Abstract
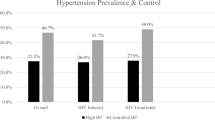
The aim of this study was to describe the pattern of blood pressure (BP) distribution in a multiethnic primary care practice in relation to sociodemographic characteristics, lifestyle and risk factors. Another aim was to analyse the quality of diagnosis and effectiveness of hypertension (HT) treatment. In all, 470 adult patients (⩾16 years old) who visited the Jordbro Health Centre (JHC), Haninge Municipality, participated in this study. A general questionnaire with questions about sociodemographic characteristics, lifestyle, health status and chronic disease was used. Medical records: information on consultations with the general practitioner and prescriptions were collected from the medical records for the year 2001. Furthermore, a medical examination was performed: this consisted of weight, height, systolic (SBP) and diastolic (DBP) blood pressure, and laboratory analyses including fasting blood glucose, serum cholesterol, serum triglycerides, electrocardiogram and spirometry. Out of 464 patients, 114 (24.6%) reported HT. Among the HT patients, 93 (81.6%) had SBP ⩾140 mmHg and 52 (45.6%) DBP ⩾90 mmHg. Among the nonhypertensive patients (n=350), 120 (34.3%) had SBP ⩾140 mmHg and 50 (14.3%) DBP ⩾90 mmHg. Furthermore, there are some patients with high BP who are unknown or undetected. HT treatment among this population is unsatisfactory and greater efforts are required to identify people with high BP and to ensure that they are managed according to the best available evidence.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
SBU. Måttligt förhöjt blodtryck. En systematisk litteraturöversikt (Moderately Elevated Blood Pressure. A Systematic Literature Review), The Swedish Council on Technology Assessment in Health Care, 2004 (in Swedish) Sweden.
Pittrow D et al. Patterns of antihypertensive drug utilization in primary care. Eur J Clin Pharmacol 2004; 60: 135–142.
Farsang C et al. Effective control of hypertension: a project of the Hungarian Society of Hypertension, baseline data. J Hum Hypertens 2004; 18: 591–594.
Fagard RH, Van den Enden M . Treatment and blood pressure control in isolated systolic hypertension vs diastolic hypertension in primary care. J Hum Hypertens 2003; 17: 681–687.
Hajjar I, Kotchen TA . Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988–2000. JAMA 2003; 290: 199–206.
Jo I et al. Prevalence, awareness, treatment, control and risk factors of hypertension in Korea: the Ansan study. J Hypertens 2001; 19: 1523–1532.
Sharma AM, et al, HYDRA Study Group. High prevalence and poor control of hypertension in primary care: cross-sectional study. J Hypertens 2004; 22: 479–486.
Jancso Z et al. [Cardiovascular risk among patients of general practices who are not in current acute care]. Orv Hetil 2003; 144: 1433–1439.
Weinehall L et al. High remaining risk in poorly treated hypertension: the ‘rule of halves’ still exists. J Hypertens 2002; 20: 2081–2088.
Amar J et al PRATIK study investigators. Hypertension in high-risk patients: beware of the underuse of effective combination therapy (results of the PRATIK study). J Hypertens 2002; 20: 779–784.
Carter BL . Implementing the new guidelines for hypertension: JNC 7, ADA, WHO-ISH. J Manage Care Pharm 2004; 10: S18–S25.
Grzybowski A et al. Effectiveness of hypertension treatment assessed by blood pressure level achieved in primary care setting in Poland. Blood Pressure 2003; 12: 232–238.
Supina AL et al. Treatment gaps for hypertension management in rural Canadian patients with type 2 diabetes mellitus. Clin Ther 2004; 26: 598–606.
Steinman MA et al. Clinician awareness of adherence to hypertension guidelines. Am J Med 2004; 117: 747–754.
Khan N, Chockalingam A, Campbell NR . Lack of control of high blood pressure and treatment recommendations in Canada. Can J Cardiol 2002; 18: 657–661.
Staessen JA, Wang JG, Thijs L . Cardiovascular prevention and blood pressure reduction: a quantitative overview updated until 1 March 2003. J Hypertens 2003; 21: 1055–1076.
