Abstract
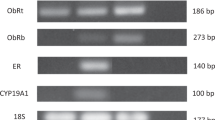
We reported previously that the obesity hormone leptin is overexpressed in breast cancer biopsies. Here, we investigated molecular mechanisms involved in this process, focusing on conditions that are associated with obesity, that is, hyperinsulinemia and induction of hypoxia. By using quantitative real-time PCR, immunofluorescent detection of proteins and enzyme-linked immunosorbent assays, we found that treatment of MCF-7 breast cancer cells with high doses of insulin or the hypoxia-mimetic agent CoCl2, or culturing the cells under hypoxic conditions significantly increased the expression of leptin mRNA and protein. Notably, the greatest leptin mRNA and protein expression were observed under combined hyperinsulinemia and hypoxia or hypoxia-mimetic treatments. Luciferase reporter assays suggested that increased leptin synthesis could be related to the activation of the leptin gene promoter. DNA affinity precipitation and chromatin immunoprecipitation experiments revealed that insulin, CoCl2 and/or hypoxia treatments augmented nuclear accumulation of hypoxia-inducible factor-1α (HIF-1α) and increased its interaction with several upstream leptin regulatory sequences, especially with the proximal promoter containing four hypoxia-response elements and three GC-rich regions. By using reverse chromatin precipitation, we determined that loading of HIF-1α on the proximal leptin promoter concurred with the recruitment of p300, the major HIF coactivator, suggesting that the HIF/p300 complex is involved in leptin transcription. The importance of HIF-1α in insulin- and CoCl2-activated leptin mRNA and protein expression was confirmed using RNA interference.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 50 print issues and online access
$259.00 per year
only $5.18 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
References
Ahima RS, Flier JS . (2000). Adipose tissue as an endocrine organ. Annu Rev Physiol 62: 413–437.
Calle EE, Thun MJ . (2004). Obesity and cancer. Oncogene 23: 6365–6378.
Cascio S, Bartella V, Garofalo C, Russo A, Giordano A, Surmacz E . (2007). Insulin-like growth factor 1 differentially regulates estrogen receptor-dependent transcription at estrogen response element and AP-1 sites in breast cancer cells. J Biol Chem 282: 3498–3506.
De Vos P, Lefebvre AM, Shrivo I, Fruchart JC, Auwerx J . (1998). Glucocorticoids induce the expression of the leptin gene through a non-classical mechanism of transcriptional activation. Eur J Biochem 253: 619–626.
Ebert BL, Bunn HF . (1998). Regulation of transcription by hypoxia requires a multiprotein complex that includes hypoxia-inducible factor 1, an adjacent transcription factor, and p300/CREB binding protein. Mol Cell Biol 18: 4089–4096.
Eisenberg A, Biener E, Charlier M, Krishnan RV, Djiane J, Herman B et al. (2004). Transactivation of erbB2 by short and long isoforms of leptin receptors. FEBS Lett 565: 139–142.
Garofalo C, Koda M, Cascio S, Sulkowska M, Kanczuga-Koda L, Golaszewska J et al. (2006). Increased expression of leptin and the leptin receptor as a marker of breast cancer progression: possible role of obesity-related stimuli. Clin Cancer Res 12: 1447–1453.
Garofalo C, Sisci D, Surmacz E . (2004). Leptin interferes with the effects of the antiestrogen ICI 182,780 in MCF-7 breast cancer cells. Clin Cancer Res 10: 6466–6475.
Garofalo C, Surmacz E . (2006). Leptin and cancer. J Cell Physiol 207: 12–22.
Generali D, Berruti A, Brizzi MP, Campo L, Bonardi S, Wigfield S et al. (2006). Hypoxia-inducible factor-1alpha expression predicts a poor response to primary chemoendocrine therapy and disease-free survival in primary human breast cancer. Clin Cancer Res 12: 4562–4568.
Gonzalez RR, Cherfils S, Escobar M, Yoo JH, Carino C, Styer AK et al. (2006). Leptin signaling promotes the growth of mammary tumors and increases the expression of vascular endothelial growth factor (VEGF) and its receptor type two (VEGF-R2). J Biol Chem 281: 26320–26328.
Gray MJ, Zhang J, Ellis LM, Semenza GL, Evans DB, Watowich SS et al. (2005). HIF-1alpha, STAT3, CBP/p300 and Ref-1/APE are components of a transcriptional complex that regulates Src-dependent hypoxia-induced expression of VEGF in pancreatic and prostate carcinomas. Oncogene 24: 3110–3120.
Grosfeld A, Andre J, Hauguel-De Mouzon S, Berra E, Pouyssegur J, Guerre-Millo M . (2002). Hypoxia-inducible factor 1 transactivates the human leptin gene promoter. J Biol Chem 277: 42953–42957.
Hirota K, Semenza GL . (2006). Regulation of angiogenesis by hypoxia-inducible factor 1. Crit Rev Oncol Hematol 59: 15–26.
Ishikawa M, Kitayama J, Nagawa H . (2004). Enhanced expression of leptin and leptin receptor (OB-R) in human breast cancer. Clin Cancer Res 10: 4325–4331.
Klein S, Wadden T, Sugerman HJ . (2002). AGA technical review on obesity. Gastroenterology 123: 882–932.
Losso JN, Bawadi HA . (2005). Hypoxia inducible factor pathways as targets for functional foods. J Agric Food Chem 53: 3751–3768.
