Abstract
Objective:
The magnitude of the contribution of childbearing to the development of obesity is not entirely understood. Published studies on postpartum weight retention focus on risk factors and clinical interventions. Pooled estimates of postpartum weight retention have not been reported. We summarized the existing evidence of the natural history of postpartum weight retention and estimated the extent of time after delivery that weight retention is attributable to pregnancy.
Design:
Systematic review and meta-analysis of qualitatively homogeneous studies.
Data sources:
Medline search of published studies between January 1995 and August 2005; bibliography of candidate studies.
Review methods:
Eligibility: Observational studies and control groups of randomized controlled trials. Independent review and data abstraction including study design, subject characteristics, women's weight and study quality by two reviewers. Meta-analysis of average postpartum weight retention at different points in time after delivery. Sensitivity analysis for study specific covariates using meta-regression.
Results:
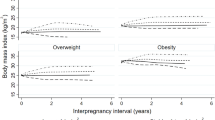
Twenty-five studies describing 21 cohorts met eligibility criteria. Sixteen studies appeared homogeneous enough to be included in the meta-analysis. Average postpartum weight retention decreased continuously until 12 months postpartum (6 weeks: 2.42 (95% confidence interval (95% CI): 2.32–2.52) Body mass index (BMI), 6 months: 1.14 (95% CI: 1.04–1.25) BMI, 12 months: 0.46 (95% CI: 0.38–0.54) BMI). Postpartum weight retention was 0.46 BMI lower in studies with follow-up rate ⩾80% at 6 weeks postpartum compared to studies with lower follow-up rate (P<0.01).
Conclusion:
Published studies consistently showed a decline in mean body weight within the first year postpartum. Data on body weight later than 12 months postpartum are scarce. The published evidence suggests a re-increase in body weight. As there are rather lifestyle-related than biological reasons for an increase in body weight after one year postpartum, we suggest using the term ‘postpartum weight retention’ exclusively within a limited period (for example, up to 12–18 months) postpartum.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Williamson DF, Kahn HS, Remington PL, Anda RF . The 10-year incidence of overweight and major weight gain in US adults. Arch Intern Med 1990; 150: 665–672.
Ogden CL, Flegal KM, Carroll MD, Johnson CL . Prevalence and trends in overweight among US children and adolescents, 1999–2000. JAMA 2002; 288: 1728–1732.
Flegal KM, Carroll MD, Kuczmarski RJ, Johnson CL . Overweight and obesity in the United States: prevalence and trends, 1960–1994. Int J Obes Relat Metab Disord 1998; 22: 39–47.
Gunderson EP, Abrams B . Epidemiology of gestational weight gain and body weight changes after pregnancy. Epidemiol Rev 2000; 22: 261–274.
Öhlin A, Rössner S . Factors related to body weight changes during and after pregnancy: the Stockholm Pregnancy and Weight Development Study. Obes Res 1996; 4: 271–276.
Kral JG . Preventing and treating obesity in girls and young women to curb the epidemic. Obes Res 2004; 12: 1539–1546.
Linné Y, Rössner S . Interrelationships between weight development and weight retention in subsequent pregnancies: the SPAWN study. Acta Obstet Gynecol Scand 2003; 82: 318–325.
Committee on Nutritional Status during Pregnancy and Lactation IOM. Effects of Gestational Weight Gain on Outcome in Singleton Pregnancies. In: Institute of Medicine (ed), Nutrition During Pregnancy: Part I: Weight Gain, Part II: Nutrient Supplements (1990). National Academy Press: Washington, DC, 1990. pp 176–205.
Cartwright Y . Battling excess postpartum weight retention. J Am Diet Assoc 2004; 104: 1108–1109.
Walker LO . Predictors of weight gain at 6 and 18 months after childbirth: a pilot study. J Obstet Gynecol Neonatal Nurs 1996; 25: 39–48.
Öhlin A, Rössner S . Trends in eating patterns, physical activity and socio-demographic factors in relation to postpartum body weight development. Br J Nutr 1994; 71: 457–470.
Linné Y, Rössner S . [Easy to remain overweight after pregnancy]. Lakartidningen 2003; 100: 4091–4095.
Devine CM, Bove CF, Olson CM . Continuity and change in women's weight orientations and lifestyle practices through pregnancy and the postpartum period: the influence of life course trajectories and transitional events. Soc Sci Med 2000; 50: 567–582.
Schauberger CW, Rooney BL, Brimer LM . Factors that influence weight loss in the puerperium. Obstet Gynecol 1992; 79: 424–429.
