Abstract
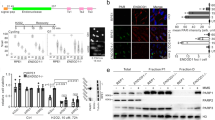
SAP is an adaptor molecule with one SH2 domain and it is expressed in activated T and NK cells, where it is required for the appropriate signaling from the SLAM family of surface receptors. Deleted or mutated SAP genes that encode functionally defective protein are associated with the X-linked lymphoproliferative disease (XLP). This primary immunodeficiency is characterized by extreme sensitivity to Epstein–Barr virus (EBV) infection, dysgammaglobulinemia and a high rate of lymphoma development. The vigorous T- and B-cell proliferation that follows EBV infection and the high incidence of lymphomas (30%) in XLP patients might reflect functional defects in cell cycle and/ or apoptosis control. Our experiments show that SAP is a target of p53. In Burkitt lymphoma (BL) lines transfected with a temperatur-sensitive (ts) p53, SAP mRNA and protein expression was dependent on wild-type (wt) p53. Activation of endogenous wt p53 in BLs and lymphoblastoid cell lines led to the induction of SAP and this was inhibited by the specific p53 inhibitor pifithrin-α. Cell lines that carried mutant p53 did not express SAP under similar conditions. Moreover, we have shown binding of wt p53 to the promoter region of SAP by ChIP assay. Our results suggest that SAP contributes to the execution of some p53 functions.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 50 print issues and online access
$259.00 per year
only $5.18 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
References
Bourdon JC, Deguin-Chambon V, Lelong JC, Dessen P, May P, Debuire B and May E . (1997). Oncogene, 14, 85–94.
Chan B, Lanyi A, Song HK, Griesbach J, Simarro-Grande M, Poy F, Howie D, Sumegi J, Terhorst C and Eck MJ . (2003). Nat. Cell Biol., 5, 155–160.
Coffey AJ, Brooksbank RA, Brandau O, Oohashi T, Howell GR, Bye JM, Cahn AP, Durham J, Heath P, Wray P, Pavitt R, Wilkinson J, Leversha M, Huckle E, Shaw-Smith CJ, Dunham A, Rhodes S, Schuster V, Porta G, Yin L, Serafini P, Sylla B, Zollo M, Franco B, Bolino A, Seri M, Lanyi A, Davis JR, Webster D, Harris A, Lenoir G, de St Basile G, Jones A, Behloradsky BH, Achatz H, Murken J, Fassler R, Sumegi J, Romeo G, Vaudin M, Ross MT, Meindl A and Bentley DR . (1998). Nat. Genet., 20, 129–135.
Czar MJ, Kersh EN, Mijares LA, Lanier G, Lewis J, Yap G, Chen A, Sher A, Duckett CS, Ahmed R and Schwartzberg PL . (2001). Proc. Natl. Acad. Sci. USA, 98, 7449–7454.
Fei P, Bernhard EJ and El-Deiry WS . (2002). Cancer Res., 62, 7316–7327.
Gorgoulis VG, Zacharatos P, Kotsinas A, Kletsas D, Mariatos G, Zoumpourlis V, Ryan KM, Kittas C and Papavassiliou AG . (2003). EMBO J., 22, 1567–1578.
Grierson H and Purtilo DT . (1987). Ann. Intern. Med., 106, 538–545.
Harada S, Bechtold T, Seeley JK and Purtilo DT . (1982). Int. J. Cancer, 30, 739–744.
Harrington DS, Weisenburger DD and Purtilo DT . (1987). Cancer, 59, 1419–1429.
Komarov PG, Komarova EA, Kondratov RV, Christov-Tselkov K, Coon JS, Chernov MV and Gudkov AV . (1999). Science, 285, 1733–1737.
Latour S, Roncagalli R, Chen R, Bakinowski M, Shi X, Schwartzberg PL, Davidson D and Veillette A . (2003). Nat. Cell Biol., 5, 149–154.
Michalovitz D, Halevy O and Oren M . (1990). Cell, 62, 671–680.
Mori T, Anazawa Y, Iiizumi M, Fukuda S, Nakamura Y and Arakawa H . (2002). Oncogene, 21, 2914–2918.
Nagy N, Cerboni C, Mattsson K, Maeda A, Gogolak P, Sumegi J, Lanyi A, Szekely L, Carbone E, Klein G and Klein E . (2000). Int. J. Cancer, 88, 439–447.
