Abstract
OBJECTIVE: We assessed the relationships between four circulating acute phase proteins and the circulating and adipose tissue levels of three adipocytokines.
SUBJECTS: In all, 15 nondiabetic obese women with a body mass index (BMI) above 32 kg/m2 were investigated.
METHOD: Circulating concentrations of C-reactive protein (CRP), alpha 1 acid glycoprotein (AAG), fibrinogen, alpha 1 antitrypsin and both circulating and adipose tissue levels of interleukin (IL)-6, tumor necrosis factor (TNF)α and leptin were measured by either nephelometry or enzyme-linked immunosorbent assay.
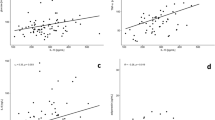
RESULTS: We found a strong positive correlation between both circulating and adipose tissue levels of IL-6, TNFα and leptin and serum CRP levels. All these adipose tissue adipocytokines were also positively correlated with serum AAG levels. These correlations disappeared when adjusted for fat mass, suggesting that the relationship observed was dependent on fat amount.
CONCLUSION: Our results indicate a strong relationship between adipocytokines and inflammatory markers, and suggest that cytokines secreted by adipose tissue in obese subjects could play a role in increased inflammatory proteins secretion by the liver.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Ridker PM . Clinical application of C-reactive protein for cardiovascular disease detection and prevention. Circulation 2003; 107: 363–369.
Visser M, Bouter LM, McQuillan GM, Wener MH, Harris TB . Elevated C-reactive protein levels in overweight and obese adults. JAMA 1999; 282: 2131–2135.
Piéroni L, Bastard JP, Piton A, Khalil L, Hainque B, Jardel C . Interpretation of circulating C-reactive protein levels in adults: body mass index and gender are a must. Diabetes Metab 2003; 29: 133–138.
Castell JV, Gomez-Lechon MJ, David M, Fabra R, Trullenque R, Heinrich PC . Acute-phase response of human hepatocytes: regulation of acute-phase protein synthesis by interleukin-6. Hepatology 1990; 12: 1179–1186.
Bastard JP, Jardel C, Delattre J, Hainque B, Bruckert E, Oberlin F . Evidence for a link between adipose tissue interleukin-6 content and serum C-reactive protein concentrations in obese subjects. Circulation 1999; 99: 2221–2222.
Yudkin JS, Stehouwer CD, Emeis JJ, Coppack SW . C-reactive protein in healthy subjects: associations with obesity, insulin resistance, and endothelial dysfunction: a potential role for cytokines originating from adipose tissue? Arterioscler Thromb Vasc Biol 1999; 19: 972–978.
Maruna P, Gurlich R, Frasko R, Haluzik M . Serum leptin levels in septic men correlate well with C-reactive protein (CRP) and TNF-alpha but not with BMI. Physiol Res 2001; 50: 589–594.
Bullo M, Garcia-Lorda P, Megias I, Sals-Salvado J . Systemic inflammation, adipose tissue tumor necrosis factor, and leptin expression. Obes Res 2003; 11: 525–531.
Benedek IH, Blouin RA, McNamara PJ . Serum protein binding and the role of increased alpha 1-acid glycoprotein in moderately obese male subjects. Br J Clin Pharmacol 1984; 18: 941–946.
Pickup JC, Mattock MB, Chusney GD, Burt D . NIDDM as a disease of the innate immune system: association of acute-phase reactants and interleukin-6 with metabolic syndrome X. Diabetologia 1997; 40: 1286–1292.
Hanusch-Enserer U, Cauza E, Spak M, Dunky A, Rosen HR, Wolf H, Prager R, Eibl MM . Acute-phase response and immunological markers in morbid obese patients and patients following adjustable gastric banding. Int J Obes Relat Metab Disord 2003; 27: 355–361.
Bastard JP, Vidal H, Jardel C, Bruckert E, Robin D, Vallier P, Blondy P, Turpin G, Forest C, Hainque B . Subcutaneous adipose tissue expression of plasminogen activator inhibitor-1 gene during very low calorie diet in obese subjects. Int J Obes Relat Metab Disord 2000; 24: 70–74.
Bastard JP, Jardel C, Bruckert E, Blondy P, Capeau J, Laville M, Vidal H, Hainque B . Elevated levels of interleukin-6 are reduced in serum and subcutaneous adipose tissue of obese women after weight loss. J Clin Endocrinol Metab 2000; 85: 3338–3342.
Ridker PM, Rifai N, Rose L, Buring JE, Cook NR . Comparison of C-reactive protein and low-density lipoprotein cholesterol levels in the prediction of first cardiovascular events. N Engl J Med 2002; 347: 1557–1565.
Ridker PM, Buring JE, Cook NR, Rifai N . C-reactive protein, the metabolic syndrome, and risk of incident cardiovascular events. Circulation 2003; 107: 391–397.
Gomez-Ambrosi J, Salvador J, Paramo JA, Orbe J, de Irala J, Diez-Caballero A, Gil MJ, Cienfuegos JA, Fruhbeck G . Involvement of leptin in the association between percentage of body fat and cardiovascular risk factors. Clin Biochem 2002; 35: 315–320.