Gore SA, Brown DM, West DS . The role of postpartum weight retention in obesity among women: a review of the evidence. Ann Behav Med 2003; 26: 149–159.
Siega-Riz AM, Evenson KR, Dole N . Pregnancy-related weight gain – a link to obesity? Nutr Rev 2004; 62: S105–S111.
Egger M, Smith DE, Altman DG . Systematic Reviews in Healthcare: Meta-Analysis in Context. BMJ Books: London, 2001.
Greenland S . Quantitative methods in the review of epidemiologic literature. Epidemiol Rev 1987; 9: 1–30.
Stata Corporation. Stata 8 Reference Manual. College Station: TX, 2003.
Benichou J, Gail MH . Methods of inference for estimates of absolute risk derived from population-based case–control studies. Biometrics 1995; 51: 182–194.
Stata Corporation. Stata Statistical Software: Release 8.0. Stata Corporation, College Station: TX, 2002.
Boardley DJ, Sargent RG, Coker AL, Hussey JR, Sharpe PA . The relationship between diet, activity, and other factors, and postpartum weight change by race. Obstet Gynecol 1995; 86: 834–838.
Butte NF, Ellis KJ, Wong WW, Hopkinson JM, Smith EO . Composition of gestational weight gain impacts maternal fat retention and infant birth weight. Am J Obstet Gynecol 2003; 189: 1423–1432.
Gunderson EP, Abrams B, Selvin S . Does the pattern of postpartum weight change differ according to pregravid body size? Int J Obes Relat Metab Disord 2001; 25: 853–862.
Harris HE, Ellison GT, Holliday M . Is there an independent association between parity and maternal weight gain? Ann Hum Biol 1997; 24: 507–519.
Harris HE, Ellison GT, Holliday M, Lucassen E . The impact of pregnancy on the long-term weight gain of primiparous women in England. Int J Obes Relat Metab Disord 1997; 21: 747–755.
Harris HE, Ellison GT, Clement S . Do the psychosocial and behavioral changes that accompany motherhood influence the impact of pregnancy on long-term weight gain? J Psychosom Obstet Gynaecol 1999; 20: 65–79.
Harris HE, Ellison GT, Clement S . Relative importance of heritable characteristics and lifestyle in the development of maternal obesity. J Epidemiol Community Health 1999; 53: 66–74.
Janney CA, Zhang D, Sowers M . Lactation and weight retention. Am J Clin Nutr 1997; 66: 1116–1124.
Jenkin W, Tiggemann M . Psychological effects of weight retained after pregnancy. Women Health 1997; 25: 89–98.
Kac G, Benicio MH, Velasquez-Melendez G, Valente JG, Struchiner CJ . Breastfeeding and postpartum weight retention in a cohort of Brazilian women. Am J Clin Nutr 2004; 79: 487–493.
Kac G, D'Aquino Benicio MH, Valente JG, Velasquez-Melendez G . Postpartum weight retention among women in Rio de Janeiro: a follow-up study. Cad Saude Publica 2003; 19 (Suppl 1): S149–S161.
Kac G, Benicio MH, Velasquez-Melendez G, Valente JG, Struchiner CJ . Gestational weight gain and prepregnancy weight influence postpartum weight retention in a cohort of Brazilian women. J Nutr 2004; 134: 661–666.
Kanadys WM . [Postpartum body weight change]. Ginekol Pol 1998; 69: 570–574.
Lederman SA, Alfasi G, Deckelbaum RJ . Pregnancy-associated obesity in black women in New York city. Matern Child Health J 2002; 6: 37–42.
Linné Y, Dye L, Barkeling B, Rössner S . Long-term weight development in women: a 15-year follow-up of the effects of pregnancy. Obes Res 2004; 12: 1166–1178.
Muscati SK, Gray-Donald K, Koski KG . Timing of weight gain during pregnancy: promoting fetal growth and minimizing maternal weight retention. Int J Obes Relat Metab Disord 1996; 20: 526–532.
Olson CM, Strawderman MS, Hinton PS, Pearson TA . Gestational weight gain and postpartum behaviors associated with weight change from early pregnancy to 1 y postpartum. Int J Obes Relat Metab Disord 2003; 27: 117–127.
Polley BA, Wing RR, Sims CJ . Randomized controlled trial to prevent excessive weight gain in pregnant women. Int J Obes Relat Metab Disord 2002; 26: 1494–1502.
