Abstract
OBJECTIVE: To assess whether overweight children and adolescents, who often have poor dietary habits, are at increased risk of iron deficiency (ID).
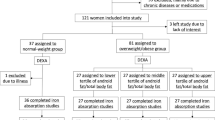
METHODS: The study sample included 321 children and adolescents followed in two endocrine centers in Israel between 1999 and 2001. The subjects were divided into three groups on the basis of body mass index (BMI) for age and gender as follows: group 1—BMI below 85th percentile (normal weight); group 2—BMI above 85th, but below 97th percentile (overweight); and group 3—BMI above 97th percentile (obese). ID was defined as iron levels <8 μmol/l (45 mcg/dl), and iron-deficiency anemia (IDA) was defined as ID and hemoglobin level below 2 standard deviation score (SDS) for the mean for age and gender.
RESULTS: Iron levels below 8 μmol/l (45 mcg/dl) were noted in 38.8% of the obese children and 12.1% of the overweight children, compared with 4.4% of the normal-weight group (P<0.001). There was a significant negative correlation of low iron levels with BMI SDS (r=−0.44, P<0.001), but not with age or gender. Among the children with ID, 26.6% also had IDA. Groups 1, 2, and 3 accounted for 6.7%, 35%, and 58.3% of the children with IDA, respectively.
CONCLUSIONS: ID is common in overweight and obese children. A significantly greater proportion of obese than normal-weight children have IDA. Insufficient dietary intake of iron, whether absolute or relative to body mass, and increased iron needs may be a result of unbalanced nutrition or repeated short-term restrictive diets. Because of potentially harmful effects of ID, obese children should be routinely screened and treated as necessary.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Saloojee H, Pettifor JM . Iron deficiency and impaired child development. Br Med J 2001; 15: 1377–1378.
Bhatia D, Seshadri S . Growth performance in anemia and following iron supplementation. Indian Pediatr 1993; 30: 195–200.
Barlow ES, Dietz WH . Obesity evaluation and treatment: expert committee recommendations, Vol 102. The Maternal and Child Health Bureau, Health Resources and Services Administration and the Department of Health and Human Services. Pediatrics, 1998. p E29.
American Academy of Pediatrics, Committee on Practice and Ambulatory Medicine. Recommendations for preventive pediatric health care. Pediatrics 1995; 96: 373–374.
http://www.cdc.gov/nchs/about/major/nhanes/growthcharts/charts.htm
Dixon WJ (Chief ed). BMDP statistical software. University of California Press: Berkeley, CA; 1993.
Popkin B . Obesity is a worldwide phenomenon. Nutr Rev 1998; 56: 106–114.
Halterman JS, Kaczorowski MJ, Aligne AC, Auigner P, Szilagyij PG . Iron deficiency and cognitive achievement among school-aged children and adolescents in the United States. Pediatrics 2001; 107: 1381–1386.
Hinton PS, Giordano C, Brownlie T, Haas JD . Iron supplementation improves endurance after training in iron-depleted, non-anemic women. J Appl Physiol 2000; 888: 1103–1111.
Andrews NC . Disorders of iron metabolism. N Engl J Med 1999; 341: 1986–1995.
Conrad ME, Umbreit JN . A concise review: iron absorption—the mucin–mobilferrin–integrin pathway. A competitive pathway for metal absorption. Am J Hematol 1993; 42: 67.
Beguin Y, Grek V, Weber G, Sautois B, Paquot N, Pereira M, Scheen A, Lefebvre P, Fillet G . Acute functional iron deficiency in obese subjects during a very-low-energy all-protein diet. Am J Clin Nutr 1997; 66: 75–79.
Failla ML, Kennedy ML, Chen ML . Iron metabolism in genetically obese (ob/ob) mice. J Nutr 1988; 118: 46–51.
Gibson RS, MacDonald AC, Smit-Vanderkooy PD . Serum ferritin and dietary iron parameters in a sample of Canadian preschool children. J Can Dietetic Assoc 1988; 49: 23.
Haas JD, Brownlie T . Iron deficiency and reduced work capacity: a critical review of the research to determine a causal relationship. J Nutr 2001; 131: 676S–688S.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pinhas-Hamiel, O., Newfield, R., Koren, I. et al. Greater prevalence of iron deficiency in overweight and obese children and adolescents. Int J Obes 27, 416–418 (2003). https://doi.org/10.1038/sj.ijo.0802224
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ijo.0802224
Keywords
This article is cited by
-
Alterations in glutathione redox homeostasis among adolescents with obesity and anemia
Scientific Reports (2021)
-
Multiple micronutrient supplementation improves micronutrient status in primary school children in Hai Phong City, Vietnam: a randomised controlled trial
Scientific Reports (2021)
-
Nonalcoholic Steatohepatitis Modifies Serum Iron-Related Variables in Patients with Morbid Obesity
Biological Trace Element Research (2021)
-
Prevalence of iron deficiency among university kendo practitioners in Japan: an observational cohort study
Journal of the International Society of Sports Nutrition (2020)
-
Prevalence of Iron deficiency in Lebanese schoolchildren
European Journal of Clinical Nutrition (2020)