Abstract
Introduction:
Obesity and obstructive sleep apnea each have a substantial genetic basis and commonly coexist in individuals. The degree to which the genetic underpinnings for these disorders overlap has not been previously quantified.
Methods:
A total of 1802 individuals from 310 families in the Cleveland Family Study underwent home sleep studies as well as standardized assessment of body mass index (BMI) and circumferences at the waist, hip and neck. In 713 participants with laboratory sleep studies, fasting blood samples were assayed for leptin, adiponectin and resistin. Variance component models were used to estimate heritability and genetic correlations.
Results:
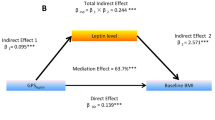
The heritability of the apnea hypopnea index (AHI) was 0.37±0.04 and 0.33±0.07 for home and laboratory sleep studies, respectively. The genetic correlations between AHI and anthropomorphic adiposity measures ranged from 0.57 to 0.61, suggesting that obesity can explain nearly 40% of the genetic variance in sleep apnea. The magnitude of the genetic correlations between apnea severity and adipokine levels was substantially less than those with anthropomorphic measures, ranging from 0.11 to 0.46. After adjusting for BMI, no significant genetic correlation with apnea severity was observed for any of the other adiposity measures.
Conclusions:
Substantial but not complete overlap in genetic bases exists between sleep apnea and anthropomorphic indices of adiposity, and this overlap accounts for more than one-third of the genetic variance in apnea severity. These findings suggest that genetic polymorphisms exist that importantly influence sleep apnea susceptibility through both obesity-dependent and -independent pathways.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Young T, Peppard PE, Gottlieb DJ . Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med 2002; 165: 1217–1239.
Peppard PE, Young T, Palta M, Dempsey J, Skatrud J . Longitudinal study of moderate weight change and sleep-disordered breathing. JAMA 2000; 284: 3015–3021.
Patel SR . Shared genetic risk factors for obstructive sleep apnea and obesity. J Appl Physiol 2005; 99: 1600–1606.
Redline S, Tishler PV, Tosteson TD, Williamson J, Kump K, Browner I et al. The familial aggregation of obstructive sleep apnea. Am J Respir Crit Care Med 1995; 151: 682–687.
Carmelli D, Colrain IM, Swan GE, Bliwise DL . Genetic and environmental influences in sleep-disordered breathing in older male twins. Sleep 2004; 27: 917–922.
Mathur R, Douglas NJ . Family studies in patients with the sleep apnea–hypopnea syndrome. Ann Intern Med 1995; 122: 174–178.
Gislason T, Johannsson JH, Haraldsson A, Olafsdottir BR, Jonsdottir H, Kong A et al. Familial predisposition and cosegregation analysis of adult obstructive sleep apnea and the sudden infant death syndrome. Am J Respir Crit Care Med 2002; 166: 833–838.
Pillar G, Lavie P . Assessment of the role of inheritance in sleep apnea syndrome. Am J Respir Crit Care Med 1995; 151: 688–691.
Stunkard AJ, Foch TT, Hrubec Z . A twin study of human obesity. JAMA 1986; 256: 51–54.
Stunkard AJ, Harris JR, Pedersen NL, McClearn GE . The body-mass index of twins who have been reared apart. N Engl J Med 1990; 322: 1483–1487.
Davies RJ, Ali NJ, Stradling JR . Neck circumference and other clinical features in the diagnosis of the obstructive sleep apnoea syndrome. Thorax 1992; 47: 101–105.
Grunstein R, Wilcox I, Yang TS, Gould Y, Hedner J . Snoring and sleep apnoea in men: association with central obesity and hypertension. Int J Obes 1993; 17: 533–540.
Selby JV, Newman B, Quesenberry Jr CP, Fabsitz RR, King MC, Meaney FJ . Evidence of genetic influence on central body fat in middle-aged twins. Hum Biol 1989; 61: 179–194.