Rooney BL, Schauberger CW . Excess pregnancy weight gain and long-term obesity: one decade later. Obstet Gynecol 2002; 100: 245–252.
Soltani H, Fraser RB . A longitudinal study of maternal anthropometric changes in normal weight, overweight and obese women during pregnancy and postpartum. Br J Nutr 2000; 84: 95–101.
Stein TP, Scholl TO, Schluter MD, Schroeder CM . Plasma leptin influences gestational weight gain and postpartum weight retention. Am J Clin Nutr 1998; 68: 1236–1240.
Thorsdottir I, Birgisdottir BE . Different weight gain in women of normal weight before pregnancy: postpartum weight and birth weight. Obstet Gynecol 1998; 92: 377–383.
To WW, Cheung W . The relationship between weight gain in pregnancy, birth-weight and postpartum weight retention. Aust N Z J Obstet Gynaecol 1998; 38: 176–179.
Walker LO, Timmerman GM, Sterling BS, Kim M, Dickson P . Do low-income women attain their pre-pregnant weight by the 6th week of postpartum? Ethn Dis 2004; 14: 119–126.
Carter AS, Baker CW, Brownell KD . Body mass index, eating attitudes, and symptoms of depression and anxiety in pregnancy and the postpartum period. Psychosom Med 2000; 62: 264–270.
Öhlin A, Rössner S . Maternal body weight development after pregnancy. Int J Obes Relat Metab Disord 1990; 14: 159–173.
O'Toole ML, Sawicki MA, Artal R . Structured diet and physical activity prevent postpartum weight retention. J Womens Health (Larchmt) 2003; 12: 991–998.
Colditz GA . Economic costs of obesity. Am J Clin Nutr 1992; 55: 503S–507S.
Colditz GA, Willett WC, Rotnitzky A, Manson JE . Weight gain as a risk factor for clinical diabetes mellitus in women. Ann Intern Med 1995; 122: 481–486.
Manson JE, Willett WC, Stampfer MJ, Colditz GA, Hunter DJ, Hankinson SE et al. Body weight and mortality among women. N Engl J Med 1995; 333: 677–685.
McGinnis JM, Foege WH . Actual causes of death in the United States. JAMA 1993; 270: 2207–2212.
Rookus MA, Rokebrand P, Burema J, Deurenberg P . The effect of pregnancy on the body mass index 9 months postpartum in 49 women. Int J Obes Relat Metab Disord 1987; 11: 609–618.
Harris HE, Ellison GT, Richter LM, de Wet T, Levin J . Are overweight women at increased risk of obesity following pregnancy? Br J Nutr 1998; 79: 489–494.
Acknowledgements
We thank Joanna Brzeska for translating the article by Kanadys et al. (1998). She did not receive money for her assistance.
Author information
Authors and Affiliations
Corresponding author
Additional information
Conflict of interest
All authors hereby give consent to publication of this manuscript in the International Journal Of Obesity. None of the contributing authors received any funding for this work or has any other competing interests (that is relevant patents, financial and business relationships to sponsors, companies related to the research or the outcome of the studies in the manuscript) to declare.
Natalie M Schmitt: Conception, design, literature search, data abstraction, interpretation of data, drafting the manuscript, final approval of the manuscript to be published. Wanda K Nicholson: Conception, interpretation of data, revision of the manuscript, final approval of the manuscript to be published. Jochen Schmitt: Conception, literature search, data abstraction, interpretation of data, statistical analysis, revision of the manuscript, final approval of the manuscript to be published.
Rights and permissions
About this article
Cite this article
Schmitt, N., Nicholson, W. & Schmitt, J. The association of pregnancy and the development of obesity – results of a systematic review and meta-analysis on the natural history of postpartum weight retention. Int J Obes 31, 1642–1651 (2007). https://doi.org/10.1038/sj.ijo.0803655
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ijo.0803655
Keywords
This article is cited by
-
Monitoring gestational weight gain: setting up a regional surveillance system in Italy
BMC Public Health (2023)
-
Interpregnancy weight gain and childhood obesity: analysis of a UK population-based cohort
International Journal of Obesity (2022)
-
Food consumption and undernutrition variations among mothers during the post-harvest and lean seasons in Amoron'i Mania Region, Madagascar
BMC Public Health (2019)
-
The duration of the interpregnancy interval in multiparous women and maternal weight gain between pregnancies: findings from a UK population-based cohort
Scientific Reports (2019)
-
The Association between Neighborhood Environments and Physical Activity from Pregnancy to Postpartum: a Prospective Cohort Study
Journal of Urban Health (2019)