Weisberg SP, McCann D, Desai M, Rosenbaum M, Leibel RL, Ferrante Jr AW . Obesity is associated with macrophage accumulation in adipose tissue. J Clin Invest 2003; 112: 1796–1808.
Xu H, Barnes GT, Yang Q, Tan G, Yang D, Chou CJ, Sole J, Nichols A, Ross JS, Tartaglia LA, Chen H . Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance. J Clin Invest 2003; 112: 1821–1830.
Bastard JP, Maachi M, Tran Van Nhieu J, Jardel C, Bruckert E, Grimaldi A, Robert JJ, Capeau J, Hainque B . Adipose tissue IL-6 content correlates with resistance to insulin activation of glucose uptake both in vivo and in vitro. J Clin Endocrinol Metab 2002; 87: 2084–2089.
Hotamisligil GS . Molecular mechanisms of insulin resistance and the role of the adipocyte. Int J Obes Relat Metab Disord 2000; 24 (Suppl 4): S23–S27.
Lagathu C, Bastard JP, Auclair M, Maachi M, Capeau J, Caron M . Chronic interleukin-6 (IL-6) treatment increased IL-6 secretion and induced insulin resistance in adipocyte: prevention by rosiglitazone. Biochem Biophys Res Commun 2003; 311: 372–379.
Fain JN, Cheema PS, Bahouth SW, Hiler ML . Resistin release by human adipose tissue explants in primary culture. Biochem Biophys Res Commun 2002; 300: 674–678.
Pasceri V, Willerson JT, Yeh ET . Direct proinflammatory effect of C-reactive protein on human endothelial cells. Circulation 2000; 102: 2165–2168.
Yeh ET, Anderson HV, Pasceri V, Willerson JT . C-reactive protein: linking inflammation to cardiovascular complications. Circulation 2001; 104: 974–975.
Verma S, Li SH, Badiwala MV, Weisel RD, Fedak PW, Li RK, Dhillon B, Mickle DA . Endothelin antagonism and interleukin-6 inhibition attenuate the proatherogenic effects of C-reactive protein. Circulation 2002; 105: 1890–1896.
Wang CH, Li SH, Weisel RD, Fedak PW, Dumont AS, Szmitko P, Li RK, Mickle DA, Verma S . C-reactive protein upregulates angiotensin type 1 receptors in vascular smooth muscle. Circulation 2003; 107: 1783–1790.
Heilbronn LK, Noakes M, Clifton PM . Energy restriction and weight loss on very-low-fat diets reduce C-reactive protein concentrations in obese, healthy women. Artrioscler Thromb Vasc Biol 2001; 21: 968–970.
Tchernof A, Nolan A, Sites CK, Ades PA, Poehlman ET . Weight loss reduces C-reactive protein levels in obese postmenopausal women. Circulation 2002; 105: 564–569.
Ziccardi P, Nappo F, Giugliano G, Esposito K, Marfella R, Cioffi M, D'Andrea F, Molinari AM, Giugliano D . Reduction of inflammatory cytokine concentrations and improvement of endothelial functions in obese women after weight loss over one year. Circulation 2002; 105: 804–809.
Kopp HP, Kopp CW, Festa A, Krzyzanowska K, Kriwanek S, Minar E, Roka R, Schernthaner G . Impact of weight loss on inflammatory proteins and their association with the insulin resistance syndrome in morbidly obese patients. Arterioscler Thromb Vasc Biol 2003; 23: 1042–1047.
Esposito K, Pontillo A, Di Palo C, Giugliano G, Masella M, Marfella R, Giugliano D . Effect of weight loss and lifestyle changes on vascular inflammatory markers in obese women: a randomized trial. JAMA 2003; 289: 1799–1804.
Acknowledgements
This work was supported by grants from Le Ministère de la Santé (Programme Hospitalier de Recherche Clinique No. AOA94042) and INSERM.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Maachi, M., Piéroni, L., Bruckert, E. et al. Systemic low-grade inflammation is related to both circulating and adipose tissue TNFα, leptin and IL-6 levels in obese women. Int J Obes 28, 993–997 (2004). https://doi.org/10.1038/sj.ijo.0802718
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ijo.0802718
Keywords
This article is cited by
-
Impact of visceral adipose tissue on longevity and metabolic health: a comparative study of gene expression in perirenal and epididymal fat of Ames dwarf mice
GeroScience (2024)
-
Progranulin (PGRN) as a regulator of inflammation and a critical factor in the immunopathogenesis of cardiovascular diseases
Journal of Inflammation (2023)
-
Frailty is related to serum inflammageing markers: results from the VITAL study
Immunity & Ageing (2023)
-
Hepatocyte-specific fibroblast growth factor 21 overexpression ameliorates high-fat diet-induced obesity and liver steatosis in mice
Laboratory Investigation (2022)
-
Evaluation of serum semaphorin 3A and interleukin 6 levels in patients with pseudoexfoliation syndrome
International Ophthalmology (2022)