studies to confirm or refute mild dehydration or hypohydration as a risk factor of broncho-pulmonary disorders.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Anderson SD & Daviskas E (2000): The mechanism of exercise induced asthma is … J. Allergy Clin. Immunol. 106, 453–459.
Ardern KD & Ram FSF (2001): Dietary salt reduction or exclusion for allergic asthma (Cochrane review). In The Cochrane Library. vol. 4. Oxford: Updated Software.
Bahna SL & Kaushik SP (1984): Water and electrolyte status in children with acute asthma. J. Asthma 21, 73–79.
Baines DL, Folkesson HG, Norlin A, Bingle CD, Yuan HT & Olver RE (2000): The influence of mode of delivery, hormonal status and postnatal O2 environment on epithelial sodium channel (EnaC) expression in perinatal guinea-pig lung. J. Physiol. 522, 147–157.
Bar-Or O, Neumann I & Dotan R (1977): Effects of dry and humid climates on exercise-induced asthma in children and preadolescents. J. Allergy Clin. Immunol. 60, 163–168.
Boucher RC (1994a): Human airway ion transport. Part one. Am. J. Respir. Crit. Care. Med. 150, 271–281.
Boucher RC (1994b): Human airway ion transport. Part two. Am. J. Respir. Crit. Care Med. 150, 581–593.
Barker PM, Nguyen MS, Gatzy JT, Grubb B, Norman H, Hummler E, Rossier B, Boucher RC & Koller B (1998): Role of the ãENaC subunit in lung liquid clearance and electrolyte balance in newborn mice. J. Clin. Invest. 102, 1634–1640.
Bauer J, Beedgen B, Bohler T, Sontheimer D, Zilow EP & Linderkamp O (1996): Bronchopulmonary dysplasia. Retrospective analysis of various forms of treatment and development of a staged therapeutic plan. Klin. Pädiatr. 208, 56–60.
Bell EF & Acarregui MJ (2001): Restricted versus liberal water intake for preventing morbidity and mortality in preterm infants (Cochrane review). In The Cochrane Library. Vol. 4. Oxford: Updated Software.
Bland RD (1997): Fetal lung liquid and its removal near birth. In The lung. Scientific Foundations. 2nd Edition, eds RG Crystal & JB West, pp 2115–2128. Philadelphia: Lippincott-Raven Publishers.
Burri PH (1997): Postnatal development and growth. In The Lung. Scientific Foundations. 2 nd Edition, eds RG Crystal & JB West, pp 573–584. Philadelphia: Lippincott-Raven Publishers.
Canessa CM, Horisberger JD & Rossier BC (1993): Functional cloning of the epithelial sodium channel: relation with genes involved in neurodegeneration. Nature 361, 467–470.
Canessa CM, Schild L, Buell G, Thorens B, Gautschi I, Horisberger JD & Rossier BC (1994): Amiloride-sensitive epithelial Na+ channel is made of three homologous subunits. Nature 367, 463–467.
Culver BH (1999): Physiology. In Comprehensive Respiratory Medicine. eds R Albert, S Spiro & J Jett, pp 41.1–41.42. London: Mosby.
Dawson KP, Mann DW, Fergusson DM & Sadler WA (1984): The antidiuretic hormone response to therapy for acute asthma. Aust. Paediatr. J. 20, 323–324.
Defebach ME, Nirmal B, Lakshminarayan S & Butler J (1987): The bronchial circulation. Am. Rev. Respir. Dis. 135, 463–481.
Freed AN, Taskar V, Schofild B & Omori C (1996): Effect of furosemide on hyperpnea-induced airway obstruction, injury, and microvascular leakage. J. Appl. Physiol. 81, 2461–2467.
Gabriel SE & Boucher RC (1997): Ion channels. In The Lung. Scientific Foundations. 2nd Edition, eds. RG Crystal, JB West, pp 305–318. Philadelphia: Lippincott-Raven Publishers.
Gilbert IA, Winslow CJ, Lenner KA, Nelson JA & McFadden ER (1993): Vascular volume expansion and thermally induced asthma. Eur. Respir. J. 6, 189–197.
Gopalan AV, Govindan UT & Govindaraj M (1983): Asthma and chronic bronchitis: contrasting changes in body weight and hematocrit values during recovery from acute episodes. J. Asthma 20, 53–55.
Green J & Britton N (1998): Qualitative research and evidence based medicine. B. M. J. 316, 1230–1234.
