Abstract
BACKGROUND: Despite the westernized lifestyle, most Japanese are not prominently obese. As their obesity may be obscured, we want to further explore central fat distribution and health risks among this population.
METHODS: 2668 men (body mass index (BMI) 20–<26.4 kg/m2) were identified from 3343 men (BMI 14.0–37.7, median of waist‐to‐height ratio (W/Ht) 0.50) who underwent routine health examinations. They were divided into four groups: (1) BMI 20–<24, W/Ht<0.50; (2) BMI 20–<24, W/Ht≥0.50; (3) BMI 24–<26.4, W/Ht<0.50; and (4) BMI 24–<26.4, W/Ht≥0.50. The metabolic risks and physical activities were compared.
RESULTS: W/Ht≥0.50 comprised 35% of the subjects of BMI 20–<24, 91% of BMI 24–<26.4, only 1% of BMI<20 and up to 99% of BMI≥26.4. After adjusting for age and smoking and with group 1 as the reference group, odds ratios (ORs) were significantly higher in both groups 2 and 4 for the risk of hypertension (1.42, 1.98), hyperglycaemia (1.49, 1.78), hypertriglyceridaemia (1.95, 2.56), low HDL cholesterol (1.87, 2.20), hyperuricaemia (2.00, 2.51) and fatty liver (2.57, 5.64) and additionally in group 4 for hypercholesterolaemia (1.35). ORs in group 3 were only significantly higher for risk of hypertension (1.86) and fatty liver (1.89). Significantly lower frequencies of regular physical activity were noted in the higher W/Ht groups (0.75, 0.47, 1.10, 0.52 days per week, from groups 1–4, respectively).
CONCLUSIONS: Measurement of waist circumference may be a preliminary method for the survey of people at higher risk of lifestyle‐related disorders in Japanese men, especially among those with moderate BMI.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Vague J . The degree of masculine and differentiation of obesities Am J Clin Nutr 1956 4:: 20–34.
Lasson B, Svädsudd K, Welin L, Wilhelmsen L, Bjöntrop P, Tibblin G . Abdominal adipose tissue distribution, obesity, and risk of cardiovascular disease and death: 13 year follow up of participants in the study of men born in 1913 Br Med J 1984 288: 1401–1404.
Fujioka S, Matsuzawa Y, Tokunaga K, Tarui S . Contribution of intra‐abdominal fat accumulation to the impairment of glucose and lipid metabolism in human obesity Metabolism 1987 36: 54–59.
Deprés J‐P . Lipoprotein metabolism in visceral obesity Int J Obes Relat Metab Disord 1991 15: 45–52.
Blair D, Habicht J‐P, Sims EAH, Sklwester D, Abraham S . Evidence for an increased risk for hypertension with centrally located body fat and the effect of race and sex on this risk Am J Epidemiol 1984 119: 526–539.
Kaplan NM . The deadly quartet. Upper‐body obesity, glucose intolerance, hypertriglyceridemia, and hypertension Arch Intern Med 1989 149: 1514–1520.
Pouliot M‐C, Després J‐P, Lemieux S, Moorjani S, Bouchard C, Tremblay A et al.Waist circumference and abdominal saggital diameter. Best simple anthropometric indexes of abdominal visceral adipose tissue accumulation and related cardiovascular risk in men and women Am J Cardiol 1994 73: 460–468.
Lean MEJ, Han TS, Morrison CE . Waist circumference as a measure for indicating need for weight management Br Med J 1995 311: 158–161.
Lean MEJ, Han TS, Seidell JC . Impairment of health and quality of life in people with large waist circumference Lancet 1998 351: 853–856.
Ruderman N, Chisholm D, Pi‐Sunyer Xavier, Schneider S . Perspective in diabetes. The metabolically obese, normal‐weight individuals revised Diabetes 1998 47: 699–713.
Yoshiike Y, Matsumara M, Zaman MM, Yamaguchi M . Descriptive epidemiology of body index in Japanese adults in a representative sample from the National Nutrition Survey 1990–1994 Int J Obes Relat Metab Disord 1995 19:: 585–589.
Kosaka K, Kuzuya T, Yoshinaga H, Hagura R . A prospective study of health check examinees for the development of non‐insulin‐dependent diabetes mellitus: relationship of the incidence of diabetes with the initial insulinogenic index and degree of obesity Diabetic Med 1998 22: 684–687.
