Abstract
Background:
People with obesity and/or the metabolic syndrome have an increased risk for developing diabetes and cardiovascular disease and may have low adiponectin levels. The obesity associated with Prader–Willi syndrome (PWS) would be expected to have similar complications. However, it was recently reported that, despite their adiposity, people with PWS have reduced visceral fat and are less likely to develop diabetes mellitus or the metabolic syndrome compared with people with simple obesity.
Objective:
To determine if plasma adiponectin levels and other variables relevant to diabetes and cardiovascular risk are different in a cohort of PWS subjects with known genetic subtypes compared with age-, sex- and weight-matched control subjects.
Results:
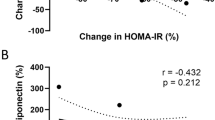
Fasting plasma glucose, C-peptide, triglycerides, leptin and cholesterol levels were similar in PWS and obese subjects. Our 20 PWS subjects (mean age=27.7 years) had higher percent body fat (54.1 vs 48.5%) determined by DEXA measurements and lower percent lean mass (45.9 vs 51.5%) compared with 14 obese controls (mean age=26.9 year). Plasma adiponectin levels were significantly higher in PWS (15.5±8.2 μg/ml) than in obese controls (7.5±2.7 μg/ml). A significant positive correlation was found with insulin sensitivity in PWS subjects (r=0.75, P=0.0003) but not in obese controls (r=0.36, P=0.20).
Discussion:
Our study confirmed an earlier observation of higher adiponectin levels in PWS subjects and less insulin resistance proportionate to their obesity status than found in subjects with simple obesity. Furthermore, no differences were seen in PWS subjects with the chromosome 15 deletion or maternal disomy 15. The reported excessive visceral adiposity in subjects with simple obesity compared with PWS may be associated with decreased production and lower circulating levels of adiponectin.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Butler MG . Prader-Willi syndrome: current understanding of cause and diagnosis. Am J Med Genet 1990; 35: 319–332.
Cassidy SB . Prader-Willi syndrome. J Med Genet 1997; 34: 917–923.
Butler MG, Thompson T . Prader-Willi syndrome: clinical and genetic findings. Endocrinology 2000; 10: 35–165.
Mascari MJ, Gottlieb W, Rogan PK, Butler MG, Waller DA, Armour JA et al. The frequency of uniparental disomy in Prader-Willi syndrome. Implications for molecular diagnosis. N Engl J Med 1992; 326: 1599–1607.
Glenn CC, Driscoll DJ, Yang TP, Nicholls RD . Genomic imprinting: potential function and mechanisms revealed by the Prader-Willi and Angelman syndromes. Mol Hum Reprod 1997; 3: 321–332.
Robinson WP, Kuchinka BD, Bernasconi F, Petersen MB, Schulze A, Brondum-Nielsen K et al. Maternal meiosis I non-disjunction of chromosome 15: dependence of the maternal age effect on level of recombination. Hum Mol Genet 1998; 7: 1011–1019.
Ohta T, Gray TA, Rogan PK, Buiting K, Gabriel JM, Saitoh S et al. Imprinting-mutation mechanisms in Prader-Willi syndrome. Am J Hum Genet 1999; 64: 397–413.
Buiting K, Gross S, Lich C, Gillessen-Kaesbach G, el-Maarri O, Horsthemke B . Epimutations in Prader-Willi and Angelman syndromes: a molecular study of 136 patients with an imprinting defect. Am J Hum Genet 2003; 72: 571–577.
Weyer C, Funahashi T, Tanaka S, Hotta K, Matsuzawa Y, Pratley RE et al. Hypoadiponectinemia in obesity and type 2 diabetes: close association with insulin resistance and hyperinsulinemia. J Clin Endocrinol Metab 2001; 86: 1930–1935.
Argiles JM, Lopez-Soriano J, Almendro V, Busquets S, Lopez-Soriano FJ . Cross-talk between skeletal muscle and adipose tissue: a link with obesity? Med Res Rev 2004.
Kershaw EE, Flier JS . Adipose tissue as an endocrine organ. J Clin Endocrinol Metab 2004; 89: 2548–2556.
Meier U, Gressner AM . Endocrine regulation of energy metabolism: review of pathobiochemical and clinical chemical aspects of leptin, ghrelin, adiponectin, and resistin. Clin Chem 2004; 50: 1511–1525.
Phillips SA, Ciaraldi TP, Kong AP, Bandukwala R, Aroda V, Carter L et al. Modulation of circulating and adipose tissue adiponectin levels by antidiabetic therapy. Diabetes 2003; 52: 667–674.
