Abstract
Objective: To study the level of and changes in basal metabolic rate (BMR) in children with a solid tumour at diagnosis and during treatment in order to provide a more accurate estimate of energy requirements for nutritional support.
Design: An observational study.
Setting: Tertiary care at the Centre for Paediatric Oncology, University Hospital Nijmegen.
Subjects: Thirteen patients were recruited from a population of patients visiting the University Hospital Nijmegen for treatment. All patients asked to participate took part in and completed the study.
Intervention: BMR was measured by indirect calorimetry, under stringent, standardised conditions, for 20 min and on three different occasions in all patients. Continuous breath gas analysis using a mouthpiece was performed. Weight, height and skinfold measurements were performed before each measurement.
Main outcome measures: BMR was expressed as percentage of the estimated reference value, according to the Schofield formulas based on age, weight and sex, and in kJ (kcal) per kg of fat-free mass.
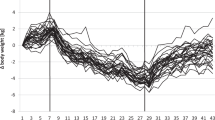
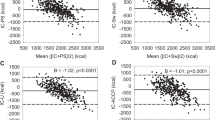
Results: At diagnosis, the BMR was higher than the estimated reference BMR in all patients and 44% of the patients were considered hypermetabolic. Mean BMR (as percentage of reference) was significantly increased (11.6% (s.d. 6.7%); P=0.001), but decreased during treatment in 12 of the 13 patients (mean decrease 12.7% (s.d. 3.9%); P<0.0001). Furthermore, a significant negative correlation (P=−0.67; P=0.01) was found between the change in BMR and tumour response.
Conclusions: These data suggest that the BMR of children with a solid tumour is increased at diagnosis and possibly during the first phase of oncologic treatment. This may be important when determining energy requirements for nutritional support.
European Journal of Clinical Nutrition (2001) 55, 673–681
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Andrassy RJ & Chwals WJ (1998) Nutritional support of the paediatric oncology patient Nutrition 14 124–129
Arbeit JM, Lees DE, Corsey R & Brennan MF (1984) Resting energy expenditure in controls and cancer patients with localized and diffuse disease Ann. Surg. 199 292–298
Bond SA, Han AM, Wootton SA & Kohler JA (1992) Energy intake and basal metabolic rate during maintenance chemotherapy Arch. Dis. Child. 67 229–232
Boothby WM, Berkson J & Dunn HL (1936) Studies on the energy of metabolism of normal individuals: a standard for basal metabolism with a nomogram for clinical application Am. J. Physiol. 3 468–483
Bozetti F, Pagnoni AM & Del Vecchio M (1980) Excessive caloric expenditure as a cause of malnutrition in patients with cancer Surg. Gynecol. Obstet. 150 229–234
den Broeder E, Lippens RJJ, van’t Hof MA, Tolboom JJM, van Staveren WA, Hofman Z & Sengers RCA (1998) Effects of naso-gastric tube feeding on the nutritional status of children with cancer Eur. J. Clin. Nutr. 52 494–500
den Broeder E, Lippens RJJ, van’t Hof MA, Tolboom JJM, Sengers RCA, van den Berg AMJ, van Houdt NBM, Hofman Z & van Staveren WA (2000) Naso-gastric tube feeding in children with cancer: the effect of two different formulas on weight, body composition and serum protein concentrations J. Parenter. Enteral Nutr. 24 351–360.
Brown JK (1993) Gender, age, usual weight, and tobacco use as predictors of weight loss in patients with lung cancer Oncol. Nurs. Forum 20 466–472
Delbecque-Boussard L, Gottrand F, Ategbo S, Nelken B, Mazingue F, Vic P, Farriaux JP & Turck D (1997) Nutritional status of children with acute lymphoblastic leukemia: a longitudinal study Am. J. Clin. Nutr. 65 95–100
Deurenberg P, Pieters JJL & Hautvast JGAJ (1990) The assessment of the body fat percentage by skinfold thickness measurements in childhood and young adolescence Br. J. Nutr. 63 293–303
Dörffel W, Schellong G, Rühl U & Pötter R (1995) GPOH-HD 95 Studienprotokoll, Ahhang 8
Firouzbakhsh S, Mathis RK, Dorchester WL, Oseas RS, Groncy PK, Grant KE & Finklestein JZ (1993) Measured resting energy expenditure in children J. Pediatr. Gastroenterol. Nutr. 16 136–142
Fredriks AM, Van Buuren 5, Burgmeijer RJF, Meulmeester JF, Beuker RJ, Brugman E, Roede MJ, Verloove-Vanhorick SP & Wit JM (2000) Continuing positive secular growth change in The Netherlands (1955–1997) Pediatr. Res. 47 316–323
Fredrix EW, Soeters PB, Deerenberg IM, Kester AD, von Meyenfeldt MF & Saris WH (1990) Resting and sleeping energy expenditure in the elderly Eur. J. Clin. Nutr. 44 741–747
Fredrix EW, Soeters PB, von Meyenfeldt MF & Saris WH (1991a) Resting energy expenditure in cancer patients before and after gastrointestinal surgery J. Parenter. Enteral Nutr. 15 604–607
Fredrix EWHM, Soeters PB, Wouters EFM, Deerenberg IM, von Meyenfeldt MF & Saris WHM (1991b) Effect of different tumour types on resting energy expenditure Cancer Res. 51 6138–6141
Frisancho AR (1981) New norms of upper limb fat and muscle areas for the assessment of nutritional status Am. J. Clin. Nutr. 34 2540–2545
Hyltander A, Körner U & Lundholm KG (1993) Evaluation of mechanisms behind elevated energy expenditure in cancer patients with solid tumours Eur. J. Clin. Invest. 23 46–52
Isbell TR, Klesges RC, Meyers AW & Klesges LM (1991) Measurement reliability and reactivity using repeated measurements of resting energy expenditure with a face mask, mouthpiece, and ventilated canopy J. Parenter. Enteral Nutr. 15 165–168
Kaplan AS, Zemel BS, Neiswender KM & Stallings VA (1995) Resting energy expenditure in clinical pediatrics: measured versus predicted equations J. Pediatr. 127 200–205
Kern AK & Norton JA (1988) Cancer cachexia J. Parenter. Enteral Nutr. 12 286–298
Kien CL & Camitta BM (1987) Close association of accelerated rates of whole body protein turnover (synthesis and breakdown) and energy expenditure in children with newly diagnosed acute lymphocytic leukemia J. Parenter. Enteral Nutr. 11 129–134
Kun LE (1997) General principles of radiation therapy In Principles and Practise of Pediatric Oncology, 3rd edn, eds. PA Pizzo & DG Poplack 289–321. Philadelphia, PA: Lippincott Raven.
