Abstract
OBJECTIVE:
To assess the effectiveness of dietary interventions and exercise in long-term weight loss in overweight and obese people.
DESIGN:
A systematic review with meta-analysis.
SUBJECTS:
Overweight and obese adults—18 years old or older with body mass index (calculated as weight divided by the square of height in meters)>25.
DATA SOURCE:
Medline, Cochrane Library and Lilacs databases up to March 2003. Also, published reviews and all relevant studies and their reference lists were reviewed in search for other pertinent publications. No language restrictions were imposed.
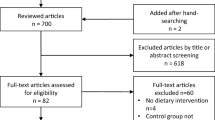
STUDY SELECTION:
Randomised clinical trials comparing diet and exercise interventions vs diet alone. All trials included a follow-up of 1 y after intervention.
DATA EXTRACTION:
Two reviewers independently abstracted data and evaluated the studies’ quality with criteria adapted from the Jadad Scale and the Delphi list.
DATA SYNTHESIS:
The estimate of the intervention's effect size was based on the differences between the comparison groups, and then the overall effect was calculated. A chi-squared test was used to assess statistical heterogeneity.
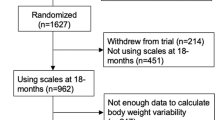
RESULTS:
A total of 33 trials evaluating diet, exercise or diet and exercise were found. Only 6 studies directly comparing diet and exercise vs diet alone were included (3 additional studies reporting repeated observations were excluded). The active intervention period ranged between 10 and 52 weeks across studies. Diet associated with exercise produced a 20% greater initial weight loss. (13 kg vs 9.9 kg; z=1.86—p=0.063, 95%CI). The combined intervention also resulted in a 20% greater sustained weight loss after 1 y (6.7 kg vs 4.5 kg; z=1.89—p=0.058, 95%CI) than diet alone. In both groups, almost half of the initial weight loss was regained after 1 y.
CONCLUSION:
Diet associated with exercise results in significant and clinically meaningful initial weight loss. This is partially sustained after 1 y.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
World Health Organization. Obesity: Preventing and Managing the Global Epidemic. Technical Report Series 894. WHO: Geneva; 2000.
National Heart Lung and Blood Institute (NHLBI). Clinical Guidelines on the identification, evaluation, and treatment of overweight and obesity in adults—the evidence report (Clinical Gdlns). Obes Res 1998; 6: 51S–209S.
Wadden TA . Treatment of obesity by moderate and severe caloric restriction. Results of clinical research trials. Ann Intern Med 1993; 119: 688–693.
Kramer FM, Jeffery RW, Forster JL, Snell MK . Long-term follow-up of behavioral treatment for obesity: patterns of weight regain among men and women. Int J Obes Relat Metab Disord 1989; 13: 123–136.
Brownell KD, Jefery RW . Improving long-term weight loss: pushing the limits of treatment. Behav Ther 1987; 18: 353–374.
Anderson JW, Kons EC, Frederich RC, Wood CL . Long-term weight loss maintenance: a meta-analysis of US studies. Am J Clin Nutr 2001; 74: 579–584.
Jadad A, Moore RA, Carrol D, Jenkinson C, Reynolds DJM, Gavaghan DJ, McQuay HJ . Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 1996; 17: 1–12.
Verhagen AP, de Vet HCW, de Bie RA, Kessels AGH, Boers M, Bouter LM, Knipschild PG . The Delphi List: a criteria list for quality assessment of randomized clinical trials for conducting systematic reviews developed by Delphi Consensus. J Clin Epidemiol 1998; 51: 1235–1241.
StataCorp. Stata Statistical Software: Release 6.0 College Station. Stata Corporation: TX; 1999.
Fisher LP, Van Belle G Biostatistics – a methodology for the health science John Wiley & Sons, Inc; New york; 1993.
Borg P, Kukkonen-Harjula K, Fogelholm M, Pasanen M . Effects of walking or resistance training on weight loss maintenance in obese, middle-aged men: a randomized trial. Int J Obes Relat Metab Disord 2002; 26: 676–683.
