Abstract
Objective: To test the hypothesis that milk drinking increases the risk of ischaemic heart disease (IHD) and ischaemic stroke in a prospective study.
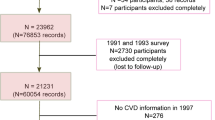
Design: In the Caerphilly Cohort Study dietary data, including milk consumption, were collected by a semiquantitative food frequency questionnaire in 1979–1983. The cohort has been followed for 20–24 y and incident IHD and stroke events identified.
Subjects: A representative population sample in South Wales, of 2512 men, aged 45–59 y at recruitment.
Main outcome measures: In total, 493 men had an IHD event and 185 an ischaemic stroke during follow-up.
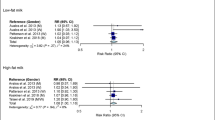
Results: After adjustment, the hazard ratio in men with a milk consumption of one pint (0.57 l) or more per day, relative to men who stated that they consumed no milk, is 0.71 (0.40–1.26) for IHD and 0.66 (0.24–1.81) for ischaemic stroke. At baseline, 606 men had had clinical or ECG evidence of vascular disease, and in these the vascular risk was even lower (0.37; 0.15–0.90). The hazard ratio for IHD and ischaemic stroke combined is 0.64 (0.39–1.06) in all men and 0.37 (0.15–0.90) in those who had had a prior vascular event.
Conclusion: The data provide no convincing evidence that milk consumption is associated with an increase in vascular disease risk. Evidence from an overview of all published cohort studies on this topic should be informative.
Sponsorship: The Medical Research Council, the University of Wales College of Medicine and Bristol University. Current support is from the Food Standards Agency.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Abbott RD, Curb JD, Rodriguez BL, Sharp DS, Birchfield CM & Yano K (1996): Effect of dietary calcium and milk consumption on risk of thromboembolic stroke in older middle aged men: The Honolulu Heart Program. Stroke 27, 813–818.
Ackley S, Barrett-Connor E & Suarez L (1983): Dairy products, calcium and blood pressure. Am. J. Nutr. 38, 457–461.
Bainton D, Baker IA, Sweetnam PM, Yarnell JWG & Elwood PC (1988): Prevalence of ischaemic heart disease: the Caerphilly and Speedwell Surveys. Br. Heart J. 59, 201–206.
Baker IA, Pickering J, Elwood PC, Bayer A & Ebrahim S (2002): Fibrinogen, viscosity and white blood cell count predict myocardial infarction, but not cerebral infarction: evidence from the Caerphilly and Speedwell cohort. Thromb Haemost 87, 421–425.
Barr SI, McCarron DA, Heaney RP, Dawson-Hughes B, Berga SL, Stern JS & Oparil S (2000): Effects if increased consumption of fluid milk on energy and nutrient intake, body weight, and cardiovascular risk factors in healthy older adults. J. Am. Diet. Assoc. 100, 810–817.
Elwood PC (2001): Milk, coronary disease and mortality. J. Epidemiol. Commun. Health 55, 375.
Elwood PC, Beswick A, Pickering J, McCarron P, O’Brien JR, Renaud SR & Flower RJ (2001a): Platelet tests in the prediction of myocardial infarction and stroke: evidence from the Caerphilly study. Br. J. Haematol. 113, 514–520.
Elwood PC, Pickering J & Gallacher JEJ (2001b): Cognitive function and blood rheology: results from the Caerphilly cohort of older men. Age Ageing 30, 135–139.
Elwood PC, Pickering J, Fehily AM, Hughes J & Ness A (2004): Milk drinking, ischaemic heart disease and ischaemic stroke. II. evidence from cohort studies. Eur. J. Clin. Nutr. 58, 718–724.
Fehily AM & Hopkinson T (1993): Do we need information about portion sizes to rank individuals by their nutrient intakes? J. Hum. Nutr. Diet. 6, 101–111.
Fehily AM, Yarnell JWG & Butland BK (1987): Diet and ischaemic heart disease in the Caerphilly study. Hum. Nutr. Appl. Nutr. 41A, 319–326.
Fehily AM, Butland BK, Holiday RM & Yarnell JWG (1988): Dietary studies in the Caerphilly Heart Disease Survey. Food Sci. Nutr. 42F, 77–78.
Gallacher JEJ, Yarnell JWG, Sweetnam PM, Elwood PC & Stansfeld SA (1999) Anger and incident heart disease in the Caerphilly study. Psychosomatic Med. 61, 446–453.
Greenwood R, McCarron P, Elwood PC, Ben Shlomo Y, Bayer A, Baker IA, Frankell S, Ebrahim S, Murray L & Davey Smith G (2001): The incidence and aetiology of stroke in the Caerphilly and Speedwell Collaborative studies. I Methods and incidence of events. Public Health 115, 4–11.