Lewinter-Suskind L, Suskind D, Murthy KK & Suskind RM (1993) The malnourished child. In Textbook of Paediatric Nutrition, 2nd edn, eds. RM Suskind & L Lewinter-Suskind 127–140. New York: Raven Press.
Lindmark L, Bennegard K, Eden E, Ekman L, Schersten T, Svaninger G & Lundholm K (1984) Resting energy expenditure in malnourished patients with and without cancer Gastroenterology 87 402–408
Luketich JD, Mullen JL, Feurer ID, Sternlieb J & Fried RC (1990) Ablation of normal energy expenditure by curative tumor resection Arch. Surg. 125 337–341
Mauer AM, Burgess JB, Donaldson SS, Rickard KA, Stallings VA, van Eys J & Wininck M (1990) Special nutritional needs of children with malignancies: a review J. Parenter. Enteral Nutr. 14 315–324
McArdle WD, Katch FI & Katch VL (eds) (1996) Exercise Physiology: Energy, Nutrition, and Human Performance 139–147. Baltimore, MA: Williams & Wilkins.
Merrit RJ, Ashley JM, Siegel SE, Sinatra FR, Thomas DW & Hays DM (1981) Calorie and protein requirements of paediatric patients with acute non-lymphoblastic leukemia J. Parenter. Enteral Nutr. 5 20–23
Pencharz PB (1998) Aggressive oral, enteral or parenteral nutrition: prescriptive decisions in children with cancer Int. J. Cancer 11 (Suppl) S73–S75
Pencharz PB & Azcue MP (1995) Measured resting energy expenditure in clinical practice J. Pediatr. 127 269–271
Picton SV (1998) Aspects of altered metabolism in children with cancer Int. J. Cancer 11(Suppl) S62–S64
Picton SV, Eden OB and Rothwell NJ (1995) Metabolic rate, interleukin 6 and cachexia in children with malignancy (Abstract) Med. Pediatr. Oncol. 5 24 9
Rickard KA, Coates TD, Grosfeld JL, Weetman RM & Baehner RL (1986) The value of nutrition support in children with cancer Cancer 58 1904–1910
Schofield WN (1985) Predicting basal metabolic rate, new standards and review of previous work Hum. Nutr. Clin. Nutr. 39(Suppl) S5–S41
Scott CB (1993) Resting metabolic rate variability as influenced by mouthpiece and noseclip practice procedures J. Burn Care Rehabil. 4 573–577
Staal-van de Brekel AJ, Dentener MA, Schols AMWJ, Buurman WA & Wouters EFM (1995) Increased resting energy expenditure and weight loss are related to a systemic inflammatory response in lung cancer patients J. Clin. Oncol. 12 2600–2605
Stallings VA, Vaisman N, Chan HSL, Weitzman SS, Hahn E & Pencharz PB (1989) Energy metabolism in children with newly diagnosed acute lymphoblastic leukemia Pediatr. Res. 26 154–157
Vaisman N, Stallings VA, Chan HSL, Weitzman SS, Clarke R & Pencharz PB (1993) Effect of chemotherapy on the energy and protein metabolism of children near the end of treatment for acute lymphoblastic leukaemia Am. J. Clin. Nutr. 57 679–684
Warner JT, Bell W, Webb DK & Gregory JW (1998) Daily energy expenditure and physical activity in survivors of childhood malignancy Pediatr. Res. 43 607–613
Waterlow JC, Buzina R, Keller W, Nichaman MZ & Tanner JM (1977) The presentation and use of weight and height data for comparing the nutritional status of groups of children under the age of 10 years Bull. WHO 55 489–498
Yu LC (1993) Nutrition and childhood malignancies In Textbook of Paediatric Nutrition, 2nd edn, eds. RM Suskind & L Lewinter-Suskind 417–424. New York: Raven Press.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
den Broeder, E., Oeseburg, B., Lippens, R. et al. Basal metabolic rate in children with a solid tumour. Eur J Clin Nutr 55, 673–681 (2001). https://doi.org/10.1038/sj.ejcn.1601199
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ejcn.1601199
Keywords
This article is cited by
-
Trends in age- and sex-adjusted body mass index and the prevalence of malnutrition in children with cancer over 42 months after diagnosis: a single-center cohort study
European Journal of Pediatrics (2020)
-
Glomerular hyperfiltration in children with cancer: prevalence and a hypothesis
Pediatric Radiology (2017)
-
A pilot study of gas chromatograph/mass spectrometry-based serum metabolic profiling of colorectal cancer after operation
Molecular Biology Reports (2010)
-
Genotype × diet interactions in mice predisposed to mammary cancer. I. Body weight and fat
Mammalian Genome (2008)