Niklason A et al Captopril Prevention Project Study Group. Development of diabetes is retarded by ACE inhibition in hypertensive patients—a subanalysis of the Captopril Prevention Project (CAPPP). J Hypertens 2004; 22: 645–652.
Scheen AJ . Prevention of type 2 diabetes mellitus through inhibition of the renin–angiotensin system. Drugs 2004; 64: 2537–2565.
Al-Windi A . Depression in general practice. Nordic Psychiatry 2005 (in press).
Tibblin G, Peciva S, Kullman S, Svardsudd K . ‘The Gothenburg quality of life instrument’: an assessment of well-being and symptoms among men born 1913 and 1923. Methods and validity. Scand J Prim Health Care Suppl 1990; 1: 33–38.
JMP program. Statistical Discovery Software. Introductory Guide, ed. version 4 SAS Institute Inc.: Cary, NC, 2000.
Scisney-Matlock M et al. Comparison of quality-of-hypertension-care indicators for groups treated by physician versus groups treated by physician–nurse team. J Am Acad Nurse Pract 2004; 16: 17–23.
Ornstein SM, Nietert PJ, Dickerson LM . Hypertension management and control in primary care: a study of 20 practices in 14 states. Pharmacotherapy 2004; 24: 500–507.
Hyman DJ, Pavlik VN . Self-reported hypertension treatment practices among primary care physicians: blood pressure thresholds, drug choices, and the role of guidelines and evidence-based medicine. Arch Intern Med 2000; 160: 2281–2286.
Pavlik VN, Hyman DJ . How well are we managing and monitoring high blood pressure? Curr Opin Nephrol Hypertens 2003; 12: 299–304.
McKerracher A . Treating to hypertension targets. Heart 2004; 90: S33–S35, 39–40.
Williams B et al BHS guidelines working party, for the British Hypertension Society. British Hypertension Society guidelines for hypertension management 2004 (BHS-IV): summary. BMJ 2004; 328: 634–640.
Franklin SS et al. Predominance of isolated systolic hypertension among middle-aged and elderly US hypertensives: analysis based on National Health and Nutrition Examination Survey (NHANES) III. Hypertension 2001; 37: 869–874.
Ford ES et al. Prevalence of the metabolic syndrome among US adults: findings from the third National Health and Nutrition Examination Survey. JAMA 2002; 287: 356–359.
Little P et al. Comparison of agreement between different measures of blood pressure in primary care and daytime ambulatory blood pressure. BMJ 2002; 325: 254.
Parati G . Blood pressure variability: its measurement and significance in hypertension. J Hypertens 2005; 23 (Suppl): S19–S25.
Campbell NR et al. Lifestyle modifications to prevent and control hypertension. 1. Methods and an overview of the Canadian recommendations. Canadian Hypertension Society, Canadian Coalition for High Blood Pressure Prevention and Control, Laboratory Centre for Disease Control at Health Canada, Heart and Stroke Foundation of Canada. CMAJ 1999; 160: S1–S6.
Fodor JG, Whitmore B, Leenen F, Larochelle P . Lifestyle modifications to prevent and control hypertension. 5. Recommendations on dietary salt. Canadian Hypertension Society, Canadian Coalition for High Blood Pressure Prevention and Control, Laboratory Centre for Disease Control at Health Canada, Heart and Stroke Foundation of Canada. CMAJ 1999; 160: S29–S34.
Jacobson TA et al. Characteristics of US adults with the metabolic syndrome and therapeutic implications. Diabetes Obes Metab 2004; 6: 353–362.
Acknowledgements
This study was supported by grants from Stockholm County Council (Dagmar & ALF Fund) and Haninge Municipal Council (Economic Target to Large Cities).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Al-Windi, A. Detection and treatment of hypertension in general health-care practice: a patient-based study. J Hum Hypertens 19, 775–786 (2005). https://doi.org/10.1038/sj.jhh.1001902
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jhh.1001902
Keywords
This article is cited by
-
Hypertension management initiative prospective cohort study: comparison between immediate and delayed intervention groups
Journal of Human Hypertension (2014)
-
Towards improving the clinical assessment and management of human hypertension: an overview from this Journal
Journal of Human Hypertension (2006)