Hajjar IM, Grim CE & Kotchen TA (2003): Dietary calcium lowers the age-related rise in blood pressure in the United States: the NHANES III survey. J. Clin. Hypertens. (Greenwich) 5, 122–126.
Iso H, Stampfer MJ, Manson JE, Rexrode K, Hennekens CH, Colditz GA, Speizer FE & Willett WC (1999): Prospective study of calcium, potassium and magnesium intake and risk of stroke in women. Stroke 30, 1772–1779.
Jorde R & Bonna KH (2001): Calcium from dairy products, vitamin D intake and blood pressure: the Tromso Study. Am. J. Clin. Nutr. 73, 659–660.
Naidoo J & Willis J (1994): Health Promotion: Foundation for Practice. London: Bailliere Tindall.
Ness AR, Davey Smith G & Hart C (2001): Milk, coronary heart disease and mortality. J. Epidemiol. Commun. Health 55, 379–382.
Nutritional Aspects of Cardiovascular Disease (1994): Report of the Cardiovascular Review Group: the Committee on Medical Aspects of Food Policy. London: HMSO.
Pryer J, Cappuccio FP & Elliott P (1995): Dietary calcium and blood pressure: a review of the observational studies. J. Hum. Hypertens. 9, 597–604.
Roberts DCK, Truswell AS, Sullivan DR, Gorrie J, Darnton-Hill I, Norton H, Thomas MA & Allen JK (1982): Milk, plasma cholesterol and controls in nutritional experiments. Atherosclerosis 42, 323–325.
Segall JJ (1977): Is milk a coronary health hazard? Br. J. Prev. Soc. Med. 31, 81–85.
St Onge MP, Farnworth ER & Jones PJH (2000): Consumption of fermented and nonfermented dairy products: effects on cholesterol concentrations and metabolism. Am. J. Clin. Nutr. 71, 674–681.
Steinmetz KA, Childs MT, Stimson C, Kushi LH, McGovern PG, Potter JD & Yamanaka WK (1994): Effect of consumption of whole milk and skim milk on blood lipids profiles in healthy men. Am. J. Clin. Nutr. 59, 612–618.
The Caerphilly & Speedwell Collaborative Group (1984): Caerphilly and Speedwell collaborative heart disease studies. J. Epidemiol. Commun. Health 38, 259–262.
Vijver L Van der, Wall M Van der, Wetterings KGC, Dekker JM, Schouten EG & Kok FJ (1992): Calcium intake and 28-year cardiovascular and coronary heart disease mortality in Dutch civil servants. Int. J. Epidemiol. 21, 36–39.
Yarnell JWG, Patterson CC, Sweetnam PM, Thomas HF, Bainton D, Elwood PC, Bolton CH & Miller N (2001): Do total and high density lipoprotein cholesterol and triglycerides act independently in the prediction of ischaemic heart disease? Arterioscler. Thromb. Vasc. Biol. 21, 1340–1345.
Acknowledgements
The Caerphilly study was conducted by the former MRC Epidemiology Unit (South Wales) and was funded by the Medical Research Council of the United Kingdom. The archive is now maintained by the Department of Social Medicine in the University of Bristol. We are grateful to Mr Stephen Swinglehurst, Operations Manager of Farmers and Dairymen, who supplied data on the distribution of milk in the Caerphilly area. We thank John Fennick for statistical help and advice. Janet Pickering and Janie Hughes are supported by the Food Standards Agency.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Elwood, P., Pickering, J., Fehily, A. et al. Milk drinking, ischaemic heart disease and ischaemic stroke I. Evidence from the Caerphilly cohort. Eur J Clin Nutr 58, 711–717 (2004). https://doi.org/10.1038/sj.ejcn.1601868
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ejcn.1601868
Keywords
This article is cited by
-
Intake of dairy products and associations with major atherosclerotic cardiovascular diseases: a systematic review and meta-analysis of cohort studies
Scientific Reports (2021)
-
Whole milk consumption and risk of cardiovascular disease and mortality: Isfahan Cohort Study
European Journal of Nutrition (2019)
-
Milk and dairy consumption and risk of cardiovascular diseases and all-cause mortality: dose–response meta-analysis of prospective cohort studies
European Journal of Epidemiology (2017)
-
The association between dairy product intake and cardiovascular disease mortality in Chinese adults
European Journal of Nutrition (2017)
-
Daily milk consumption and all-cause mortality, coronary heart disease and stroke: a systematic review and meta-analysis of observational cohort studies
BMC Public Health (2016)