Smalley KJ, Knerr AN, Kendrick ZV, Colliver JA, Owen OE . Reassessment of body mass index Am J Clin Nutr 1990 52: 405–408.
Hsieh SD, Yoshinaga H . Abdominal fat distribution and coronary heart disease risk factors in men—waist/height ratio as a simple and useful predictor Int J Obes Relat Metab Disord 1995 19: 585–589.
Hsieh SD, Yoshinaga H . Waist/height ratio as a simple and useful predictor of coronary heart disease risk factors in women Intern Med 1995 34: 1147–1152.
Hsieh SD, Yoshinaga H . Is there any difference in coronary heart disease risk factors and prevalence of fatty liver in subjects with normal body mass index having different physiques? Tohuku J Exp Med 1995 177: 223–231.
Hsieh SD, Yoshinaga H . The relationships between various obesity indices and coronary heart risk factors. The comparisons of waist/height ratio to other obesity indices J Japan Human Dry Dock 1996 11: 26–29 (in Japanese).
Lee JS, Aoki K, Kawakubo K, Gunji A . A study on indices of body fat distribution for screening for obesity J Occup Health 1995 37: 9–18.
Ashwell M, Lejeune S, McPherson K . Ratio of waist circumference to height may be better indicator of need for weight management Br Med J 1996 312: 377.
Cox BD, Whichelow MJ, Ashwell M, Prevost AT, Lejeune SRE . Association of anthropometric indices with elevated blood pressure in British adults Int J Obes Relat Metab Disord 1997 21: 674–680.
Ashwell M, Cole TJ, Dixon AK . Ratio of waist circumference to height is a strong predictor of intra‐abdominal fat Br Med J 1996 313: 559–560.
Japan Society for the Study of Obesity . Obesity: the guidance of diagnosis and treatment. Ishiyaku: Tokyo, 1993, p18 (in Japanese).
Hsieh SD, Yoshinaga H, Muto T, Sakurai Y . Regular physical activity and coronary risk factors in Japanese men Circulation 1998 97: 661–665.
National Center for Health Statistics and National Center for Chronic Disease Prevention and Health Promotion . Update: prevalence of overweight among children, adolescent and adults‐United States, 1988–1994 JAMA 1997 277 (14): 1111.
National Institutes of Health Consensus Development Panel on the Health Implications of Obesity . Health implications of obesity, national institutes of health consensus development conference statement Ann Intern Med 1985 103 (6 pt 2): 1073–1077.
Weinsier RL, Norris DJ, Birch R, Bernstein RS, Wang J, Yang M‐U et al.The relative contribution of body fat and fat pattern to blood pressure level Hypertension 1985 7: 578–585.
Waaler Ht . Height, weight and mortality—the Norwegian experience Acta Med Scand 1984 679 (Suppl): 1–56.
Hebert PR, Rich‐Ewards JW, Manson JE, Ridker PM, Cook NR, O'Connor GT et al.Height and incidence of cardiovascular disease in male physicians Circulation 1993 88 (part 1): 1437–1443.
Parker DR, Lapane KL, Lasater TM, Carleton RA . Short stature and cardiovascular disease among men and women from two southeastern New England communities Int J Epidemiol 1998 27: 970–975.
Acknowledgements
We thank Mitsui Chemical Industries Ltd, for their financial assistance in this study and Miss Miyuki Suzuki for her secretarial assistance in the preparation of this manuscript.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Hsieh, S., Yoshinaga, H., Muto, T. et al. Health risks among Japanese men with moderate body mass index. Int J Obes 24, 358–362 (2000). https://doi.org/10.1038/sj.ijo.0801157
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ijo.0801157
Keywords
This article is cited by
-
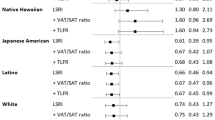
Ethnic Disparities in Blood Pressure: A Population-based Study
Journal of Immigrant and Minority Health (2017)
-
High prevalence of overweight, obesity, and hypertension with increased risk to cardiovascular disorders among adults in northwest Ethiopia: a cross sectional study
BMC Cardiovascular Disorders (2014)
-
Association between body fat distribution and androgen deficiency in middle-aged and elderly men in China
International Journal of Impotence Research (2014)
-
Waist-to-height ratio, waist circumference, and body mass index as indices of cardiometabolic risk among 36,642 Taiwanese adults
European Journal of Nutrition (2013)
-
Waist to height ratio for recording the risks of overweight in schoolchildren in Kerala
Indian Pediatrics (2013)