Abstract
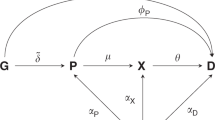
Biomedical researchers usually test the null hypothesis that there is no difference of the population mean of pharmacokinetics (PK) parameters between genotypes by the Kruskal–Wallis test. Although a monotone increasing pattern with a number of alleles is expected for PK-related genes, the Kruskal–Wallis test does not consider a monotonic response pattern. For detecting such patterns in clinical and toxicological trials, a maximum contrast method has been proposed. We show how that method can be used with pharmacogenomics data to a develop test of association. Further, using simulation studies, we compare the power of the modified maximum contrast method to those of the maximum contrast method and the Kruskal–Wallis test. On the basis of the results of those studies, we suggest rules of thumb for which statistics to use in a given situation. An application of all three methods to an actual genome-wide pharmacogenomics study illustrates the practical relevance of our discussion.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Licinio J, Wong M . Pharmacogenomics: The Search for Individualized Therapies. Wiley: Weinheim (Germany), 2002.
Evans WE, McLeod HL . Pharmacogenomics—drug disposition, drug targets, and side effects. N Engl J Med 2003; 348: 538–549.
Ingelman-Sundberg M . Pharmacogenomic biomarkers for prediction of severe adverse drug reactions. N Engl J Med 2008; 358: 637–639.
Efferth T, Volm M . Pharmacogenetics for individualized cancer chemotherapy. Pharmacol Ther 2005; 107: 155–176.
US FDA. Guidance for Industry Pharmacogenomic Data Submissions. 2005.
International Human Genome Sequencing Consortium. Finishing the euchromatic sequence of the human genome. Nature 2004; 431: 931–945.
Risch N, Merikangas K . The future of genetic studies of complex human diseases. Science 1996; 273: 1516–1517.
Hirschhorn JN, Daly MJ . Genome-wide association studies for common diseases and complex traits. Nat Rev Genet 2005; 6: 95–108.
Kingsmore SF, Lindquist IE, Mudge J, Gessler DD, Beavis WD . Genome-wide association studies: progress and potential for drug discovery and development. Nat Rev Drug Discov 2008; 7: 221–230.
Kruskal HW, Wallis WA . Use of ranks in one-criterion variance analysis. J Am Stat Assoc 1952; 47: 583–621.
Siegel S, Castellan NJ . Nonparametric Statistics for the Behavioral Sciences, 2nd edn. McGraw-Hill: New York, 1988.
Mukerjee H, Robertson T, Wright FT . Comparison of several treatments with a control using multiple contrast. J Am Stat Assoc 1987; 82: 902–910.
Ruberg SJ . Contrasts identifying the minimum effective dose. J Am Stat Assoc 1989; 82: 816–822.
Yoshimura I, Wakana A, Hamada C . A performance comparison of maximum contrast methods to detect dose dependency. Drug Inf J 1997; 31: 423–432.
Stewart H, Ruberg SJ . Detecting dose response with contrasts. Stat Med 2000; 19: 913–921.
Nishiyama H, Yanagihara H, Yoshimura I . SAS/IML program for computing probabilities related to maximum contrast methods. Jpn J Biometrics 2003; 24: 57–70, (in Japanese).
Wakana A, Yoshimura I, Hamada C . A method for therapeutic dose selection in a phase II clinical trial using contrast statistics. Stat Med 2007; 26: 498–511.
Jeunemaitre X, Soubrier F, Kotelevtsev YV, Lifton RP, Williams CS, Charru A et al. Molecular basis of human hypertension: role of angiotensinogen. Cell 1992; 71: 169–180.
Caulfield M, Lavender P, Farrall M, Munroe P, Lawson M, Turner P et al. Linkage of the angiotensinogen gene to essential hypertension. N Engl J Med 1994; 330: 1629–1633.
Hegele RA, Brunt JH, Connelly PW . A polymorphism of the angiotensinogen gene associated with variation in blood pressure in a genetic isolate. Circulation 1994; 90: 2207–2212.
Vasku A, Soucek M, Znojil V, Rihacek I, Tschoplova S, Strelcova L et al. Angiotensin I-converting enzyme and angiotensinogen gene interaction and prediction of essential hypertension. Kidney Int 1998; 53: 1479–1482.
Pereira TV, Nunes AC, Rudnicki M, Yamada Y, Pereira AC, Krieger JE . Meta-analysis of the association of 4 angiotensinogen polymorphisms with essential hypertension: a role beyond M235T? Hypertension 2008; 51: 778–783.
Pei Y, Scholey J, Thai K, Suzuki M, Cattran D . Association of angiotensinogen gene T235 variant with progression of immunoglobulin A nephropathy in Caucasian patients. J Clin Invest 1997; 100: 814–820.
Genz A, Bretz F . Numerical computation of multivariate t-probabilities with application to power calculation of multiple contrasts. J Stat Comput Simulat 1999; 63: 361–378.
Westfall PH, Young SS . Resampling-Based Multiple Testing: Examples and Methods for P-value Adjustment. Wiley: New York, 1993.
Gabrielsson J, Weiner D . Pharmacokinetic and Pharmacodynamic Data Analysis: Concepts and Applications. Taylor & Francis: Sweden, 2000.
Sugiyama E, Kaniwa N, Kim SR, Kikura-Hanajiri R, Hasegawa R, Maekawa K et al. Pharmacokinetics of gemcitabine in Japanese cancer patients: the impact of a cytidine deaminase polymorphism. J Clin Oncol 2007; 25: 32–42.
Acknowledgements
We thank Professor Isao Yoshimura and Professor Chikuma Hamada at Tokyo University of Science for their valuable advice, and Dr Hiromi Sakamoto and Ms Sumiko Ohnami for the SNP genotyping. Yasunori Sato is a recipient of Official Trainee of the Foreign Clinical Pharmacology Training Program, Japanese Society of Clinical Pharmacology and Therapeutics. This work was initiated while Yasunori Sato was a postdoctoral fellow at the Department of Biostatistics, Harvard School of Public Health, and partially supported in Japan by the program for promotion of Fundamental Studies in Health Sciences of the National Institute of Biomedical Innovation (NiBio).
Author information
Authors and Affiliations
Corresponding author
Additional information
Duality of Interest
None declared.
Rights and permissions
About this article
Cite this article
Sato, Y., Laird, N., Nagashima, K. et al. A new statistical screening approach for finding pharmacokinetics-related genes in genome-wide studies. Pharmacogenomics J 9, 137–146 (2009). https://doi.org/10.1038/tpj.2008.17
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/tpj.2008.17