Häussinger D, Roth E, Lang F & Gerok W (1993): Cellular hydration state: an important determinant of protein catabolism in health and disease. Lancet II, 1330–1332.
Houtmeyers E, Gosselink R, Gayan-Ramirez G & Decramer M (1999): Regulation of mucociliary clearance in health and disease. Eur. Respir. J. 13, 1177–1188.
Hummler E & Horiberger JD (1999): Genetic disorders of membrane transport V. The epithelial sodium channel and its implication in human diseases. Am. J. Physiol. 276, 567–571.
Kavvadia V, Greenough A, Dimitriou G & Hooper R (1999): Comparison of the effect of two fluid input regimens on perinatal lung function in ventilated infants of very low birthweight. Eur. J. Pediatr. 158, 917–922.
King LS & Agre P (1996): Pathophysiology of the aquaporin water channels. Annu. Rev. Physiol. 56, 619–648.
King LS & Agre P (2000): Aquaporins and the respiratory system: advice for a lung investigator. J. Clin. Invest. 105, 15–16.
Kleiner S (1999): Water: an essential but overlooked nutrient. J. Am. Diet. Assoc. 99, 200–206.
Lang F, Busch GL, Ritter M, Volkl H, Waldegger S, Gulbins E & Häussinger D (1998): Functional significance of cell volume regulatory mechanism. Physiol. Rev. 78, 247–306.
Marchette LC, Marchette BE, Abraham WM & Wanner A (1985): The effect of systemic hydration on normal and impaired mucociliary function. Pediatr. Pulmonol. 1, 107–111.
Matalon S & O'Brodovich H (1999): Sodium channels in alveolar epithelial cells. Annu. Rev. Physiol. 61, 627–661.
Matsui H, Randell SH, Peretti SW, Davis W & Boucher RC (1998): Coordinated clearance of periciliary liquid and mucus from airway surfaces. J. Clin. Invest. 102, 1125–1131.
Matthay MA, Folkesson HG & Verkman AS (1996): Salt and water transport across alveolar and distal airway epthelia in the adult lung. Am. J. Physiol. 270, 487–503.
McFadden ER (1997): Airway function: regulation by physical factors. In The Lung. Scientific Foundations. 2nd Edition, RG Crystal & West, pp 487–503. Philadelphia: Lippincott-Raven Publishers.
McFadden ER & Gilbert IA (1994): Exercise-induced asthma. N. Engl. J. Med. 330, 1362–1367.
National Heart, Lung, and Blood Institute (1997): Guidelines for the Diagnosis and Management of Asthma (Expert Panel Report 2). U.S. Department of Health and Human Services (Pub no 97-4051), p 116. Bethesda: National Institutes of Health.
O'Brodovich HM (1997): Respiratory distress syndrome: the importance of effective transport. J. Pediatr. 130, 342–344.
Paré PD, Yager DC & Godden DJ (1997): Airway edema. In The Lung. Scientific Foundations. 2nd Edition, eds. RG Crystal & JB West, pp 1355–1364. Philadelphia: Lippincott-Raven Publishers.
Partridge MR (1999): Asthma: clinical features, diagnosis, and treatment. In Comprehensive Respiratory Medicine. eds R Albert, S Spiro & J Jett, pp 41.1–41.41. London: Mosby.
Postma DS, Kerstjens AM & Ten Hacken NHT (1999): Asthma: epidemiology and risk factors. In Comprehensive respiratory medicine. eds. R Albert, S Spiro & J Jett, pp 401–408. London: Mosby.
Sachdeva A, Sachdeva OP, Gulati SP & Kakkar V (1993): Nasal mucociliary clearance and mucus pH in patients with diabetes mellitus. Indian J. Med. Res. 98, 265–268.
Salah B, Dinh Xuan AT, Fouilladieu JL, Lockhart A & Regnard J (1988): Nasal mucociliary transport in healthy subjects is slower when breathing dry air. Eur. Respir. J. 1, 852–855.
Shim C, King M & Williams MH (1987): Lack of effect of hydration on sputum production in chronic bronchitis. Chest 92, 679–682.
Singleton R, Moel DI & Cohn RA (1986): Preliminary observation of impaired water excretion in treated status asthmaticus. Am. J. Dis. Child. 140, 59–61.
Smith DE, Otulakowski G, Yeger H, Post M, Cutz E & O'Brodovich (2000): Epithelial Na+ Channel (EnaC) expression in the developing normal and abnormal human perinatal lung. Am. J. Respir. Crit. Care Med. 161, 1322–1331.