Fogelholm M, Kukkonen-Harjula K, Nenonen A, Pasanen M . Effects of walking training on weight maintenance after a very-low-energy diet in premenopausal obese women: a randomized controlled trial. Arch Intern Med 2000; 160: 2177–2184.
Wadden TA, Anderson DA, Foster GD . Two-year changes in lipids and lipoproteins associated with the maintenance of a 5–10% reduction in initial weight: some findings and some questions. Obes Res 1999; 7: 170–178.
Fogelholm M, Kukkonen-Harjula K, Oja P . Eating control and physical activity as determinants of short-term weight maintenance after a very-low-calorie diet among obese women. Int J Obes Relat Metab Disord 1999; 23: 203–210.
Andersen RE, Wadden TA, Bartlett SJ, Zemel B, Verde TJ, Franckowiak SC . Effects of lifestyle activity vs structured aerobic exercise in obese women: a randomized trial. JAMA 1999; 281: 335–340.
Weinstock RS, Dai H, Wadden TA . Diet and exercise in the treatment of obesity: effects of 3 interventions on insulin resistance. Arch Intern Med 1998; 158: 2477–2483.
Wadden TA, Vogt RA, Foster GD, Anderson DA . Exercise and the maintenance of weight loss: 1-year follow-up of a controlled clinical trial. J Consult Clin Psychol 1998; 66: 429–433.
Skender ML, Goodrick GK, Del Junco DJ, Reeves RS, Darnell L, Gotto AM, Foreyt JP . Comparison of 2-year weight loss trends in behavioral treatments of obesity: diet, exercise, and combination interventions. J Am Diet Assoc 1996; 96: 342–346.
Wing RR, Epstein LH, Paternostro-Bayles M, Kriska A, Nowalk MP, Gooding W . Exercise in a behavioural weight control programme for obese patients with Type 2 (non-insulin-dependent) diabetes. Diabetologia 1988; 31: 902–909.
Coutinho WF . Consenso Latino-americano de Obesidade: Até onde já Chegamos. Arq Bras Endocrinol Metab 1999; 43: 21–67.
Fogelholm M, Kukkonen-Harjula K . Does physical activity prevent weight gain—a systematic review. Obes Rev 2000; 1: 95–111.
Bennett GA . An evaluation of self-instructional training in the treatment of obesity. Addict Behav 1986; 11: 125–134.
Bennett GA . Cognitive rehearsal in the treatment of obesity: a comparison against cue avoidance and social pressure. Addict Behav 1986; 11: 225–237.
Wadden TA, Stunkard AJ . Controlled trial of very-low-calorie diet, behavior therapy, and their combination in the treatment of obesity. J Cons Clin Psychol 1986; 54: 482–488.
Wing R, Epstein L . Prescribed level of caloric restriction in behavioral weight loss programs. Addict Behav 1981; 6: 139–144.
Wing R, Epstein L, Shapira B . The effect of increasing initial weight loss with the Scardsale diet on subsequent weight loss in a behavioral treatment program. J Cons Clin Psychol 1982; 50: 446–447.
Adams SO, Grady KE, Lund AK, Mukaida C, Wolk CH . Weight loss: long-term results in an ambulatory setting. J Am Diet Assoc 1983; 83: 306–310.
McTigue KM, Harris R, Hemphill B, Lux L, Sutton S, Bunton AJ, Lohr KN . Screening and interventions for obesity in adults: summary of the evidence for the U.S. Preventive Service Task Force. Ann Intern Med 2003; 139: 933–942.
Miller WC, Koceja DM, Hamilton EJ . A meta-analysis of the past 25 years of weight loss research using diet, execise or diet plus exercise intervention. Int J Obes Relat Metab Disord 1997; 21: 941–947.