Nagy N, Maeda A, Bandobashi K, Kis LL, Nishikawa J, Trivedi P, Faggioni A, Klein G and Klein E . (2002). Int. J. Cancer, 100, 433–440.
Nichols KE, Harkin DP, Levitz S, Krainer M, Kolquist KA, Genovese C, Bernard A, Ferguson M, Zuo L, Snyder E, Buckler AJ, Wise C, Ashley J, Lovett M, Valentine MB, Look AT, Gerald W, Housman DE and Haber DA . (1998). Proc. Natl. Acad. Sci. USA, 95, 13765–13770.
Okan I, Wang Y, Chen F, Hu LF, Imreh S, Klein G and Wiman KG . (1995). Oncogene, 11, 1027–1031.
Parolini S, Bottino C, Falco M, Augugliaro R, Giliani S, Franceschini R, Ochs HD, Wolf H, Bonnefoy JY, Biassoni R, Moretta L, Notarangelo LD and Moretta A . (2000). J. Exp. Med., 192, 337–346.
Ramqvist T, Magnusson KP, Wang Y, Szekely L, Klein G and Wiman KG . (1993). Oncogene, 8, 1495–1500.
Sayos J, Wu C, Morra M, Wang N, Zhang X, Allen D, van Schaik S, Notarangelo L, Geha R, Roncarolo MG, Oettgen H, De Vries JE, Aversa G and Terhorst C . (1998). Nature, 395, 462–469.
Seemayer TA, Gross TG, Egeler RM, Pirruccello SJ, Davis JR, Kelly CM, Okano M, Lanyi A and Sumegi J . (1995). Pediatr. Res., 38, 471–478.
Shlapatska LM, Mikhalap SV, Berdova AG, Zelensky OM, Yun TJ, Nichols KE, Clark EA and Sidorenko SP . (2001). J. Immunol., 166, 5480–5487.
Strahm B, Rittweiler K, Duffner U, Brandau O, Orlowska-Volk M, Karajannis MA, Stadt U, Tiemann M, Reiter A, Brandis M, Meindl A and Niemeyer CM . (2000). Br. J. Haematol., 108, 377–382.
Sumegi J, Huang D, Lanyi A, Davis JD, Seemayer TA, Maeda A, Klein G, Seri M, Wakiguchi H, Purtilo DT and Gross TG . (2000). Blood, 96, 3118–3125.
Sylla BS, Murphy K, Cahir-McFarland E, Lane WS, Mosialos G and Kieff E . (2000). Proc. Natl. Acad. Sci. USA, 97, 7470–7475.
Voelkerding KV, Steffen DW, Zaidi SH and Malter JS . (1995). Oncogene, 10, 515–521.
Williams LL, Rooney CM, Conley ME, Brenner MK, Krance RA and Heslop HE . (1993). Lancet, 342, 587–588.
Wu C, Nguyen KB, Pien GC, Wang N, Gullo C, Howie D, Sosa MR, Edwards MJ, Borrow P, Satoskar AR, Sharpe AH, Biron CA and Terhorst C . (2001). Nat. Immunol., 2, 410–414.
Yin L, Al-Alem U, Liang J, Tong WM, Li C, Badiali M, Medard JJ, Sumegi J, Wang ZQ and Romeo G . (2003). J. Med. Virol., 71, 446–455.
Zhou X, Wong S, Walter J, Jacks T and Eisen HN . (1999). J. Immunol., 162, 3957–3960.
Acknowledgements
We thank Janos Sumegi (Cincinnati Children's Hospital Medical Center, MLC, Cincinnati, Ohio), Wang Qian (Division of Virology, National Institute for Medical Research, London) and Klas G Wiman (CCK, Karolinska Institute, Stockholm) for helpful discussions. The work was supported by the Swedish Cancer Society and by the Cancer Research Institute (New York)/Concern Foundation (Los Angeles).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nagy, N., Takahara, M., Nishikawa, J. et al. Wild-type p53 activates SAP expression in lymphoid cells. Oncogene 23, 8563–8570 (2004). https://doi.org/10.1038/sj.onc.1207908
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.onc.1207908