Goldstone AP, Thomas EL, Brynes AE, Bell JD, Frost G, Saeed N et al. Visceral adipose tissue and metabolic complications of obesity are reduced in Prader-Willi syndrome female adults: evidence for novel influences on body fat distribution. J Clin Endocrinol Metab 2001; 86: 4330–4338.
Hoybye C, Bruun JM, Richelsen B, Flyvbjerg A, Frystyk J . Serum adiponectin levels in adults with Prader-Willi syndrome are independent of anthropometrical parameters and do not change with GH treatment. Eur J Endocrinol 2004; 151: 457–461.
Katz A, Nambi SS, Mather K, Baron AD, Follmann DA, Sullivan G et al. Quantitative insulin sensitivity check index: a simple, accurate method for assessing insulin sensitivity in humans. J Clin Endocrinol Metab 2000; 85: 2402–2410.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC . Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985; 28: 412–419.
Mazess RB, Barden HS, Bisek JP, Hanson J . Dual-energy X-ray absorptiometry for total-body and regional bone-mineral and soft-tissue composition. Am J Clin Nutr 1990; 51: 1106–1112.
Grundy SM . Hypertriglyceridemia, insulin resistance, and the metabolic syndrome. Am J Cardiol 1999; 83: 25F–29F.
Haffner SM, Valdez RA, Hazuda HP, Mitchell BD, Morales PA, Stern MP . Prospective analysis of the insulin-resistance syndrome (syndrome X). Diabetes 1992; 41: 715–722.
Isomaa B, Almgren P, Tuomi T, Forsen B, Lahti K, Nissen M et al. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care 2001; 24: 683–689.
Weiss R, Dufour S, Groszmann A, Petersen K, Dziura J, Taksali SE et al. Low adiponectin levels in adolescent obesity: a marker of increased intramyocellular lipid accumulation. J Clin Endocrinol Metab 2003; 88: 2014–2018.
Bacha F, Saad R, Gungor N, Arslanian SA . Adiponectin in youth: relationship to visceral adiposity, insulin sensitivity, and beta-cell function. Diabetes Care 2004; 27: 547–552.
Ford ES, Giles WH, Dietz WH . Prevalence of the metabolic syndrome among US adults: findings from the third National Health and Nutrition Examination Survey. JAMA 2002; 287: 356–359.
Lebovitz H . Insulin resistance: definition and consequences. Exp Clin Endocrinol Diabetes 2001; 109 (Suppl 2): S135–S148.
Martin A, State M, Koenig K, Schultz R, Dykens EM, Cassidy SB et al. Prader-Willi syndrome. Am J Psychiatry 1998; 155: 1265–1273.
Talebizadeh Z, Butler M . Insulin resistance and obesity-related factors in Prader-Willi syndrome: Comparison with obese subjects. Clin Genet 2005; 67: 230–239.
Meaney FJ, Butler MG . Characterization of obesity in the Prader-Labhart-Willi syndrome: Fatness patterning. Med Anthropo Quart 1989; 3: 294–305.
Acknowledgements
We thank Brian Sheridan at the Regional Biochemistry Laboratory, Royal Victoria Hospital, Belfast, Northern Ireland, for measuring plasma insulin and C-peptide and Karen Brezner for her assistance in processing the plasma samples. Support was provided by Grant PO1HD30329 and RO1HD41672 from the National Institutes of Health; Children's Mercy Hospitals Physician Scientist Award (01.4871); and the Hall Family Foundation (01.3905) to MGB as well as Grant DK37373 from the National Institutes of Health to SPK.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kennedy, L., Bittel, D., Kibiryeva, N. et al. Circulating adiponectin levels, body composition and obesity-related variables in Prader–Willi syndrome: comparison with obese subjects. Int J Obes 30, 382–387 (2006). https://doi.org/10.1038/sj.ijo.0803115
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ijo.0803115
Keywords
This article is cited by
-
Do patients with Prader–Willi syndrome have favorable glucose metabolism?
Orphanet Journal of Rare Diseases (2022)
-
Irisin levels in genetic and essential obesity: clues for a potential dual role
Scientific Reports (2020)
-
Excessive carbohydrate consumption and body mass index: the risk factors for type 2 diabetes mellitus in patients with Prader-Willi syndrome in Tamil Nadu population
The Journal of Basic and Applied Zoology (2018)
-
Body composition, adipokines, bone mineral density and bone remodeling markers in relation to IGF-1 levels in adults with Prader-Willi syndrome
International Journal of Pediatric Endocrinology (2018)
-
Prevalence and risk factors for type 2 diabetes mellitus with Prader–Willi syndrome: a single center experience
Orphanet Journal of Rare Diseases (2017)