Alderson P, Green S, Higgins JPT (eds). Locating and selecting studies for reviews. In Cochrane Reviewers’ Handbook 4.2.2, [updated December 2003]; Section 5. http://www.cochrane.org/resources/handbook/hbook.htm (accessed 31st January 2004).
Glenny AM, O’Meara S, Melville A, Sheldon TA, Wilson C . The treatment and prevention of obesity: a systematic review of the literature. Int J Obes Relat Metab Disord 1997; 21: 715–737.
Alderson P, Green S, Higgins JPT (eds). Analysing and presenting results. In: Cochrane Reviewers’ Handbook 4.2.2, [updated December 2003]; Section 8. http://www.cochrane.org/resources/handbook/hbook.htm (accessed 31st January 2004).
King AC, Frey-Hewitt B, Dreon DM, Wood PD . Diet vs exercise in weight maintenance. Arch Intern Med 1989; 149: 2741–2746.
Jeffery RW, Wing RR . Long-term effects of interventions for weight loss using food provision and monetary incentives. J Consult Clin Psychol 1995; 63: 793–796.
Pavlou KN, Krey S, Steffee WP . Exercise as an adjunct to weight loss and maintenance in moderately obese subjects. Am J Clin Nutr 1989; 49 (Suppl 5): 1115–1123.
Perri MG, McAdoo WG, McAllister DA, Lauer JB, Yancey DZ . Enhancing the efficacy of behavior therapy for obesity: effects of aerobic exercise and a multicomponent maintenance program. J Cons Clin Psychol 1986; 54: 670–675.
Sikand G, Kondo A, Foyret JP, Jones PH . Two-year follow-up of patients treated with very-low-calorie diet and exercise training. J Am Diet Assoc 1988; 88: 487–488.
Tuomilehto J, Lindstrom J, Eriksson JG, Valle TT, Hamalainen H, Ilanne-Parikka P, Keinanen-Kiukaanniemi S, Laakso M, Louheranta A, Rastas M, Salminen V, Uusitupa M ; Finnish Diabetes Prevention Study Group . Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 2001; 344: 1343–1350.
Uusitupa M, Louheranta A, Lindstrom J, Valle T, Sundvall J, Eriksson J, Tuomilehto J . The Finnish Diabetes Prevention Study. Br J Nutr 2000; 83 (Suppl 1): S137–S142.
van Dale D, Saris WH, ten Hoor F . Weight maintenance and resting metabolic rate 18–40 months after a diet/exercise treatment. Int J Obes 1990; 14: 347–359.
Bacon L, Keim NL, Van Loan MD, Derricote M, Gale B, Kazaks A, Stern JS . Evaluating a ‘non-diet’ wellness intervention for improvement of metabolic fitness, psychological well-being and eating and activity behaviors. Int J Obes Relat Metab Disord 2002; 26: 854–865.
Blackburn GL, Kanders BS, Lavin PT, Keller SD, Whatley J . The effect of aspartame as part of a multidisciplinary weight-control program on short- and long-term control of body weight. Am J Clin Nutr 1997; 65: 409–418.
Ditschuneit HH, Flechtner-Mors M, Johnson TD, Adler G . Metabolic and weight-loss effects of a long-term dietary intervention in obese patients. Am J Clin Nutr 1999; 69: 198–204.
Ditschuneit HH, Flechtner-Mors M . Value of structured meals for weight management: risk factors and long-term weight maintenance. Obes Res 2001; 9 (Suppl 4): 284S–289S.
Ditschuneit HH, Frier HI, Flechtner-Mors M . Lipoprotein responses to weight loss and weight maintenance in high-risk obese subjects. Eur J Clin Nutr 2002; 56: 264–270.
Flechtner-Mors M, Ditschuneit HH, Johnson TD, Suchard MA, Adler G . Metabolic and weight loss effects of long-term dietary intervention in obese patients: four-year results. Obes Res 2000; 8: 399–402.