Song Y, Jayaraman S, Yang B, Matthay MA & Verkman AS (2001): Role of aquaporin water channels in airway fluid transport, humidification, and surface liquid hydration. J. Gen. Physiol. 117, 573–582.
Song Y, Fukuda N, Bai C, Ma T, Matthay MA & Verkman AS (2000): Role of aquaporins in alveolar fluid clearance in neonatal and adult lung, and in oedema formation following acute lung injury: studies in transgenic aquaporin null mice. J. Physiol. 525, 771–779.
Taburet AM & Schmit B (1994): Pharmacokinetic optimisation of asthma treatment. Clin. Pharmacokin. 26, 396–418.
Taylor AE, Khimenko PL, Moore TM & Adkins WK (1997): Fluid balance. In The Lung. Scientific Foundations. 2nd Edition, eds. RG Crystal & JB West, pp 1549–1566. Philadelphia: Lippincott-Raven Publishers.
van Os CH, Kamsteeg E-J, Marr N & Deen PMT (2000): Physiological relevance of aquaporins: luxury of necessity? Pflügers Arch.—Eur. J. Physiol. 440, 513–520.
Van Schoor J, Joos GF & Pauwels RA (2000): Indirect bronchial hyperresponsiveness in asthma: mechanisms, pharmacology and implications for clinical research. Eur. Respir. J. 16, 514–533.
Verkman AS (1998): Role of aquaporin water channels in kidney and lung. Am. J. Med. Sci. 316, 310–320.
Wagner EM (1997): Bronchial circulation. In The Lung. Scientific Foundations. 2nd Edition, eds. RG Crystal & JB West, pp 1093–1105. Philadelphia: Lippincott-Raven Publishers.
Wang X, Zhang Y, Amberson A & Engelhardt JF (2001): New models of the tracheal airway define the glandular contribution to airway surface fluid and electrolyte composition. Am. J. Respir. Cell. Mol. Biol. 24, 195–202.
Wanner A, Salathé M & O'Riordan TG (1996): Mucociliary clearance in the airways. Am. J. Respir. Crit. Care Med. 154, 1868–1902.
Widdicombe JH (1997): Ion transport by airway epithelia. In The Lung. Scientific Foundations. 2nd Edition, eds. RG Crystal & JB West, pp 573–584. Philadelphia: Lippincott-Raven Publishers.
Winters SL & Yeates DB (1997): Roles of hydration, sodium, and chloride in regulation of canine mucociliary transport system. J. Appl. Physiol. 83, 1348–1359.
Wlodek ME, Hooper SB, Thorburn GD, Tester ML & Harding R (1998): Effects of prostaglandin E2 on renal function and lung liquid dynamics in foetal sheep. Clin. Exp. Pharmacol. Physiol. 25, 805–812.
Yager D, Kamm RD & Drazen JM. (1995): Airway wall liquid. Sources and role as an amplifier of bronchoconstriction. Chest 107, 105–110.
Yeates DB, Besseris GJ & Wong LB (1997): Physicochemical properties of mucus and its propulsion. In The Lung. Scientific Foundations. 2nd Edition, eds. RG Crystal & JB West, pp 487–503. Philadelphia: Lippincott-Raven Publishers.
Author information
Authors and Affiliations
Contributions
Guarantor: H. Kalhoff.
Corresponding author
Rights and permissions
About this article
Cite this article
Kalhoff, H. Mild dehydration: a risk factor of broncho-pulmonary disorders?. Eur J Clin Nutr 57 (Suppl 2), S81–S87 (2003). https://doi.org/10.1038/sj.ejcn.1601906
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ejcn.1601906
Keywords
This article is cited by
-
Analysis of the Relationship Between Hemorheologic Parameters, Aluminum, Manganese, and Selenium in Smokers
Biological Trace Element Research (2019)
-
XII AIST 2018 Conference: “The thousand faces of cough: clinical and therapeutic updates”
Multidisciplinary Respiratory Medicine (2018)
-
Clinicopathological and EBV analysis of respiratory epithelial adenomatoid hamartoma
Diagnostic Pathology (2014)
-
Differences in Mucociliary activity of volunteers undergoing Ramadan versus Nineveh fasting
European Archives of Oto-Rhino-Laryngology (2013)
-
A study of fluid intake from beverages in a sample of healthy French children, adolescents and adults
European Journal of Clinical Nutrition (2010)