Buxbaum SG, Elston RC, Tishler PV, Redline S . Genetics of the apnea hypopnea index in Caucasians and African Americans: I. segregation analysis. Genet Epidemiol 2002; 22: 243–253.
Redline S, Schluchter MD, Larkin EK, Tishler PV . Predictors of longitudinal change in sleep-disordered breathing in a nonclinic population. Sleep 2003; 26: 703–709.
Palmer LJ, Buxbaum SG, Larkin E, Patel SR, Elston RC, Tishler PV et al. A whole-genome scan for obstructive sleep apnea and obesity. Am J Hum Genet 2003; 72: 340–350.
Almasy L, Blangero J . Multipoint quantitative-trait linkage analysis in general pedigrees. Am J Hum Genet 1998; 62: 1198–1211.
Arita Y, Kihara S, Ouchi N, Takahashi M, Maeda K, Miyagawa J et al. Paradoxical decrease of an adipose-specific protein, adiponectin, in obesity. Biochem Biophys Res Commun 1999; 257: 79–83.
Palmer LJ, Buxbaum SG, Larkin EK, Patel SR, Elston RC, Tishler PV et al. Whole genome scan for obstructive sleep apnea and obesity in African-American families. Am J Respir Crit Care Med 2004; 169: 1314–1321.
Tang W, Hong Y, Province MA, Rich SS, Hopkins PN, Arnett DK et al. Familial clustering for features of the metabolic syndrome: the National Heart, Lung, and Blood Institute (NHLBI) Family Heart Study. Diabetes Care 2006; 29: 631–636.
O'Donnell CP, Schaub CD, Haines AS, Berkowitz DE, Tankersley CG, Schwartz AR et al. Leptin prevents respiratory depression in obesity. Am J Respir Crit Care Med 1999; 159: 1477–1484.
Menzaghi C, Coco A, Salvemini L, Thompson R, De Cosmo S, Doria A et al. Heritability of serum resistin and its genetic correlation with insulin resistance-related features in nondiabetic Caucasians. J Clin Endocrinol Metab 2006; 91: 2792–2795.
Comuzzie AG, Hixson JE, Almasy L, Mitchell BD, Mahaney MC, Dyer TD et al. A major quantitative trait locus determining serum leptin levels and fat mass is located on human chromosome 2. Nat Genet 1997; 15: 273–276.
Comuzzie AG, Funahashi T, Sonnenberg G, Martin LJ, Jacob HJ, Black AE et al. The genetic basis of plasma variation in adiponectin, a global endophenotype for obesity and the metabolic syndrome. J Clin Endocrinol Metab 2001; 86: 4321–4325.
Larkin EK, Patel SR, Elston RC, Redline S . Linkage analyses of sleep disordered breathing using alternative measures of the apnea hypopnea index (AHI) (abstract). Proc Am Thorac Soc 2006; 3: A568.
Acknowledgements
This study was supported by National Institutes of Health Grants HL081385, HL046380 and M01 RR00080.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Patel, S., Larkin, E. & Redline, S. Shared genetic basis for obstructive sleep apnea and adiposity measures. Int J Obes 32, 795–800 (2008). https://doi.org/10.1038/sj.ijo.0803803
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ijo.0803803
Keywords
This article is cited by
-
Whole-genome association analyses of sleep-disordered breathing phenotypes in the NHLBI TOPMed program
Genome Medicine (2021)
-
Genetic influences on the onset of obstructive sleep apnoea and daytime sleepiness: a twin study
Respiratory Research (2019)
-
Quality of sleep and risk for obstructive sleep apnoea in ambulant individuals with type 2 diabetes mellitus at a tertiary referral hospital in Kenya: a cross-sectional, comparative study
BMC Endocrine Disorders (2017)
-
Laparoscopic Gastric Banding in Obese Patients with Sleep Apnea: A 3-Year Controlled Study and Follow-up After 10 Years
Obesity Surgery (2015)
-
Heart Rate Variability and Cardio-respiratory Coupling During Sleep in Patients Prior to Bariatric Surgery
Obesity Surgery (2014)