Majumder PK, Febbo PG, Bikoff R, Berger R, Xue Q, McMahon LM et al. (2004). mTOR inhibition reverses Akt-dependent prostate intraepithelial neoplasia through regulation of apoptotic and HIF-1-dependent pathways. Nat Med 10: 594–601.
Mason MM, He Y, Chen H, Quon MJ, Reitman M . (1998). Regulation of leptin promoter function by Sp1, C/EBP, and a novel factor. Endocrinology 139: 1013–1022.
Meissner U, Ostreicher I, Allabauer I, Rascher W, Dotsch J . (2003). Synergistic effects of hypoxia and insulin are regulated by different transcriptional elements of the human leptin promoter. Biochem Biophys Res Commun 303: 707–712.
Melzner I, Scott V, Dorsch K, Fischer P, Wabitsch M, Bruderlein S et al. (2002). Leptin gene expression in human preadipocytes is switched on by maturation-induced demethylation of distinct CpGs in its proximal promoter. J Biol Chem 277: 45420–45427.
Miki N, Ikuta M, Matsui T . (2004). Hypoxia-induced activation of the retinoic acid receptor-related orphan receptor alpha4 gene by an interaction between hypoxia-inducible factor-1 and Sp1. J Biol Chem 279: 15025–15031.
Miller SG, De Vos P, Guerre-Millo M, Wong K, Hermann T, Staels B et al. (1996). The adipocyte specific transcription factor C/EBPalpha modulates human ob gene expression. Proc Natl Acad Sci USA 93: 5507–5511.
Morelli C, Garofalo C, Sisci D, del Rincon S, Cascio S, Tu X et al. (2004). Nuclear insulin receptor substrate 1 interacts with estrogen receptor alpha at ERE promoters. Oncogene 23: 7517–7526.
Pore N, Jiang Z, Shu HK, Bernhard E, Kao GD, Maity A . (2006). Akt1 activation can augment hypoxia-inducible factor-1alpha expression by increasing protein translation through a mammalian target of rapamycin-independent pathway. Mol Cancer Res 4: 471–479.
Porter GA, Inglis KM, Wood LA, Veugelers PJ . (2006). Effect of obesity on presentation of breast cancer. Ann Surg Oncol 13: 327–332.
Pouyssegur J, Dayan F, Mazure NM . (2006). Hypoxia signalling in cancer and approaches to enforce tumour regression. Nature 441: 437–443.
Revillion F, Charlier M, Lhotellier V, Hornez L, Giard S, Baranzelli MC et al. (2006). Messenger RNA expression of leptin and leptin receptors and their prognostic value in 322 human primary breast cancers. Clin Cancer Res 12: 2088–2094.
Snoussi K, Strosberg AD, Bouaouina N, Ben Ahmed S, Helal AN, Chouchane L . (2006). Leptin and leptin receptor polymorphisms are associated with increased risk and poor prognosis of breast carcinoma. BMC Cancer 6: 38.
Surmacz E . (2007). Obesity hormone leptin: a new target in breast cancer? Breast Cancer Res 9: 301.
Treins C, Giorgetti-Peraldi S, Murdaca J, Monthouel-Kartmann MN, Van Obberghen E . (2005). Regulation of hypoxia-inducible factor (HIF)-1 activity and expression of HIF hydroxylases in response to insulin-like growth factor I. Mol Endocrinol 19: 1304–1317.
Vleugel MM, Greijer AE, Shvarts A, van der Groep P, van Berkel M, Aarbodem Y et al. (2005). Differential prognostic impact of hypoxia induced and diffuse HIF1 alpha expression in invasive breast cancer. J Clin Pathol 58: 172–177.
Wauters M, Considine RV, Van Gaal LF . (2000). Human leptin: from an adipocyte hormone to an endocrine mediator. Eur J Endocrinol 143: 293–311.
Zhong H, De Marzo AM, Laughner E, Lim M, Hilton DA, Zagzag D et al. (1999). Overexpression of hypoxia-inducible factor 1alpha in common human cancers and their metastases. Cancer Res 59: 5830–5835.
Acknowledgements
We are grateful to Professor Auwerx, Institut de Génétique et de Biologie Moléculaire et Cellulaire, CNRS/INSERM/Université Louis Pasteur, Illkirch, France, for providing the OB1plasmid. This work was supported by the Sbarro Health Research Organization and the WW Smith Charitable Trust.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cascio, S., Bartella, V., Auriemma, A. et al. Mechanism of leptin expression in breast cancer cells: role of hypoxia-inducible factor-1α. Oncogene 27, 540–547 (2008). https://doi.org/10.1038/sj.onc.1210660
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.onc.1210660
Keywords
This article is cited by
-
Aberrant miR-874-3p/leptin/EGFR/c-Myc signaling contributes to nasopharyngeal carcinoma pathogenesis
Journal of Experimental & Clinical Cancer Research (2022)
-
Metabolic pathways in obesity-related breast cancer
Nature Reviews Endocrinology (2021)
-
Targeting obesity-related dysfunction in hormonally driven cancers
British Journal of Cancer (2021)
-
Leptin produced by obesity-altered adipose stem cells promotes metastasis but not tumorigenesis of triple-negative breast cancer in orthotopic xenograft and patient-derived xenograft models
Breast Cancer Research (2019)
-
C-myc overexpression drives melanoma metastasis by promoting vasculogenic mimicry via c-myc/snail/Bax signaling
Journal of Molecular Medicine (2017)