Abstract
OBJECTIVE: The main aim of this study was to identify subjects with (1) night eating syndrome (defined as morning anorexia, evening hyperphagia and insomnia) and (2) nocturnal eating syndrome (defined as eating at night after having gone to bed). In the literature the differences and similarities between these two syndromes are not clear.
SUBJECTS: One-hundred and ninety-four obese patients from an academic, clinical obesity unit. Mean BMI (±s.d.) was 40±5 kg/m2, age 44±12 y and 76% were women.
MEASUREMENTS: Questionnaires with multiple choices and open questions along with the Binge Eating Scale.
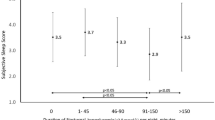
RESULTS: Fourteen percent of the patients met the criteria for night eating and/or nocturnal eating syndrome. Night eating syndrome was manifest in 6% of the patients and nocturnal eating syndrome in 10%. Both the night eaters and the nocturnal eaters had more trouble getting to sleep than the patients without night/nocturnal eating problems (P<0.001 and P<0.01). The nocturnal eaters also had more trouble staying asleep (P<0.001). Morning anorexia was not typically found in nocturnal eaters. Being on long-term sick leave was more common among the nocturnal eaters (P<0.01).
CONCLUSION: Fourteen percent of the patients at our obesity unit met the criteria for night eating and/or nocturnal eating syndrome. There are clear similarities between night eating syndrome and nocturnal eating syndrome, but also differences.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Stunkard AJ, Grace WJ, Wolff HG . The night-eating syndrome Am J Med 1955 19: 78–86.
Stunkard A, Berkowitz R, Wadden T, Tanrikut C, Reiss E, Young L . Binge eating disorder and the night-eating syndrome Int J Obes Relat Metab Disord 1996 20: 1–6.
Adami GF, Meneghelli A, Scopinaro N . Night eating and binge eating disorder in obese patients Int J Eating Disord 1999 25: 335–338.
Kuldau JM, Rand CSW . The night eating syndrome and bulimia in the morbidly obese Int J Eating Disord 1986 5: 143–148.
Rand CSW, Macgregor AMC, Stunkard AJ . The night eating syndrome in the general population and among postoperative obesity surgery patients Int J Eating Disord 1997 22: 65–69.
Rand CSW, Kuldau JM . Eating patterns in normal weight individuals: bulimia, restrained eating, and the night eating syndrome Int J Eating Disord 1986 5: 75–84.
Coates TJ . Successive self-management strategies towards coping with night eating J Behav Ther & Exp Psychiat 1978 9: 181–183.
Birketvedt GS, Florholmen J, Sundsfjord J, Osterud B, Dinges D, Bilker W, Stunkard A . Behavioral and neuroendocrine characteristics of the night eating syndrome JAMA 1999 282: 657–663.
Thorpy MJ (ed) . The international classification of sleep disorders: diagnostic and coding manual American Sleep Disorders Association, Diagnostic Classification Steering Committee Allen Press: Lawrence, KS 1990.
Greeno CG, Wing RR, Marcus MD . Nocturnal eating in binge eating disorder and matched-weight controls Int J Eating Disord 1995 18: 343–349.
Manni R, Ratti MT, Tartara A . Nocturnal eating: prevalence and features in 120 insomniac referrals Sleep 1997 20: 734–738.
Spaggiari MC, Granella F, Parrino L, Marchesi C, Melli I, Terzano MG . Nocturnal eating syndrome in adults Sleep 1994 17: 339–344.
Schenck CH, Hurwitz TD, Bundlie SR, Mahowald MW . Sleep-related eating disorders: polysomnographic correlates of a heterogeneous syndrome distinct from daytime eating disorders Sleep 1991 14: 419–431.
Schenck CH, Mahowald MW . Review of nocturnal sleep-related eating disorders Int J Eating Disord 1994 15: 343–356.
Lennernäs M, Hambraeus L, Åkerstedt T . Shift related dietary intake in day and shift workers Appetite 1995 25: 253–265.
Gormally J, Black S, Daston S, Rardin D . The assessment of binge eating severity among obese persons Addict Behav 1982 7: 47–55.
Adami GF, Meneghelli A, Scopinaro N . Night eating syndrome in individuals with mediterranean eating-style Eating Weight Disord 1997 2: 203–206.
Björk CC, Rössner S . ‘Extravagances’ during weight reduction, an analysis of food preference and selection Appetite 1998 31: 93–99.
Becker W, Enghardt H, Robertson A-K (eds) . Kostundersökningar i Sverige 1950–1990 National Food Administration Wikströms Tryckeri AB: Uppsala 1994 pp 31–37.
Andersson I, Rössner S . Meal patterns in obese and normal weight men: the ‘Gustaf’ study Eur J Clin Nutr 1996 50: 639–646.
Forslund HB, Lissner L, Lindroos AK, Sjöström L . Meal patterns in obese women and in women from a population based study. (Abstract.) Int J Obes Relat Metab Disord 1998 22 (Suppl 3): P125.
Acknowledgements
This study was supported by grants from Resource Center for Eating Disorders.
Author information
Authors and Affiliations
Corresponding author
Eating and Sleeping habit Questionnaire
Eating and Sleeping habit Questionnaire
Rights and permissions
About this article
Cite this article
Cerú-Björk, C., Andersson, I. & Rössner, S. Night eating and nocturnal eating—two different or similar syndromes among obese patients?. Int J Obes 25, 365–372 (2001). https://doi.org/10.1038/sj.ijo.0801552
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ijo.0801552
Keywords
This article is cited by
-
Cardiorenal Metabolic Consequences of Nighttime Snacking: Is it an Innocent Eating Behavior?
Current Nutrition Reports (2022)
-
Assessing established BMI variants for a role in nighttime eating behavior in robustly phenotyped Southwestern American Indians
European Journal of Clinical Nutrition (2020)
-
Binge eating disorder and night eating syndrome in adults with type 2 diabetes: a systematic review
Journal of Eating Disorders (2018)
-
Night eating syndrome: implications for severe obesity
Nutrition & Diabetes (2012)