Hakala P . Weight reduction programmes at a rehabilitation centre and a health centre based on group counselling and individual support: short- and long-term follow-up study. Int J Obes Relat Metab Disord 1994; 18: 483–489.
Hakala P, Karvetti RL, Ronnemaa T . Group vs individual weight reduction programmes in the treatment of severe obesity – a five year follow-up study. Int J Obes Relat Metab Disord 1993; 17: 97–102.
Pascale RW, Wing RR, Butler BA, Mullen M, Bononi P . Effects of a behavioral weight loss program stressing calorie restriction vs calorie plus fat restriction in obese individuals with NIDDM or a family history of diabetes. Diabetes Care 1995; 18: 1241–1248.
Pasman WJ, Westerterp-Plantenga MS, Muls E, Vansant G, van Ree J, Saris WH . The effectiveness of long-term fibre supplementation on weight maintenance in weight-reduced women. Int J Obes Relat Metab Disord 1997; 21: 548–555.
Ryttig KR, Flaten H, Rossner S . Long-term effects of a very low calorie diet (Nutrilett) in obesity treatment. A prospective, randomized, comparison between VLCD and a hypocaloric diet+behavior modification and their combination. Int J Obes Relat Metab Disord 1997; 21: 574–579.
Schlundt DG, Hill JO, Pope-Cordle J, Arnold D, Virts KL, Katahn M . Randomized evaluation of a low fat ad libitum carbohydrate diet for weight reduction. Int J Obes Relat Metab Disord 1993; 17: 623–629.
Sheppard L, Kristal AR, Kushi LH . Weight loss in women participating in a randomized trial of low-fat diets. Am J Clin Nutr 1991; 54: 821–828.
Swinburn BA, Metcalf PA, Ley SJ . Long-term (5-year) effects of a reduced-fat diet intervention in individuals with glucose intolerance. Diabetes Care 2001; 24: 619–624.
Torgerson JS, Lissner L, Lindroos AK, Kruijer H, Sjostrom L . VLCD plus dietary and behavioural support vs support alone in the treatment of severe obesity. A randomised two-year clinical trial. Int J Obes Relat Metab Disord 1997; 21: 987–994.
Wing RR, Blair E, Marcus M, Epstein LH, Harvey J . Year-long weight loss treatment for obese patients with type II diabetes: does including an intermittent very-low-calorie diet improve outcome? Am J Med 1994; 97: 354–362.
Wing RR, Marcus MD, Salata R, Epstein LH, Miaskiewicz S, Blair EH . Effects of a very-low-calorie diet on long-term glycemic control in obese type 2 diabetic subjects. Arch Intern Med 1991; 151: 1334–1340.
Acknowledgements
The authors thank: Rosely Sichieri, MD, PhD, Instituto de Medicina Social—Universidade do Estado do Rio de Janeiro; and Charles André, MD, PhD, Universidade Federal do Rio de Janeiro for valuable suggestions.
Author information
Authors and Affiliations
Corresponding author
Appendix A
Appendix A
Rights and permissions
About this article
Cite this article
Curioni, C., Lourenço, P. Long-term weight loss after diet and exercise: a systematic review. Int J Obes 29, 1168–1174 (2005). https://doi.org/10.1038/sj.ijo.0803015
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ijo.0803015
Keywords
This article is cited by
-
Ventricular Remodeling Following Metabolic and Bariatric Surgery Decreases Need for Heart Transplantation: A Predictive Model
Obesity Surgery (2024)
-
Sleeve Gastrectomy Reduces the Need for Liver Transplantation in Patients with Obesity and Non-Alcoholic Steatohepatitis: a Predictive Model
Obesity Surgery (2024)
-
Effect of instruction and experience on students’ learning strategies
Metacognition and Learning (2024)
-
Association between the use of weight management strategies and weight change among Australian adults over 12 months: an observational study
BMC Public Health (2023)
-
Eating behavior dimensions and 9-year weight loss maintenance: a sub-study of the Finnish Diabetes prevention study
International Journal of Obesity (2023)